Highlights of the Research
The role of innate immunity in the progression of atherosclerotic cardiovascular disease (ASCVD) has gained significant attention in recent years. A landmark study published in JAMA Cardiology (2025) provides compelling evidence that calprotectin, a biomarker of neutrophil activation, serves as an independent predictor of major adverse cardiovascular events. The key takeaways from this research include:
- Calprotectin levels are independently associated with a 43 percent increased risk of ASCVD events, even after rigorous adjustment for traditional risk factors and contemporary biomarkers such as high-sensitivity C-reactive protein (hs-CRP), NT-proBNP, and cardiac troponin T.
- Higher circulating calprotectin correlates with increased coronary artery calcium (CAC) scores, indicating a strong link between neutrophil-driven inflammation and subclinical atherosclerosis.
- In vitro translational data suggest that calprotectin is not merely a marker but a mediator of disease, as it impairs endothelial integrity and promotes endothelial-to-mesenchymal transition (EndMT).
- The study highlights the potential of calprotectin as a ‘mechanistically informed’ biomarker that captures inflammatory pathways distinct from those measured by hs-CRP.
The Evolving Landscape of Cardiovascular Inflammation
For decades, the management of ASCVD focused primarily on lipid-lowering therapies. However, despite achieving target LDL-C levels, many patients continue to experience cardiovascular events, a phenomenon known as residual inflammatory risk. High-sensitivity C-reactive protein (hs-CRP) has been the gold standard for assessing this risk, as demonstrated by the CANTOS and COLCOT trials. Yet, hs-CRP is a downstream marker of the IL-1β/IL-6 axis and may not fully capture the complexity of the innate immune response, particularly the role of neutrophils.
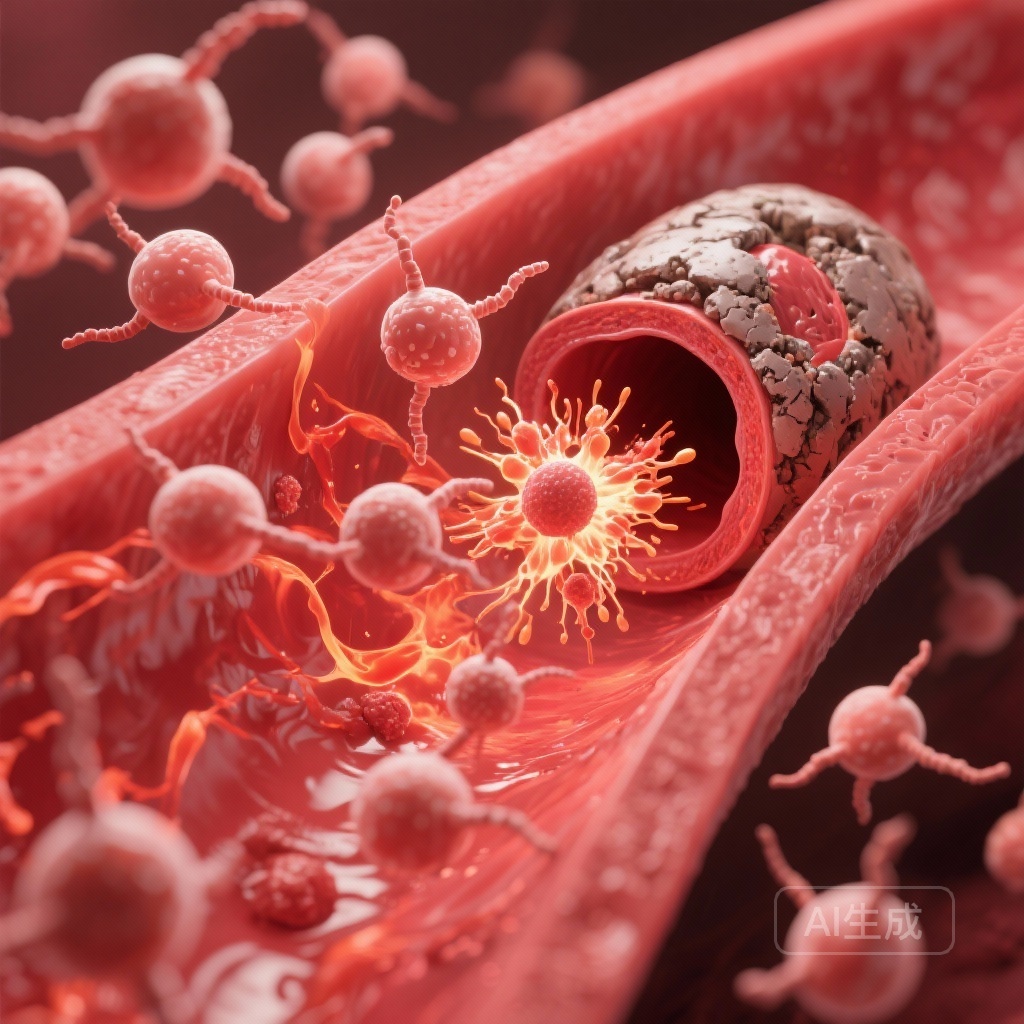
Neutrophils are the most abundant leukocytes in human blood and are early responders in the inflammatory cascade. Upon activation, they release calprotectin (a heterodimer of S100A8 and S100A9), which acts as a damage-associated molecular pattern (DAMP) and amplifies the inflammatory response. Understanding whether calprotectin provides incremental prognostic value over established markers is critical for refining cardiovascular risk stratification.
Study Design and Methodology: The Dallas Heart Study
The research utilized data from Phase 2 of the Dallas Heart Study (DHS), a multiethnic, population-based cohort known for its rigorous phenotyping. The study included 2,412 participants with a median follow-up of 8 years after plasma collection. The diverse nature of the cohort (including a significant representation of Black and Hispanic individuals) ensures that the findings are broadly applicable to modern clinical practice.
The primary outcome was defined as the first occurrence of nonfatal myocardial infarction, nonfatal stroke, coronary revascularization, or cardiovascular death. Researchers employed Cox proportional hazards models to assess the association between log-transformed calprotectin levels and these events. The models were adjusted in stages, accounting for traditional risk factors (age, sex, race, hypertension, diabetes, smoking, and lipids) and then for contemporary biomarkers (hs-CRP, NT-proBNP, and hs-cTnT).
Epidemiological Findings: Calprotectin as a Predictor
The results revealed that higher calprotectin levels were significantly associated with a higher burden of cardiovascular risk factors. Individuals in the highest quartiles of calprotectin were more likely to be older, male, and have a history of hypertension or diabetes. Interestingly, calprotectin also correlated with metabolic derangements, including higher VLDL cholesterol and triglycerides, and lower HDL cholesterol and cholesterol efflux capacity.
The prospective analysis showed a robust association with future ASCVD events. The unadjusted hazard ratio (HR) was 1.98 per log increase in calprotectin. After adjusting for prior ASCVD and traditional risk factors, the HR remained significant at 1.61. Most importantly, when hs-CRP, NT-proBNP, and hs-cTnT were added to the model, calprotectin remained an independent predictor (HR 1.43; 95% CI, 1.04-1.96). This suggests that calprotectin provides unique information regarding cardiovascular risk that is not captured by current clinical standard markers.
Furthermore, the study found a dose-response relationship between calprotectin and coronary artery calcium scores. This association reinforces the idea that calprotectin levels reflect the underlying burden of atherosclerotic plaque and the activity of the inflammatory processes within the vessel wall.
Translational Insights: Mechanisms of Endothelial Injury
To move beyond correlation, the researchers conducted in vitro studies to explore the biological effects of calprotectin on the vascular endothelium. These experiments provided crucial mechanistic insights into how elevated calprotectin might drive ASCVD progression.
1. Impairment of Endothelial Integrity
The study found that calprotectin directly compromises the endothelial barrier. By disrupting cell-cell junctions, calprotectin increases vascular permeability, which is a hallmark of early-stage atherosclerosis and plaque instability.
2. Reduction of Nitric Oxide Production
Nitric oxide (NO) is essential for maintaining vascular tone and preventing platelet aggregation. Calprotectin was shown to diminish NO production in coronary endothelial cells, leading to endothelial dysfunction—a critical precursor to clinical cardiovascular events.
3. Promotion of Endothelial-to-Mesenchymal Transition (EndMT)
Perhaps most significantly, the researchers observed that calprotectin fosters EndMT. During this process, endothelial cells lose their specific markers and acquire mesenchymal characteristics, contributing to vascular stiffness, fibrosis, and plaque calcification. This provides a clear biological pathway linking neutrophil activation to the structural changes seen in atherosclerotic arteries.
Clinical Implications and Expert Commentary
The findings from this study suggest that calprotectin could be a valuable addition to the clinician’s toolkit for risk stratification. Unlike hs-CRP, which is a general marker of systemic inflammation, calprotectin specifically reflects the activation of the innate immune system and neutrophils. This makes it a ‘mechanistically informed’ biomarker that could help identify a subset of patients with high residual inflammatory risk who might benefit from targeted anti-inflammatory therapies.
However, experts caution that while the association is statistically significant and biologically plausible, its clinical utility warrants further prospective validation. Specifically, it remains to be seen whether incorporating calprotectin into standard risk calculators (like the ASCVD Risk Estimator Plus) significantly improves clinical decision-making or patient outcomes. Additionally, the potential for calprotectin as a therapeutic target—perhaps through S100A8/A9 inhibitors—is an exciting area for future pharmacology research.
Conclusion
In summary, calprotectin is a potent and independent predictor of ASCVD events in a multiethnic population. Its association with subclinical atherosclerosis and its direct role in promoting endothelial dysfunction and EndMT suggest that it is more than a bystander in cardiovascular disease. As we move toward a more personalized approach to cardiovascular medicine, calprotectin may serve as a critical bridge between immunology and cardiology, helping clinicians better understand and manage the inflammatory drivers of atherosclerosis.