Highlights
The integration of the CYTOscore—comprising baseline levels of IL-8, CCL3, and CCL4—successfully stratifies patients with locally advanced esophageal squamous cell carcinoma (ESCC) into high- and low-risk groups for survival and treatment response.
Patients categorized as low-risk by CYTOscore exhibited a significantly higher complete response (CR) rate (66% vs 35% in the discovery cohort) and dramatically improved overall survival (HR 0.31) and progression-free survival (HR 0.33).
Multi-omics analysis linked the low-risk CYTOscore phenotype to enriched interferon-gamma and interferon-alpha signaling within B cells, suggesting a specific immunological microenvironment conducive to successful chemoradiotherapy and anti-PD-1 synergy.
A validated nomogram incorporating the CYTOscore provides clinicians with a robust predictive tool, achieving AUCs of 0.77, 0.78, and 0.76 for 1-, 2-, and 3-year overall survival, respectively.
Background: The Challenge of Locally Advanced ESCC
Esophageal squamous cell carcinoma (ESCC) remains one of the most aggressive malignancies of the gastrointestinal tract, particularly in East Asian populations. For patients with locally advanced disease, the standard of care has traditionally revolved around neoadjuvant chemoradiotherapy (nCRT) followed by surgery or definitive chemoradiotherapy (dCRT). While the introduction of immune checkpoint inhibitors, specifically anti-PD-1 antibodies like toripalimab, has revolutionized the treatment landscape, therapeutic response remains heterogeneous.
A significant unmet medical need exists for reliable, non-invasive biomarkers that can identify which patients will achieve a complete response and long-term survival. While tissue-based biomarkers like PD-L1 expression or tumor mutational burden (TMB) offer some insight, they are often limited by intratumoral heterogeneity and the invasiveness of repeated biopsies. Serum cytokines, which reflect the systemic inflammatory state and the tumor microenvironment (TME), present a promising alternative for real-time monitoring and prognosis.
Study Design: A Multicenter Exploratory and Validation Approach
In a comprehensive study published in the Journal for ImmunoTherapy of Cancer, researchers conducted exploratory analyses on 81 patients with ESCC derived from two phase II clinical trials. These patients were treated with a combination of chemoradiotherapy and toripalimab (an anti-PD-1 antibody). To ensure the robustness of their findings, the investigators validated the results in an independent prospective cohort consisting of 61 patients.
The methodology was rigorous: the team assessed 19 different serum cytokines at baseline, during treatment, and post-treatment. Beyond clinical data, the researchers employed multi-omics profiling, including RNA sequencing (RNA-seq), whole-exome sequencing (WES), and spatial transcriptomics, to bridge the gap between systemic cytokine levels and the cellular architecture of the tumor microenvironment.
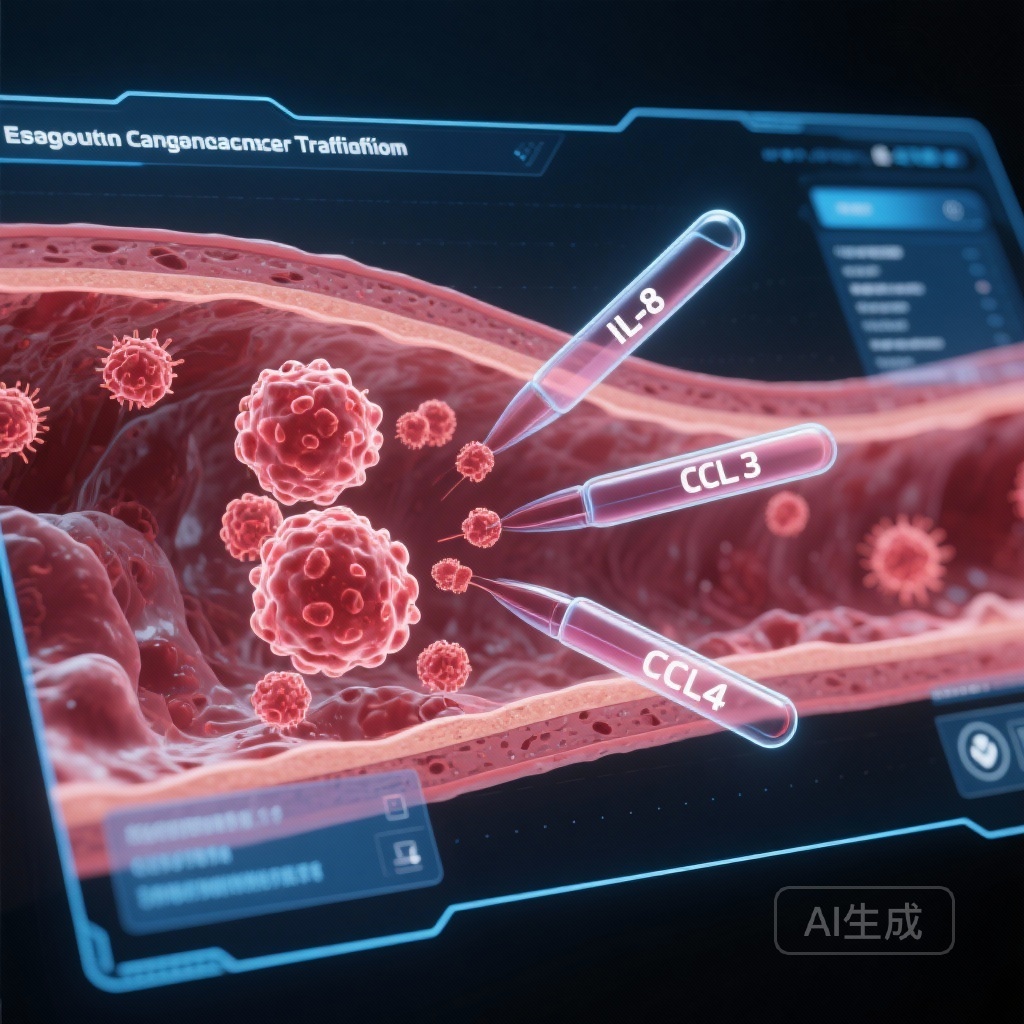
Constructing the CYTOscore: IL-8, CCL3, and CCL4
Using Cox proportional hazards analysis, the research team identified three cytokines—Interleukin-8 (IL-8), C-C motif chemokine ligand 3 (CCL3), and C-C motif chemokine ligand 4 (CCL4)—as the most significant predictors of clinical outcomes. These three markers were used to construct a cytokine-based risk score model, termed the CYTOscore.
IL-8 (CXCL8)
Often associated with pro-angiogenic and pro-inflammatory pathways, high levels of IL-8 have been implicated in promoting tumor progression and resistance to immunotherapy by recruiting myeloid-derived suppressor cells (MDSCs) to the TME.
CCL3 and CCL4
These chemokines are traditionally involved in the recruitment of various immune cells, including T cells and NK cells. However, their systemic levels in the context of ESCC treatment appear to provide a nuanced snapshot of the patient’s immune fitness and the systemic inflammatory response to the combined CRT and immunotherapy regimen.
Key Findings: Survival and Response Stratification
The primary utility of the CYTOscore lies in its ability to stratify patients into low-risk and high-risk categories based on their baseline cytokine profiles. In the discovery cohort, the differences were stark.
Patients in the low-risk CYTOscore group demonstrated a 66% complete response (CR) rate, compared to only 35% in the high-risk group (p=0.014). This clinical response translated directly into survival benefits. The hazard ratio (HR) for overall survival (OS) was 0.31 (95% CI, 0.16-0.62; p=0.00045), and the HR for progression-free survival (PFS) was 0.33 (95% CI, 0.17-0.62; p=0.00036). These figures indicate that low-risk patients had a nearly 70% reduction in the risk of death or disease progression compared to their high-risk counterparts.
Validation and Predictive Accuracy
Scientific findings are only as strong as their reproducibility. The CYTOscore was put to the test in an external, independent cohort of 61 patients. The results were consistent: the low-risk group in the validation cohort achieved a 66% CR rate versus 27% in the high-risk group (p=0.039). Survival analysis in this cohort also favored the low-risk group (HR 0.30 for OS, 95% CI 0.09-0.99, p=0.045).
To enhance the clinical utility of these findings, the researchers developed a nomogram that integrates the baseline CYTOscore with standard clinical characteristics. The predictive accuracy of this nomogram was impressive, with an Area Under the Curve (AUC) of 0.77 for 1-year, 0.78 for 2-year, and 0.76 for 3-year OS. This suggests that the CYTOscore adds significant prognostic value beyond traditional clinical staging and patient characteristics.
Mechanistic Insights: The Role of B Cells and Interferon Signaling
Perhaps the most compelling aspect of this research is the attempt to explain why these cytokines predict response. Multi-omics analysis of the tumor microenvironment revealed that patients in the low-risk category had an enrichment of interferon-gamma (IFN-γ) and interferon-alpha (IFN-α) signaling pathways. Interestingly, these pathways were specifically upregulated in B cells within the tumor.
While much of the focus in immunotherapy research has been on T cells, this study highlights the critical role of B cells in the anti-tumor immune response. The presence of IFN-signaling enriched B cells may indicate the formation of tertiary lymphoid structures (TLS), which are increasingly recognized as hubs for the generation of robust and sustained anti-tumor immunity.
Expert Commentary: Moving Toward Precision Immunotherapy
The development of the CYTOscore represents a significant step forward in the management of ESCC. Unlike many experimental biomarkers, serum cytokines are relatively easy to measure using standardized multiplex assays, making the CYTOscore a viable candidate for integration into routine clinical practice.
However, clinicians should interpret these results with a degree of caution. While the validation cohort provided support, these findings originate from phase II trials. Larger, phase III randomized controlled trials are necessary to confirm whether the CYTOscore can be used not just for prognosis, but for therapeutic decision-making—such as identifying high-risk patients who might require more intensive regimens or alternative immunotherapy combinations.
Furthermore, the biological interplay between systemic cytokines and the local tumor environment remains complex. The finding that IL-8, CCL3, and CCL4 are the primary drivers suggests that the balance between pro-tumor inflammation and anti-tumor recruitment is the key determinant of success in the CRT plus anti-PD-1 setting.
Conclusion
The CYTOscore, based on baseline levels of IL-8, CCL3, and CCL4, offers a potent and non-invasive means of predicting response and survival in patients with ESCC receiving chemoradiotherapy and anti-PD-1 antibody treatment. By identifying patients who are unlikely to respond to the standard combination, this score may allow for the early exploration of alternative strategies, ultimately moving the field closer to the goal of personalized, precision oncology for esophageal cancer.
References
Chen B, Chen J, Wang S, et al. Serum cytokines predict response and survival in esophageal squamous cell carcinoma receiving chemoradiotherapy combined with anti-PD-1 antibody: analyses of two phase II clinical trials. J Immunother Cancer. 2026;14(1):e013065. doi:10.1136/jitc-2025-013065.