The Evolution of PFO Closure: From Permanent Metal to Bioresorbable Solutions
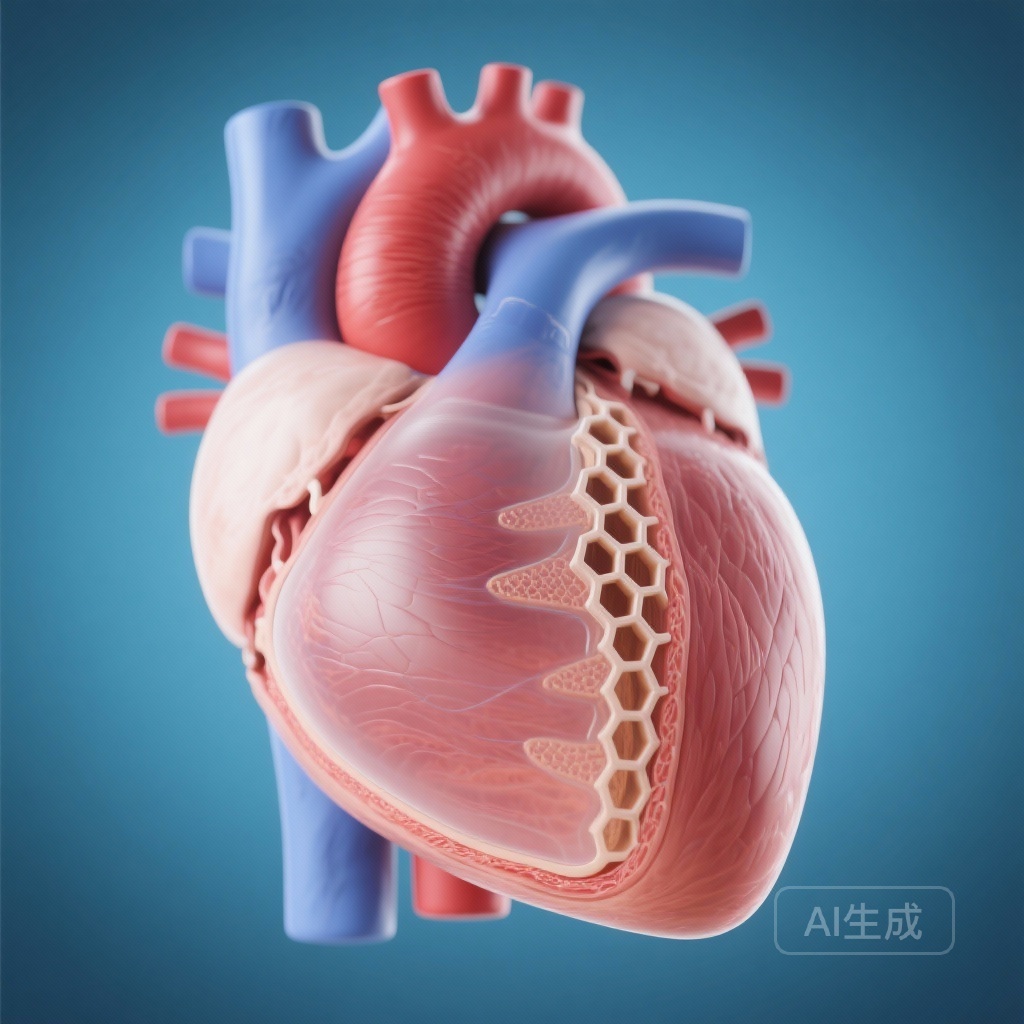
For decades, the standard of care for transcatheter closure of a patent foramen ovale (PFO) has relied on permanent metallic implants, primarily constructed from nitinol (a nickel-titanium alloy). While these devices have proven highly effective in reducing the risk of recurrent cryptogenic stroke, they are not without long-term concerns. Permanent metallic structures in the heart carry inherent risks, including nickel hypersensitivity, late-onset atrial arrhythmias, thrombus formation on the device surface, and the rare but catastrophic complication of cardiac erosion.
The quest for a ‘leave nothing behind’ approach has led to the development of biodegradable technology. The recent publication of the trial by Zhang et al. in Circulation (2026) marks a significant milestone in this journey, providing the first randomized controlled evidence that a novel biodegradable PFO closure device can match the performance of traditional nitinol-based occluders while eventually resorbing into the body.
Highlighting the Trial’s Core Outcomes
The trial produced several critical insights for the clinical community:
1. Noninferior Efficacy: The biodegradable device achieved a 90.63% closure success rate at 6 months, compared to 91.49% for the nitinol control group, meeting the strict noninferiority criteria.
2. Complete Resorption: Transthoracic echocardiography confirmed that the hyperechoic signature of the device began to diminish within 12 months and was entirely absent by 24 months post-implantation.
3. Excellent Safety Profile: No instances of death, systemic embolism, device-related thrombosis, or cardiac erosion were reported in either cohort throughout the 24-month follow-up period.
4. Procedural Nuance: While generally safe, one patient in the biodegradable group required surgical intervention due to intraprocedural device deformation, highlighting the importance of technical proficiency and device handling.
Background: The Clinical Challenge of the Patent Foramen Ovale
A Patent Foramen Ovale is a remnant of fetal circulation present in approximately 25% of the general adult population. While usually benign, it can serve as a conduit for paradoxical embolism—allowing venous thrombi to bypass the pulmonary filter and enter the systemic circulation, leading to ischemic stroke or systemic embolic events.
Large-scale clinical trials such as RESPECT, CLOSE, and REDUCE have firmly established that transcatheter PFO closure is superior to medical therapy alone for secondary prevention in patients with cryptogenic stroke. However, as the population receiving these implants is often young, the prospect of a permanent metal implant residing in the atrial septum for 40 to 50 years remains a point of clinical hesitation. Biodegradable materials offer a solution by providing the necessary scaffold for tissue endothelization and then disappearing once their mechanical function is no longer required.
Study Design: A Rigorous Multicenter Evaluation
This prospective, multicenter, randomized controlled trial enrolled 190 patients with clinically significant PFO. Participants were randomly assigned in a 1:1 ratio to receive either the novel biodegradable device (n=96) or a traditional nitinol-based occluder (n=94).
The primary efficacy endpoint was defined as successful PFO closure at 6 months, verified by contrast echocardiography (the ‘bubble study’). Success was characterized by the absence of significant right-to-left shunting. Secondary endpoints included long-term closure rates at 12 and 24 months, device-related complications, and the rate of device disappearance on imaging.
Key Results: Efficacy and Noninferiority
The study was powered as a noninferiority trial with a predefined margin of -10%. At the 6-month primary endpoint, the biodegradable group showed a success rate of 90.63% (87/96), while the nitinol group showed 91.49% (86/94). The lower limit of the 95% confidence interval for the difference was -8.98%, which comfortably stayed above the -10% margin, confirming the biodegradable device’s noninferiority.
Over the 24-month follow-up, the closure rates remained stable and comparable between the two groups. This indicates that the gradual degradation of the device scaffold does not compromise the integrity of the septal seal, likely because the body’s own endothelial tissue has fully integrated and closed the foramen before the material loses its structural strength.
Safety Profile and Procedural Observations
Safety is the paramount concern when introducing new materials into the heart. The Zhang et al. study reported zero cases of device-related thrombus—a significant finding, as the presence of foreign material usually acts as a nidus for clot formation until endothelization is complete. Furthermore, the absence of erosion is encouraging, as the biodegradable material is designed to be less rigid than nitinol, potentially reducing mechanical stress on the surrounding atrial walls.
One complication was noted: a single patient in the trial group experienced intraprocedural deformation of the biodegradable device, necessitating surgical removal. This suggests that while the material is effective, it may have different haptic properties and structural limits compared to nitinol, requiring a specific learning curve for interventionists.
The Disappearing Act: Longitudinal Imaging Results
The most distinctive feature of this novel device is its metabolic fate. Unlike nitinol, which remains visible on echocardiography and fluoroscopy indefinitely, the biodegradable polymer (typically composed of materials like poly-L-lactic acid or similar esters) undergoes hydrolysis.
The study’s imaging protocol documented a clear timeline of this resorption. At 12 months, the hyperechoic ‘brightness’ of the device on transthoracic echocardiography began to fade. By 24 months, the device was no longer detectable. This ‘vanishing’ profile is ideal for patients who may require future transseptal procedures, such as left atrial appendage closure or mitral valve interventions, as it leaves the septum in a more ‘native’ state without obstructive hardware.
Expert Commentary: A Paradigm Shift in Structural Heart Intervention?
The results of this trial suggest we are entering an era of ‘temporary’ structural implants. The concept of ‘leave nothing behind’ has been explored in coronary stents with mixed results, but the atrial septum may be a more forgiving environment. The lower pressure and different flow dynamics of the atria compared to coronary arteries may make biodegradable materials more suitable here.
However, clinicians should remain cautious. While noninferiority was proven at 24 months, longer-term data (5-10 years) will be essential to ensure that the absence of the device does not lead to late recanalization of the PFO. Additionally, the cost-effectiveness of these novel devices compared to the relatively inexpensive and reliable nitinol occluders will influence their adoption in standard clinical practice.
Conclusion: The Future of ‘Leave Nothing Behind’
The novel biodegradable PFO closure device represents a sophisticated fusion of material science and interventional cardiology. By matching the efficacy and safety of the gold-standard nitinol device while offering the unique benefit of complete resorption, it addresses many of the long-term anxieties associated with permanent cardiac implants. For the young patient following a cryptogenic stroke, the prospect of a device that does its job and then disappears is an attractive therapeutic evolution.
Funding and clinicaltrials.gov
This study was supported by various national medical research grants. Clinical trial registration can be found at clinicaltrials.gov (specific registration numbers are available in the primary manuscript).
References
1. Zhang F, Dong J, Wei P, et al. Transcatheter Closure of Patent Foramen Ovale With a Novel Biodegradable Device: A Prospective, Multicenter, Randomized Controlled Clinical Trial. Circulation. 2026;153(2):71-81.
2. Mas JL, Derumeaux G, Guillon B, et al. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med. 2017;377(11):1011-1021.
3. Søndergaard L, Kasner SE, Rhodes JF, et al. Patent Foramen Ovale Closure or Antiplatelet Therapy for Cryptogenic Stroke. N Engl J Med. 2017;377(11):1033-1042.