Highlights
- Physiology-guided complete revascularization reduces the 3-year risk of death, MI, stroke, or ischemia-driven revascularization in older patients (≥75 years) compared to culprit-only strategies.
- The clinical benefit of complete revascularization is consistent across the spectrum of renal function, including patients with an eGFR <60 mL/min/1.73 m2.
- Despite higher baseline risks, patients with chronic kidney disease (CKD) did not experience a higher rate of contrast-associated acute kidney injury (CA-AKI) with the complete revascularization strategy compared to the culprit-only approach.
- These findings suggest that advanced age and renal impairment should not be automatic barriers to comprehensive multivessel intervention in the setting of myocardial infarction.
Introduction: The Intersection of Aging, Renal Impairment, and Ischemic Heart Disease
The management of older patients presenting with myocardial infarction (MI) and multivessel coronary artery disease (MVD) remains one of the most complex challenges in contemporary interventional cardiology. This demographic is characterized by a high prevalence of comorbidities, most notably chronic kidney disease (CKD), which significantly complicates both the prognosis and the therapeutic decision-making process. Historically, older patients and those with renal impairment have been underrepresented in large-scale randomized controlled trials, leading to a ‘treatment paradox’ where the highest-risk individuals are often the least likely to receive evidence-based, intensive therapies.
The primary concern regarding complete revascularization in this population is twofold: the perceived increased risk of procedural complications and the fear of contrast-associated acute kidney injury (CA-AKI). However, leaving non-culprit lesions untreated may leave the patient vulnerable to future ischemic events, which are particularly poorly tolerated in the elderly. The FIRE (Functional Assessment in Elderly MI Patients with Multivessel Disease) trial was designed to address this gap, and this specific sub-analysis explores whether the benefits of a physiology-guided complete revascularization strategy are maintained across different strata of renal function.
The FIRE Trial: Assessing Physiology-Guided Revascularization
Study Population and Methodology
The FIRE trial was a multicenter, randomized, prospective study that enrolled 1,445 patients aged 75 years or older who presented with either ST-segment elevation myocardial infarction (STEMI) or non-ST-segment elevation myocardial infarction (NSTEMI) and had multivessel disease. Multivessel disease was defined as at least one non-culprit lesion with ≥50% diameter stenosis in a vessel with a diameter of at least 2.5 mm.
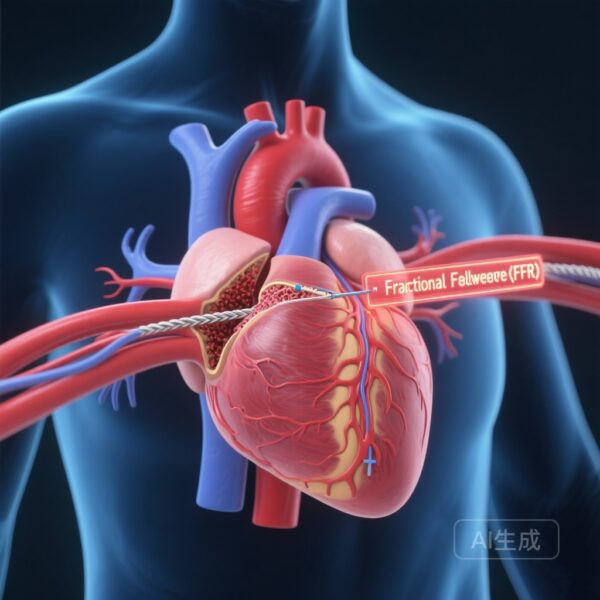
Patients were randomized in a 1:1 ratio to receive either culprit-only revascularization or physiology-guided complete revascularization. In the complete revascularization arm, all non-culprit lesions were assessed using fractional flow reserve (FFR) or non-hyperemic pressure ratios (NHPR). Revascularization was performed only if the physiology assessment indicated functional significance (FFR ≤0.80 or NHPR ≤0.89).
For this sub-analysis, the cohort was stratified by baseline renal function using the estimated glomerular filtration rate (eGFR), calculated via the CKD-EPI formula. The primary threshold for stratification was set at 60 mL/min/1.73 m2, distinguishing those with significant renal impairment from those with relatively preserved function.
Key Results: Consistent Efficacy Across the Renal Spectrum
Renal Function as a Prognostic Marker
Among the 1,445 patients, 662 (45.8%) had a baseline eGFR <60 mL/min/1.73 m2. As expected, renal impairment was a powerful predictor of adverse outcomes. The primary endpoint—a composite of death, MI, stroke, or ischemia-driven revascularization at 3 years—occurred in 33.5% of patients with eGFR <60 compared to 20.3% in those with eGFR ≥60. After adjusting for potential confounders, a lower eGFR remained independently associated with a 42% increase in the risk of the primary endpoint (adjusted HR: 1.42; 95% CI: 1.15-1.76; P < 0.001).
Impact of Complete Revascularization
The core finding of this sub-analysis is that the benefit of physiology-guided complete revascularization was consistent regardless of the patient’s baseline renal function. For patients with eGFR <60 mL/min/1.73 m2, the complete revascularization strategy reduced the risk of the primary endpoint by 32% (HR: 0.68; 95% CI: 0.52-0.89). In patients with eGFR ≥60 mL/min/1.73 m2, the reduction was 20% (HR: 0.80; 95% CI: 0.59-1.10).
Crucially, the interaction analysis (P-interaction > 0.42) confirmed that renal function did not modify the treatment effect. Whether analyzed as a categorical variable or a continuous range, the hazard ratio for complete versus culprit-only revascularization remained stable, favoring the more comprehensive approach. Because patients with CKD have a higher baseline absolute risk, they may actually derive a greater absolute clinical benefit (number needed to treat) from complete revascularization compared to their counterparts with normal renal function.
Safety Analysis: The Specter of Contrast-Associated Acute Kidney Injury
One of the most significant barriers to performing multivessel PCI in older patients is the fear of inducing CA-AKI due to increased contrast volume. In this study, CA-AKI (defined by KDIGO criteria) occurred in 17% of the total population. While the incidence of CA-AKI increased progressively with more advanced stages of CKD (P < 0.001), there was no significant difference in CA-AKI rates between the complete revascularization arm and the culprit-only arm (HR: 1.11; 95% CI: 0.87-1.43).
This finding is pivotal. It suggests that when revascularization is guided by physiology—thereby ensuring that only functionally significant lesions are treated—the additional contrast required for non-culprit intervention does not translate into a clinically significant increase in renal injury, even in a vulnerable geriatric population.
Expert Commentary: Navigating the Treatment Paradox
Mechanistic Insights and Biological Plausibility
The results of the FIRE trial sub-analysis provide a robust rebuttal to the practice of ‘renal nihilism’ in the cath lab. The efficacy of complete revascularization in CKD patients likely stems from the reduction of the total ischemic burden. Patients with CKD often have more diffuse, calcified, and complex coronary anatomy; by identifying and treating functionally significant non-culprit lesions, clinicians can improve overall myocardial perfusion and reduce the likelihood of subsequent events that the patient’s fragile physiological reserve might not survive.
Furthermore, the use of physiology-guided assessment is a key component of this success. By utilizing FFR or NHPR, operators can avoid performing unnecessary angioplasty on lesions that appear stenotic on angiography but are not causing ischemia. This ‘less is more’ approach within a ‘complete’ revascularization strategy minimizes procedural time and contrast use while maximizing clinical gain.
Clinical Implications for the Heart-Kidney Team
These data reinforce the importance of a multidisciplinary approach. Rather than avoiding revascularization, the focus should be on optimizing the procedure. This includes meticulous hydration protocols, the use of low-osmolar or iso-osmolar contrast media, and potentially the integration of intravascular imaging to further reduce contrast volume. The FIRE trial suggests that the cardiovascular benefits of preventing future MI and death far outweigh the transient and often reversible risks associated with the procedure itself.
Conclusion: Shifting the Paradigm in Geriatric Cardiology
The FIRE trial sub-analysis provides high-quality evidence that physiology-guided complete revascularization is both safe and effective for older patients with MI and multivessel disease, regardless of their renal function. Kidney function remains a potent prognostic factor, but it should not serve as a contraindication to a complete revascularization strategy. In fact, given the high absolute risk of MACE in the CKD population, these patients stand to gain the most from a comprehensive interventional approach.
Future guidelines should reflect these findings, encouraging clinicians to move beyond age- and organ-based discrimination and instead utilize functional assessment to provide the most effective care for this growing and complex patient population.
References
- Cantone A, Verardi FM, Vadalà G, et al. Renal Function-Stratified Comparison of Complete vs Culprit-Only Revascularization in Older Patients With Myocardial Infarction and Multivessel Disease. JACC Cardiovasc Interv. 2025 Dec 8;18(23):2849-2859. doi: 10.1016/j.jcin.2025.09.019.
- Biscaglia S, et al. Physiology-Guided Complete vs Culprit-Only Revascularization in Elderly Patients with Myocardial Infarction: The FIRE Trial. N Engl J Med. 2023.
- Mehran R, et al. Contrast-Associated Acute Kidney Injury. N Engl J Med. 2019;380(22):2146-2155.
- Stone GW, et al. Complete Revascularization in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Disease. J Am Coll Cardiol. 2019.