Highlights
1. Efficacy of Rescue Ablation
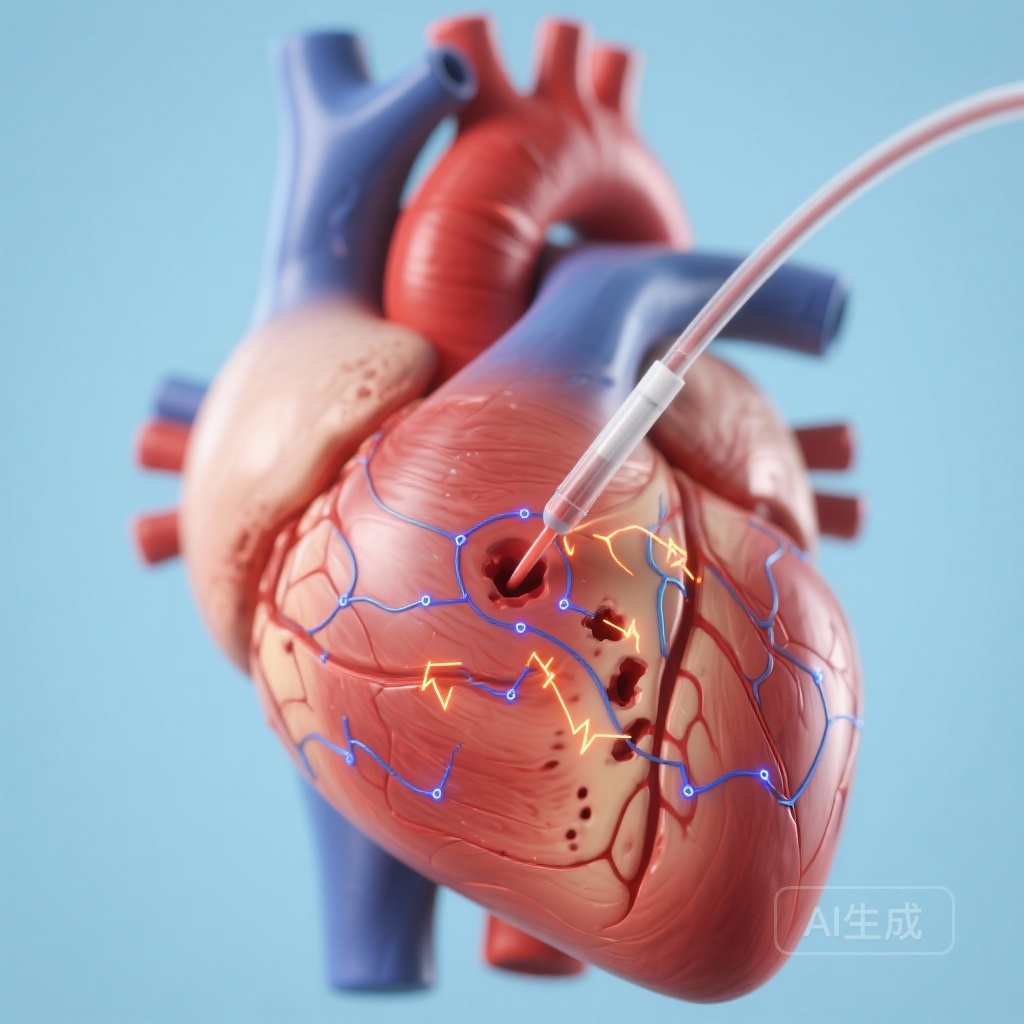
Catheter ablation serves as a potent bailout intervention for incessant ventricular tachycardia (VT) in the early phase of acute myocardial infarction (AMI) when conventional pharmacological and hemodynamic supports are exhausted.
2. Mechanistic Insight
Contrary to previous assumptions of purely ischemic triggers, intracardiac mapping confirms that scar-related reentry within the territory of the culprit artery is the primary driver of refractory VT in early AMI.
3. Clinical Outcomes
High procedural success rates and favorable 18-month survival outcomes suggest that early intervention can stabilize patients who would otherwise face high mortality due to electrical instability.
Introduction and Clinical Context
Ventricular tachycardia (VT) and ventricular fibrillation (VF) remain among the most feared complications following an acute myocardial infarction (AMI). While the widespread adoption of primary percutaneous coronary intervention (PCI) has reduced the incidence of these arrhythmias, approximately 2% of AMI patients still develop VT/VF in the early post-infarction phase. Among these patients, a critical subset (nearly 20%) progresses to a refractory VT storm—a condition characterized by repeated episodes of VT that do not respond to standard revascularization, anti-arrhythmic drugs, sedation, or advanced hemodynamic support.
Historically, clinicians have been hesitant to perform catheter ablation in the acute phase of AMI, often preferring to wait for the maturation of the myocardial scar. However, for patients in incessant VT, waiting is frequently not an option. This study, published in the European Heart Journal: Acute Cardiovascular Care, provides crucial data on the feasibility, safety, and electrophysiological characteristics of catheter ablation as a bailout strategy for this vulnerable population.
Study Design and Population Characteristics
Between 2022 and 2024, researchers screened 12,835 consecutive patients diagnosed with AMI. Of this massive cohort, 261 patients (2.0%) developed VT or VF. Within this group, 51 patients (19.5%) were identified as having a refractory VT storm necessitating intensive intervention. Ultimately, 19 patients who remained in incessant VT despite optimal medical management (including revascularization, multiple anti-arrhythmic agents, and mechanical circulatory support) underwent rescue catheter ablation.
The clinical timeline for these 19 patients was consistent: VT typically developed at a median of 4 days after the onset of AMI and reached an incessant state approximately 2 days after the first occurrence. This highlights a critical window of 48 to 72 hours where medical therapy often fails, necessitating a transition to invasive electrophysiological intervention.
Electrophysiological Characteristics and Procedural Mapping
One of the most significant findings of this study involves the underlying mechanism of early post-AMI VT. Through detailed intracardiac mapping, all 19 cases were identified as being caused by scar-related reentry. The reentry circuits were localized specifically within the territory of the culprit artery responsible for the AMI.
The technical data from the mapping procedures provided the following insights:
Mappable Cycle Length
The endocardial mappable cycle length (CL) accounted for 65.3 ± 7.6% of the total cycle length of the VT. This high percentage of mappable circuits allowed for the identification of critical isthmuses within the endocardium.
Ablation Strategy
Energy delivery was targeted at the components of the critical isthmus. In all cases, VT was successfully eliminated at these sites. Notably, no focal triggers (which are common in purely ischemic VT) were observed after the termination of the reentrant VT. Following the termination, operators performed substrate modification around the termination site to prevent recurrence.
Clinical Results and Safety Outcomes
The immediate procedural success was remarkable. In all 19 patients, the index procedure resulted in the successful suppression of the incessant VT. While two patients experienced recurrent sustained VT during the hospital stay, one was successfully managed with a repeat ablation.
The safety profile was also encouraging, given the critical state of these patients. Only one patient died in the acute phase, and the cause was a cerebral hemorrhage rather than cardiac failure or procedural complication. The remaining 18 patients were successfully stabilized and discharged alive.
Long-term Follow-up
During a median follow-up period of 18 months, the outcomes remained stable. Only one patient developed recurrent VF, and importantly, there were no documented cases of sudden cardiac death. This suggests that suppressing the initial electrical storm via ablation provides a durable benefit that extends well beyond the acute recovery phase.
Expert Commentary and Clinical Implications
The findings of this study challenge the traditional “wait-and-see” approach to post-AMI arrhythmias. For decades, it was theorized that early post-AMI VT was primarily triggered by acute ischemia or focal activity from Purkinje fibers. However, this study demonstrates that even in the very early stages (days 4-6), a functional reentrant substrate exists that is amenable to catheter ablation.
Revisiting the Timing of Intervention
The success of these bailout procedures suggests that the “electrical maturation” of the scar occurs much faster than previously thought. Clinicians should consider catheter ablation earlier in the treatment algorithm for patients who do not respond to the first two anti-arrhythmic agents or who require escalating doses of vasopressors to maintain stability during VT.
Limitations and Future Research
While the results are compelling, the study is limited by its small sample size (19 patients) and its observational, single-center design. Furthermore, these procedures were performed in a high-volume center with significant expertise in both AMI management and complex electrophysiology. The generalizability to smaller centers remains to be seen. Prospective, randomized controlled trials are necessary to formally establish the optimal timing for ablation and to determine if early ablation could prevent the need for prolonged mechanical circulatory support or sedation.
Conclusion
Scar-related reentry is a primary driver of refractory VT even in the early phase of acute myocardial infarction. Catheter ablation at the critical isthmus is not only feasible but highly effective in suppressing VT storm when medical therapy fails. As our understanding of early scar dynamics evolves, catheter ablation is likely to transition from a “last-ditch effort” to a standard component of the multidisciplinary management of complex AMI patients.
References
Li M, Yang Y, Cheng Y, et al. Catheter ablation for refractory ventricular tachycardia early after acute myocardial infarction: management, electrophysiological characteristics, and outcomes. Eur Heart J Acute Cardiovasc Care. 2025;14(11):641-650. doi:10.1093/ehjacc/zuaf102.