Highlights
- A large-scale cluster-randomized trial of 1,507 patients found no significant reduction in high opioid use when combining PECS I blocks with either paravertebral or serratus anterior plane blocks compared to paravertebral block alone.
- Primary outcomes showed a non-significant 1.9% difference in opioid consumption rates between combined block groups and the paravertebral block group.
- Secondary outcomes, including pain scores, antiemetic requirements, and quality of recovery, were comparable across all study arms.
- The results suggest that clinicians can choose between these regional techniques based on institutional expertise, patient anatomy, and safety profiles without compromising analgesic efficacy.
Background: The Challenge of Post-Mastectomy Pain
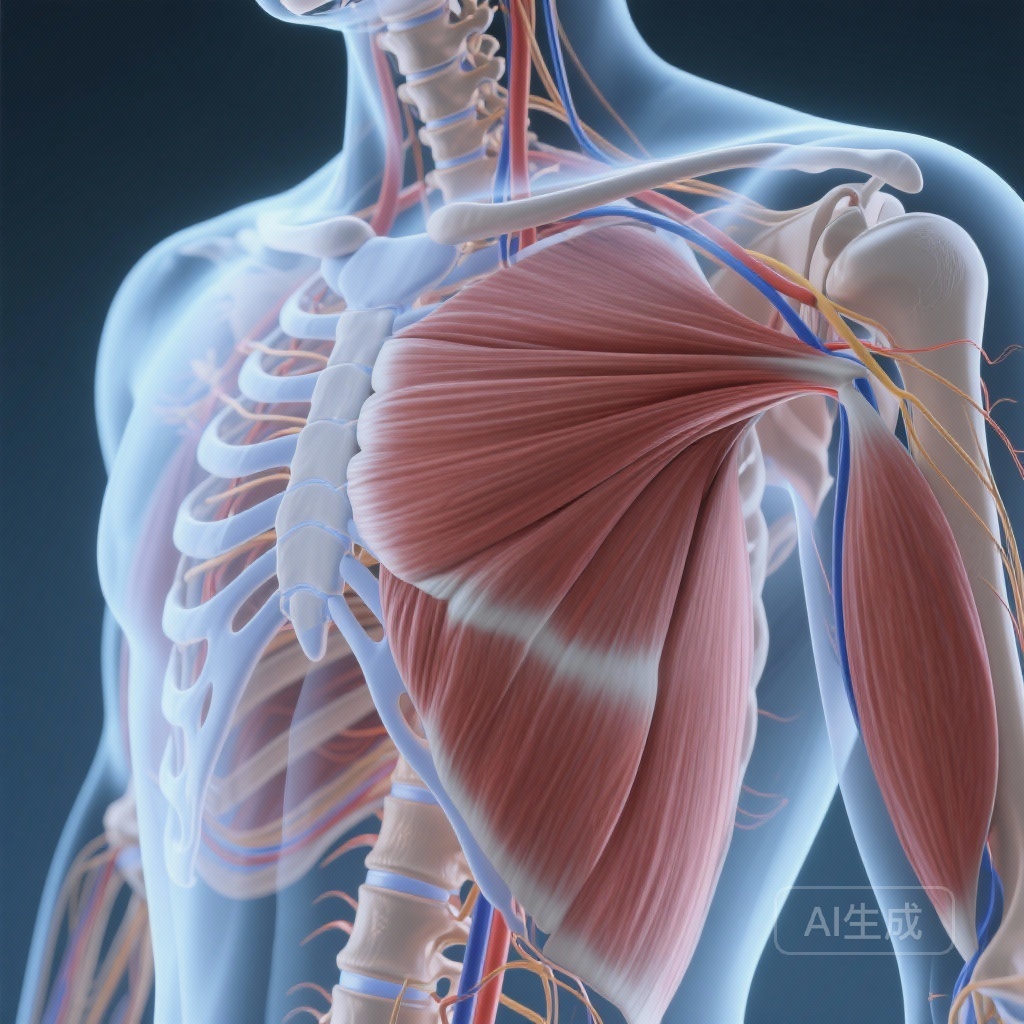
Postoperative pain management for mastectomy with immediate reconstruction remains a critical challenge in oncological surgery. The procedure, which involves extensive tissue dissection and often the placement of subpectoral expanders, is associated with significant acute pain and a risk of developing chronic post-surgical pain syndromes. Effective regional anesthesia is the cornerstone of a multimodal analgesic strategy, aimed at reducing the reliance on systemic opioids and facilitating early recovery.
Traditionally, the thoracic paravertebral block (PVB) has been considered the gold standard for breast surgery due to its ability to provide dense, dermatomal anesthesia. However, the emergence of fascial plane blocks, such as the Pecs blocks (PECS I and II) and the serratus anterior plane block (SAPB), has offered alternative, potentially easier-to-perform ultrasound-guided techniques. Despite their popularity, high-quality evidence comparing these techniques—especially in the context of combination approaches for complex reconstructive cases—has been sparse. The hypothesis that ‘more is better’—specifically, that adding an interpectoral (PECS I) block to target the pectoral nerves would improve outcomes for subpectoral reconstruction—required rigorous testing.
Study Design: A Clinically Integrated Cluster-Randomized Approach
The study by Tokita et al., published in Anesthesiology, utilized a robust cluster-randomized, clinically integrated trial design at a single high-volume cancer center. The trial enrolled 1,507 patients undergoing bilateral mastectomy with immediate expander reconstruction between 2019 and 2023. To minimize clinician bias and streamline workflow, randomization was conducted by month (cluster randomization).
Patients were assigned to one of three groups:
- Paravertebral block (PVB) alone.
- Paravertebral block plus PECS I block (PVB + PECS I).
- Serratus anterior plane block plus PECS I block (SAPB + PECS I).
The primary outcome was the incidence of ‘high postoperative opioid use,’ defined as the upper quartile of consumption. Secondary outcomes were comprehensive, including postoperative pain scores, use of antiemetics, time to discharge, adverse events, chronic pain at follow-up, and patient-reported quality of recovery scores.
Key Findings: No Superiority in Combined Approaches
The results of the trial were definitive in their lack of a significant difference between the studied techniques. Out of the 1,507 patients, 492 received PVB, 446 received PVB + PECS I, and 568 received SAPB + PECS I. The primary analysis compared the combined block groups (PVB + PECS I and SAPB + PECS I) collectively against the PVB-only group.
Primary Outcome: Opioid Consumption
The rates of high postoperative opioid use were 26% for PVB, 27% for PVB + PECS I, and 22% for SAPB + PECS I. When comparing the combined groups to the PVB group, the difference was a mere 1.9% lower rate in the combination arm, which was not statistically significant (95% CI, -2.7% to 6.5%; P = 0.4). This indicates that the addition of a PECS I block did not provide the synergistic opioid-sparing effect that many clinicians had hypothesized.
Secondary Outcomes and Safety
Analysis of secondary endpoints reinforced the primary finding. There were no statistically significant differences in pain scores across various time points, nor were there differences in the need for rescue antiemetics or the speed of discharge. Furthermore, long-term outcomes such as chronic pain and patient-reported quality of recovery metrics showed no benefit for one technique over the others. Safety profiles were excellent across all groups, with no significant increase in adverse events associated with the additional needle passes required for combination blocks.
Expert Commentary: Interpreting the Neutral Result
The failure to demonstrate superiority for combined blocks in this trial provides essential clarity for the anesthesia community. Several factors may explain why the addition of a PECS I block did not improve outcomes. First, the thoracic paravertebral block provides a broad sensory block that may already cover the necessary dermatomes, even in the presence of subpectoral expanders. Second, the use of a robust multimodal analgesic regimen (e.g., acetaminophen, NSAIDs, gabapentinoids) likely creates a ‘ceiling effect,’ where the incremental benefit of an additional regional technique becomes negligible.
From a methodological perspective, this study is a landmark for regional anesthesia research. The use of a cluster-randomized, clinically integrated design allowed for a massive sample size that would be difficult to achieve with individual randomization. This ensures that the results are highly generalizable to real-world clinical practice in high-volume surgical centers.
However, limitations must be noted. As a single-center study, the results reflect the expertise and specific protocols of that institution. Additionally, while the study focused on expander reconstruction, the findings might differ in patients undergoing different types of reconstruction or in those with pre-existing chronic pain conditions.
Conclusion: Clinical Implications for Regional Anesthesia
The Tokita et al. trial confirms that PVB, PVB + PECS I, and SAPB + PECS I are all acceptable and effective regional anesthetic techniques for mastectomy with reconstruction. The lack of superiority for the more complex combination blocks suggests that clinicians should prioritize the block they are most comfortable performing and the one that presents the lowest risk for the specific patient.
For institutions where PVB is standard practice, there is no evidence-based reason to routinely add a PECS I block. Conversely, for clinicians who prefer the safety profile or ease of ultrasound visualization offered by SAPB or PECS blocks, these remain viable alternatives to PVB. The focus of future research should perhaps shift from the specific ‘type’ of block to the optimization of multimodal pathways and the identification of patient subsets who may benefit from more intensive interventions.
Funding and Trial Information
This study was conducted at Memorial Sloan Kettering Cancer Center. The trial is registered at ClinicalTrials.gov under the identifier NCT04016376. No specific external funding conflicts were reported that would bias the interpretation of these results.
References
- Tokita HK, Assel MJ, Serafin J, et al. Paravertebral or Serratus Anterior Plane Block Combined with Interpectoral Blocks versus Paravertebral Block for Mastectomy: A Cluster-randomized Trial of 1,507 Patients. Anesthesiology. 2026;144(2):379-389.
- Bashandy GM, Abbas DN. Pectoral nerves I and II block in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(1):68-74.
- Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59(9):470-475.