Highlights
1. In a multicenter prospective study of 1,351 patients, circumferential aneurysm wall enhancement (AWE) on gadolinium-enhanced 3-T MRI was associated with a 36.8% absolute cumulative risk of instability (growth or rupture) over four years.
2. UIAs with circumferential AWE exhibited a significantly higher risk of instability compared to those with focal AWE (17.2%) or no AWE (11.4%).
3. After adjusting for traditional risk factors such as size ratio, location, and shape, circumferential AWE remained an independent predictor of instability with an adjusted hazard ratio of 2.21.
4. These findings support the integration of MRI vessel wall imaging (VWI) into routine clinical workflows to identify high-risk unruptured intracranial aneurysms that may require more aggressive intervention.
Background and Clinical Context
The management of unruptured intracranial aneurysms (UIAs) remains one of the most challenging dilemmas in neurosurgery and interventional neuroradiology. While the prevalence of UIAs in the general population is estimated at approximately 3%, only a small fraction will ever rupture. However, the consequences of subarachnoid hemorrhage (SAH) are devastating, with high rates of mortality and long-term morbidity. Historically, clinicians have relied on morphological and demographic factors—codified in scoring systems like PHASES or ELAPSS—to estimate rupture risk. These factors include aneurysm size, location, patient age, and history of previous SAH.
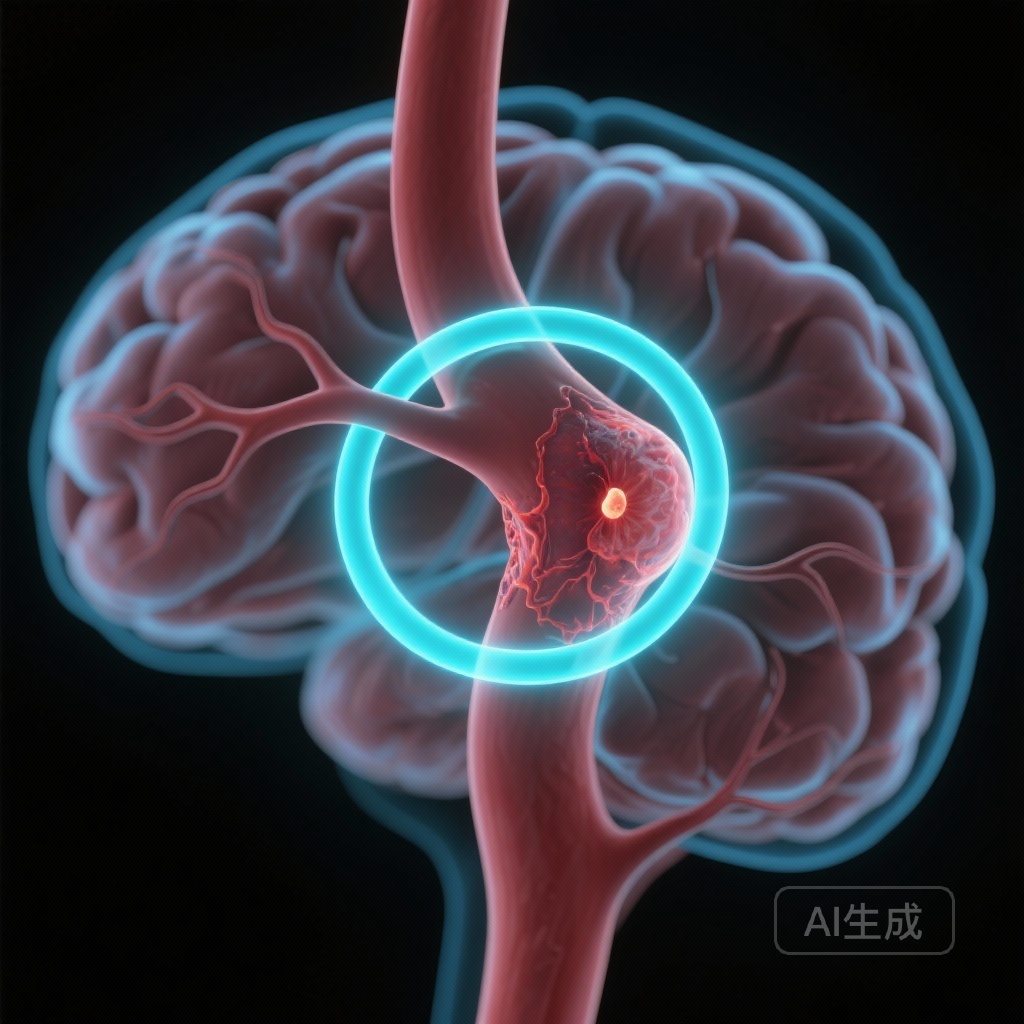
However, morphology alone often fails to capture the biological activity within the aneurysm wall. Emerging evidence suggests that chronic inflammation, atherosclerosis, and vasa vasorum proliferation within the aneurysm wall are the true drivers of instability. Gadolinium-enhanced magnetic resonance imaging (MRI) of the aneurysm wall, also known as vessel wall imaging (VWI), has emerged as a promising non-invasive tool to visualize these pathological processes. While early retrospective and small-scale longitudinal studies suggested that aneurysm wall enhancement (AWE) correlates with instability, the lack of large-scale, long-term prospective data has limited its adoption into standard clinical guidelines. The study by Liu et al., published in JAMA Neurology, addresses this gap by providing robust evidence on the predictive value of AWE over a four-year period.
Study Design and Methodology
This study utilized individual patient data from three prospective multicenter cohort studies conducted across 83 centers in China between January 2017 and December 2024. The inclusion criteria targeted patients aged 18 to 75 years with at least one asymptomatic, saccular UIA measuring 3 mm or greater. A total of 1,453 patients underwent baseline 3-T MRI with gadolinium-enhanced aneurysm wall imaging and computed tomography angiography (CTA). After excluding patients lost to follow-up or those with low-quality imaging, the final analysis included 1,351 patients with 1,416 UIAs, representing 4,884 aneurysm-years of follow-up.
The primary exposure was the pattern of AWE at baseline, categorized into three groups: circumferential AWE (enhancement involving the entire wall), focal AWE (partial enhancement), and no AWE. The primary outcome measure was aneurysm instability, defined as either documented growth (an increase in any dimension of 1 mm or more) or spontaneous rupture. Follow-up was conducted using CTA to assess for these changes. The researchers employed Kaplan-Meier estimates to determine absolute risk and Cox proportional hazards regression to calculate hazard ratios (HRs), adjusting for known confounders such as size ratio, aneurysm location, shape (regular vs. irregular), and bifurcation configuration.
Key Findings and Statistical Analysis
The median age of the cohort was 56 years, and 56% were female. Over the 4-year follow-up period, instability occurred in 235 of the 1,416 UIAs (16.6%). The data revealed a clear dose-response relationship between the extent of wall enhancement and the risk of future adverse events.
Absolute and Cumulative Risk
The absolute cumulative risk of instability at the 4-year mark was markedly higher in the circumferential AWE group. Specifically, 36.8% (95% CI, 30.7%-43.0%) of UIAs with circumferential AWE became unstable. In contrast, the risk was 17.2% (95% CI, 13.4%-21.1%) for focal AWE and 11.4% (95% CI, 11.9%-16.1%) for those with no AWE. This indicates that more than one-third of aneurysms exhibiting circumferential enhancement will either grow or rupture within four years.
Predictive Value and Hazard Ratios
In unadjusted models, circumferential AWE was associated with a nearly four-fold increase in the risk of instability (HR, 3.80; 95% CI, 2.82-5.14). Critically, even after adjusting for traditional morphological predictors—including the size ratio (the ratio of the maximum aneurysm height to the average vessel diameter), aneurysm location (e.g., posterior circulation), and shape irregularity—circumferential AWE remained a significant independent predictor (adjusted HR, 2.21; 95% CI, 1.56-3.13). This suggests that AWE provides unique biological information that morphology alone cannot provide.
Expert Commentary and Mechanistic Insights
The biological plausibility of AWE as a marker of instability is rooted in histopathological studies. Enhancement on MRI is thought to reflect gadolinium leakage into the aneurysm wall due to endothelial dysfunction, increased permeability, and the presence of inflammatory infiltrates (such as macrophages and T-cells). Furthermore, the development of vasa vasorum—small vessels within the wall itself—is associated with wall thickening and subsequent enhancement. These pathological changes weaken the structural integrity of the internal elastic lamina and the media, predisposing the aneurysm to expansion or catastrophic failure.
The distinction between focal and circumferential enhancement is particularly noteworthy. While focal enhancement may represent localized atherosclerotic plaques or organized thrombus, circumferential enhancement likely signifies a more systemic and aggressive inflammatory state across the entire aneurysmal sac. This study confirms that circumferential enhancement is the most clinically relevant phenotype for risk stratification.
However, several limitations must be considered. First, the study was conducted entirely within a Chinese population; while the results are compelling, further validation in Western cohorts is necessary to account for potential genetic and environmental differences in aneurysm natural history. Second, while the study used 3-T MRI, the specific protocols for VWI can vary between manufacturers and centers, emphasizing the need for standardized imaging parameters before AWE can be formally incorporated into international guidelines.
Clinical Implications and Future Directions
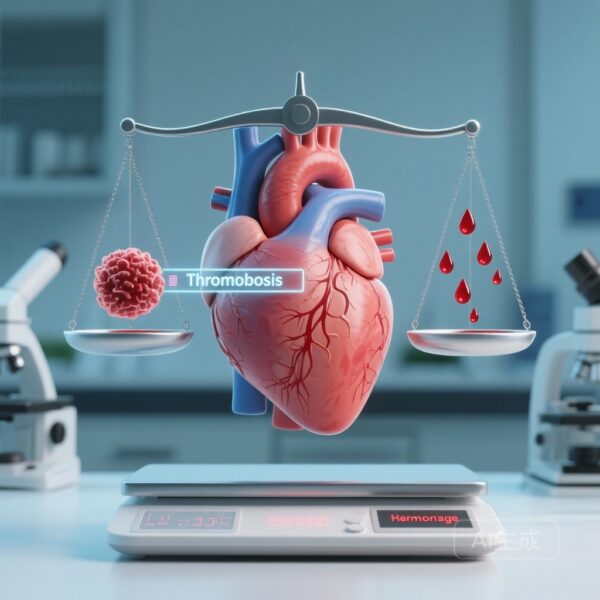
The findings by Liu et al. have immediate implications for the clinical management of UIAs. For many years, the “size threshold” (often 5 mm or 7 mm) has been the primary driver of the decision to treat. However, clinicians frequently encounter small aneurysms that rupture and large aneurysms that remain stable for decades. MRI wall imaging offers a way to move toward a more personalized, “precision medicine” approach.
Aneurysms that demonstrate circumferential AWE, even if they fall below traditional size thresholds for intervention, should perhaps be viewed with a higher degree of suspicion. Conversely, the absence of AWE in a larger aneurysm might provide some reassurance for continued observation, although it should not be the sole factor in deciding against treatment. As the technology becomes more accessible, VWI could become a standard adjunct to CTA and MRA in the initial evaluation of all UIAs.
Conclusion
In summary, this large-scale prospective study establishes circumferential aneurysm wall enhancement as a robust, independent radiological biomarker for UIA instability. With a 36.8% risk of growth or rupture within four years, circumferential AWE identifies a high-risk subset of patients who may benefit from early surgical or endovascular intervention. This research represents a significant step forward in our ability to predict the natural history of intracranial aneurysms and ultimately reduce the burden of subarachnoid hemorrhage.
References
1. Liu Q, Nie X, Vergouwen MDI, et al. Gadolinium-Enhanced Aneurysm Wall Imaging and Risk of Intracranial Aneurysm Growth or Rupture. JAMA Neurol. 2025;82(11):1135-1143. doi:10.1001/jamaneurol.2025.3209.
2. Mossa-Basha M, de Havenon A, Becker KJ, et al. Added Value of Vessel Wall Magnetic Resonance Imaging in the Management of Intracranial Aneurysms. Stroke. 2019;50(1):211-217.
3. Vergouwen MDI, Backes D, van der Schaaf IC, et al. Predictors of Aneurysm Growth and Rupture: A Systematic Review. Stroke. 2017;48(10):2859-2861.