The Struggle Against the Self: Sarah’s Story
For Sarah, a 45-year-old teacher from Chicago, life had become a series of hospital visits and exhaustion. Five years ago, she was diagnosed with Autoimmune Hemolytic Anemia (AIHA), a condition where the body’s immune system mistakenly identifies its own red blood cells as foreign invaders and destroys them.
Initially, high-dose steroids and rituximab provided some relief, but the effect was fleeting. Sarah eventually became part of a group of patients known as multirefractory. She had failed four different lines of therapy, including a splenectomy and various immunosuppressants. Her hemoglobin levels remained dangerously low, her skin was perpetually jaundiced from the breakdown of blood cells, and the threat of a life-threatening crisis was always present.
For patients like Sarah, standard medicine had run out of answers. However, a revolutionary approach—borrowed from the frontiers of cancer treatment—is now offering hope. This approach is CD19-directed chimeric antigen receptor (CAR) T-cell therapy.
What is Autoimmune Hemolytic Anemia?
To understand the breakthrough, we must first understand the enemy. In primary AIHA, the immune system’s B-cells produce autoantibodies. These antibodies latch onto red blood cells, marking them for destruction by the spleen and liver. The result is anemia, which leads to severe fatigue, shortness of breath, and in extreme cases, organ failure.
While many patients respond to initial treatments that suppress the immune system, a significant subset experiences frequent relapses. The problem lies in the persistence of these autoreactive B-cells. Even if a drug clears many of them, a small reservoir often remains, ready to trigger the disease again. In multirefractory AIHA, the disease is so aggressive that it bypasses at least three different types of standard treatments.
The CAR T-Cell Revolution: From Cancer to Autoimmunity
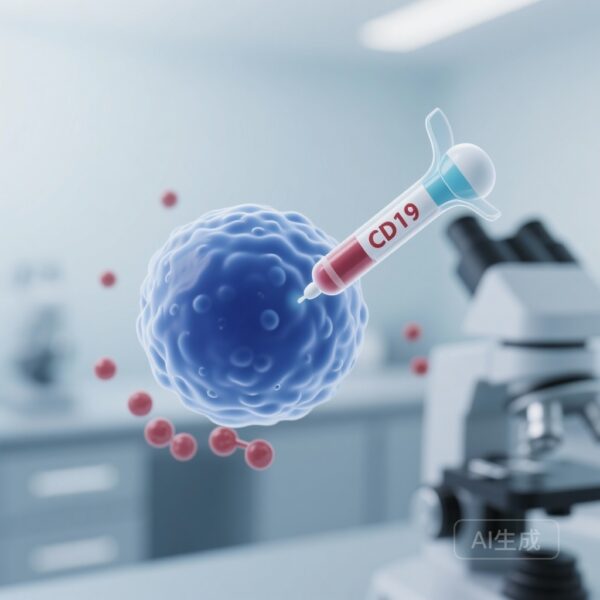
CAR T-cell therapy has already changed the landscape of oncology, particularly for B-cell lymphomas and leukemias. The process involves collecting a patient’s own T-cells (the soldiers of the immune system) and genetically engineering them in a laboratory to express a specific receptor called a Chimeric Antigen Receptor (CAR).
In this study, the CAR was designed to target CD19, a protein found on the surface of most B-cells. Once these engineered cells are infused back into the patient, they act as a living drug, seeking out and destroying every CD19-expressing B-cell in the body. The goal in AIHA is to achieve a profound, total depletion of the B-cells responsible for the harmful autoantibodies, essentially rebooting the patient’s immune system.
What the Data Tell Us: Results of the Breakthrough Study
In a study recently published in the New England Journal of Medicine (Li R, et al.), researchers evaluated the safety and efficacy of CD19 CAR T-cell therapy in 11 patients with multirefractory primary AIHA. This group included patients from a phase 1 study and a compassionate-use program.
The results were nothing short of remarkable. Every single one of the 11 patients (100%) achieved a complete response. The median time to reach this response was 45 days. More importantly, these patients achieved drug-free remission. This means they were able to stop taking steroids and other toxic immunosuppressants while maintaining healthy hemoglobin levels and normal markers of hemolysis (blood destruction).
Comparative Overview of AIHA Treatments
| Treatment Type | Mechanism | Challenges in Refractory Cases |
|---|---|---|
| Corticosteroids | Broad immune suppression | Significant side effects; high relapse rate upon tapering |
| Rituximab | Monoclonal antibody targeting CD20 | Partial B-cell depletion; many patients do not respond or eventually relapse |
| Splenectomy | Surgical removal of the site of blood destruction | Invasive; increased risk of severe infections; does not stop antibody production |
| CD19 CAR T-Cell Therapy | Genetically engineered cellular targeting of CD19 | Requires specialized infrastructure; provides deep B-cell depletion and potential for long-term remission |
Safety and Potential Side Effects
Whenever a therapy is as powerful as CAR T, safety is a primary concern. CAR T-cell therapy is known for two specific types of side effects: Cytokine-Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS).
In the study by Li and colleagues, the safety profile was manageable and consistent with what clinicians see in cancer treatments. Nine out of the 11 patients experienced CRS, but it was limited to grade 1 or 2 (mild to moderate), characterized mainly by fever and flu-like symptoms. Only one patient experienced grade 1 neurotoxicity.
While 15 infections occurred among the participants, none were classified as grade 4 or higher. This suggests that while B-cell depletion does temporarily weaken certain aspects of the immune system, with proper monitoring and supportive care, the risks are controllable.
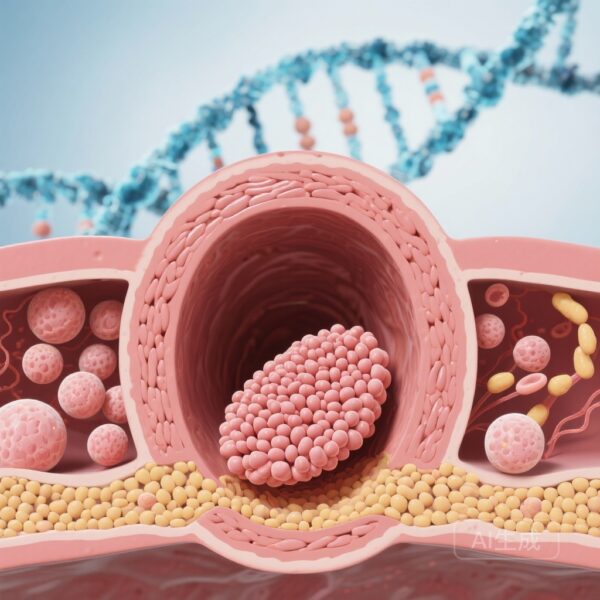
The Science of Remission: Multi-Omics and the B-Cell Niche
What makes this study particularly insightful is the use of multi-omics—the simultaneous analysis of various biological molecules. Researchers used single-cell RNA sequencing and B-cell receptor sequencing to track how the immune system recovered after the CAR T-cells did their work.
They found that in patients who stayed in drug-free remission, the new B-cells that eventually grew back were naive B-cells—essentially a fresh, non-aggressive immune population. However, the study also identified a specific relapse-specific B-cell niche. In cases where the disease might return, researchers noticed a complex crosstalk between specific B-cells (HLA-DRB5+), CD4+ T-cells, and long-lived plasma cells. Understanding this niche could help doctors predict who might need further treatment and who is truly cured.
Expert Insights and the Future of Care
Dr. Michael Thompson, a leading clinical researcher in hematology, notes that this study marks a pivotal shift. For decades, we have used blunt tools to suppress the immune system in AIHA. CAR T-cell therapy represents a precision strike. It doesn’t just manage the disease; it aims to eliminate the source of the problem.
The implications of this study extend beyond AIHA. If CD19 CAR T-cells can successfully treat this condition, they may also be effective for other B-cell-mediated autoimmune diseases, such as Lupus or Myasthenia Gravis. We are entering an era of cellular immunotherapy for autoimmunity, not just cancer.
Conclusion
CD19 CAR T-cell therapy offers a potent new lifeline for those suffering from the most severe forms of Autoimmune Hemolytic Anemia. By achieving deep B-cell depletion, it allows the body to reset and maintain healthy blood levels without the need for lifelong, debilitating drugs. While the therapy requires careful monitoring for side effects like CRS, the 100% response rate in this small cohort suggests a bright future for this high-tech approach.
For patients like Sarah, this science isn’t just about data; it is about the ability to walk to the park, teach a class, and live a life no longer shadowed by the destruction of her own blood.
Funding and Trial Information
This study was funded by the National Key Research and Development Program of China and other supporting institutions. ClinicalTrials.gov number: NCT06231368.
References
Li R, et al. CD19 CAR T-Cell Therapy for Autoimmune Hemolytic Anemia. New England Journal of Medicine. N Engl J Med 2026;394:253-267. DOI: 10.1056/NEJMoa2509820