Highlights of the J-PVAD Registry Analysis
The recent analysis of the Japanese Registry for Percutaneous Ventricular Assist Device (J-PVAD) provides critical insights into the real-world application of mechanical circulatory support (MCS). Key highlights include:
1. Only 35.6% of AMI-CS patients treated with Impella in clinical practice met the strict DanGer shock trial eligibility criteria.
2. Mortality remains high in specific subgroups excluded from trials, particularly those with out-of-hospital cardiac arrest (51.3% mortality) and mechanical complications (39.8%).
3. The use of ECPELLA (combined Impella and VA-ECMO) is associated with a 46.1% overall 30-day mortality, which can be stratified using the new J-PVAD score.
4. Age over 80 years and pre-implantation metabolic markers (lactate, creatinine) are the most potent predictors of adverse outcomes in the ECPELLA cohort.
Introduction: The Shifting Landscape of Cardiogenic Shock Management
Acute myocardial infarction complicated by cardiogenic shock (AMI-CS) remains one of the most challenging conditions in cardiovascular medicine, characterized by a persistent mortality rate hovering near 40-50%. The recent DanGer shock trial marked a significant milestone, demonstrating a survival benefit for the Impella CP device in highly selected patients with ST-elevation myocardial infarction (STEMI). However, randomized controlled trials (RCTs) often operate within narrow parameters that do not reflect the heterogeneity of the ‘all-comers’ population encountered in the emergency department and cardiac catheterization laboratory.
Clinicians often face the dilemma of whether trial results can be extrapolated to patients with non-STEMI, those who have suffered cardiac arrest, or those with mechanical complications like ventricular septal rupture. Two landmark studies utilizing the J-PVAD registry—a nationwide Japanese database—now provide the necessary data to bridge the gap between trial evidence and clinical reality.
Study Methodology: Leveraging the J-PVAD Registry
The J-PVAD registry is an exhaustive, mandatory database in Japan that includes all patients treated with the Impella device. The first study by Arai et al. (published in the European Heart Journal, 2025) identified 3,975 AMI-CS patients treated between 2020 and 2023. These patients were stratified into five cohorts: DanGer-eligible STEMI-CS, non-eligible STEMI-CS, out-of-hospital cardiac arrest (OHCA), mechanical complications (MCs), and non-STEMI-CS (NSTEMI-CS).
The eligibility criteria for the DanGer group were specifically defined as: STEMI-CS with lactate ≥ 2.5 mmol/L, systolic blood pressure (SBP) <100 mmHg or catecholamine requirement, left ventricular ejection fraction (LVEF) <45%, and a window from shock onset to Impella support of ≤24 hours.
The second study, also by Arai et al. (published in the Circulation Journal, 2025), focused specifically on the “ECPELLA” strategy—the simultaneous use of VA-ECMO and Impella—in 922 patients. This study aimed to identify specific risk factors and develop a prognostic score for this high-acuity subset.
Results Part I: Applying DanGer Shock Criteria to a Nationwide Population
The application of DanGer shock criteria to the J-PVAD population revealed a stark reality: nearly two-thirds of real-world Impella users would have been excluded from the trial. Among those who did meet the criteria (35.6%), the 30-day mortality was 37.6%, which aligns closely with the intervention arm of the original DanGer shock trial.
Subgroup Heterogeneity and Mortality Drivers
The outcomes for those who did not meet the criteria were markedly heterogeneous:
1. Non-eligible STEMI-CS: This group actually exhibited the lowest mortality at 27.6%, likely because it included patients with less severe hemodynamic instability or those who received support very early. However, mortality in this group rose sharply in the presence of advanced age, renal dysfunction, or the need for concomitant VA-ECMO.
2. Out-of-Hospital Cardiac Arrest (OHCA): This remains the most lethal subgroup, with a 51.3% 30-day mortality. Notably, if the patient did not achieve the return of spontaneous circulation (ROSC) before support, mortality soared to 63.4%, questioning the utility of routine MCS in this context without clear neuroprognostication.
3. Mechanical Complications (MC): Patients with conditions such as ventricular septal rupture or papillary muscle rupture had a 39.8% mortality rate, reflecting the surgical complexity and anatomical failure that MCS can only partially mitigate.
4. NSTEMI-CS: This group had a 33.3% mortality rate, suggesting that while they were excluded from the primary DanGer trial, they may derive significant benefit from microaxial flow pump support.
Results Part II: The Prognostic Landscape of ECPELLA Support
When cardiogenic shock is so severe that Impella alone provides insufficient flow, or when oxygenation is compromised, clinicians often escalate to ECPELLA. The J-PVAD analysis of 922 ECPELLA patients showed an overall 30-day mortality of 46.1%. While this is high, it reflects a salvage population that would otherwise have a near-certain mortality.
The J-PVAD Score: A Tool for Risk Stratification
The investigators identified five independent predictors of mortality in the ECPELLA cohort, assigning one point to each:
1. Age >80 years
2. In-hospital cardiac arrest (IHCA)
3. Systolic blood pressure < 90 mmHg
4. Creatinine > 1.5 mg/dL
5. Serum lactate >4.0 mmol/L
The resulting J-PVAD score proved to be a powerful, if sobering, predictive tool. A patient with a score of 0 had a 20.0% mortality risk, whereas a patient with a score of 5 faced a 70.0% mortality rate. For patients over 80 with even one additional risk factor, the mortality exceeded 57%, highlighting the need for careful ethical and clinical consideration before initiating such resource-intensive therapy in the elderly.
Expert Commentary: Translating Registry Data into Clinical Practice
The findings from the J-PVAD registry underscore a pivotal concept in modern cardiology: the “trial-to-registry gap.” While the DanGer shock trial provided the “gold standard” evidence for efficacy in a specific niche, the registry data provides the “real-world” context of effectiveness and safety across the spectrum of disease.
The Gap Between Trial Elegance and Real-World Complexity
One of the most significant takeaways is that the DanGer criteria are highly specific but not exhaustive. The lower mortality in the “non-eligible STEMI” group suggests that clinicians are successfully identifying patients who benefit from Impella even before they reach the profound shock state defined by high lactate and low SBP. Conversely, the high mortality in the OHCA group confirms that MCS cannot fix the brain; neurological injury often dictates the outcome regardless of the cardiac support provided.
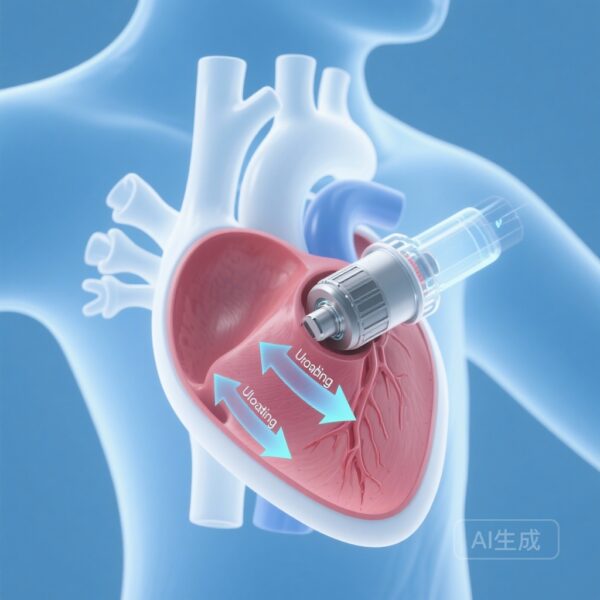
Mechanistic Insights into Unloading and Perfusion
The ECPELLA data reinforces the “ventricular unloading” hypothesis. While VA-ECMO provides systemic perfusion (the “macro-circulation”), it increases left ventricular afterload, which can be deleterious in a failing heart. Adding an Impella device (unloading) mitigates this afterload, reduces pulmonary edema, and lowers myocardial oxygen demand. The J-PVAD score effectively measures the patient’s physiological reserve to withstand the initial insult and the subsequent inflammatory response of MCS.
Conclusion: Moving Toward Individualized Hemodynamic Support
The J-PVAD registry studies remind us that in the management of cardiogenic shock, one size does not fit all. The DanGer shock criteria offer a valuable framework, but they should be viewed as a starting point rather than a strict boundary.
For the clinician at the bedside, the J-PVAD score provides a pragmatic way to communicate risk to families and to make informed decisions about the escalation or withdrawal of care. As we move forward, the focus must shift from simply “can we support the heart?” to “which patient will truly recover?” Future research should continue to refine these risk models, perhaps integrating real-time hemodynamic data and biomarkers to further personalize the application of life-saving mechanical circulatory support.
References
1. Arai R, Kojima K, Fukamachi D, Okumura Y. DanGer shock criteria and outcomes in acute myocardial infarction-related cardiogenic shock treated with Impella: the J-PVAD registry. Eur Heart J. 2025 Oct 13:ehaf787. doi: 10.1093/eurheartj/ehaf787 IF: 35.6 Q1 . PMID: 41078250 IF: 35.6 Q1 .2. Arai R, Murata N, Saito Y, Kojima K, Fukamachi D, Okumura Y; J-PVAD Investigators. Prognostic Survey of ECPELLA in Japanese Patients With Acute Myocardial Infarction and Cardiogenic Shock – Findings From the Japanese Registry for Percutaneous Ventricular Assist Device (J-PVAD). Circ J. 2025 Oct 24;89(11):1778-1785. doi: 10.1253/circj.CJ-24-0522 IF: 3.7 Q1 . PMID: 39358231 IF: 3.7 Q1 .