Introduction: The Quest for Sustained Remission in ITP
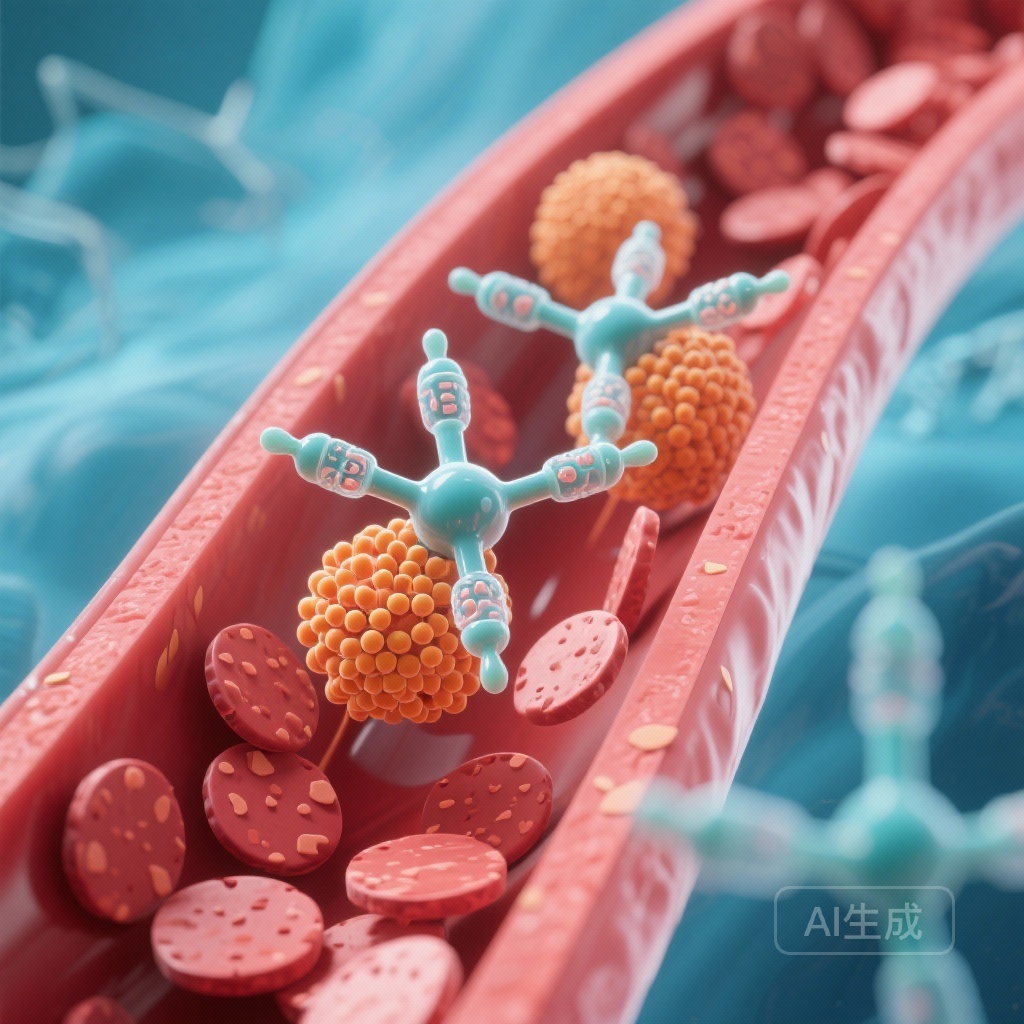
Immune thrombocytopenia (ITP) remains a complex autoimmune disorder characterized by both accelerated platelet destruction and suboptimal platelet production. For decades, the therapeutic landscape was dominated by corticosteroids, followed by a transition to second-line therapies such as splenectomy, rituximab, and thrombopoietin-receptor agonists (TPO-RAs). While TPO-RAs like eltrombopag have revolutionized management by providing high response rates, they often necessitate indefinite administration to maintain safe platelet counts. This chronic dependence poses a significant burden on patients and the healthcare system, highlighting an urgent unmet need for therapies that can induce long-term, treatment-free remission.
The VAYHIT2 trial, recently published in the New England Journal of Medicine, investigates a novel strategy: combining the TPO-RA eltrombopag with a short course of ianalumab, a next-generation B-cell depleting monoclonal antibody. This approach aims to provide both immediate platelet support and deep immune resetting, potentially allowing patients to discontinue therapy while maintaining stable platelet counts.
Highlights of the VAYHIT2 Trial
- Ianalumab combined with eltrombopag significantly increased the probability of remaining free from treatment failure at 12 months (54% in the 9-mg group vs. 30% in the placebo group).
- The time to treatment failure was significantly longer for patients receiving the ianalumab combination, with a hazard ratio of 0.55 for the 9-mg dose.
- A significantly higher percentage of patients achieved a stable response at 6 months without the need for rescue therapy.
- The safety profile of the combination was generally manageable, though higher doses of ianalumab were associated with an increase in serious adverse events compared to placebo.
Disease Burden and the Limitation of Current Therapies
In clinical practice, ITP is not merely a numbers game; it is a condition of significant morbidity, characterized by fatigue, bleeding risks, and the psychological burden of fluctuating platelet counts. First-line glucocorticoids are effective but rarely provide durable remission, and their long-term use is prohibited by a plethora of side effects. TPO-RAs have moved into the second-line setting as highly effective agents, but they function as maintenance therapies rather than cures. When TPO-RAs are discontinued, platelet counts often plummet back to baseline levels. Rituximab, the traditional B-cell depleting agent, offers remission in only about 20-30% of patients at five years. Consequently, the medical community has sought a “one-two punch”—a combination that stimulates production while simultaneously silencing the aberrant immune response.
Study Design: The VAYHIT2 Phase 3 Framework
The VAYHIT2 trial was a phase 3, randomized, double-blind, placebo-controlled study designed to evaluate the efficacy and safety of ianalumab in combination with eltrombopag. The study enrolled 152 adults with primary ITP who had either relapsed or failed to respond to first-line glucocorticoids. Participants were randomized in a 1:1:1 ratio into three distinct groups:
Experimental Arms
- Group 1: Ianalumab (9 mg/kg) monthly for 4 months + daily eltrombopag.
- Group 2: Ianalumab (3 mg/kg) monthly for 4 months + daily eltrombopag.
- Group 3: Placebo monthly for 4 months + daily eltrombopag.
Crucially, the eltrombopag dose was tapered and eventually discontinued by week 24 in patients who met specific platelet stability criteria. This design allowed investigators to assess whether the short-course ianalumab could maintain remission after the TPO-RA was withdrawn.
Endpoints
The primary endpoint was freedom from treatment failure (FTF), a composite measure including platelet counts dropping below 30×10¹ per liter after 8 weeks, initiation of rescue or new therapy, or the inability to discontinue eltrombopag. The key secondary endpoint was a stable response at 6 months, defined as maintaining a platelet count of ≥50×10¹ per liter in 75% of measurements between weeks 19 and 25.
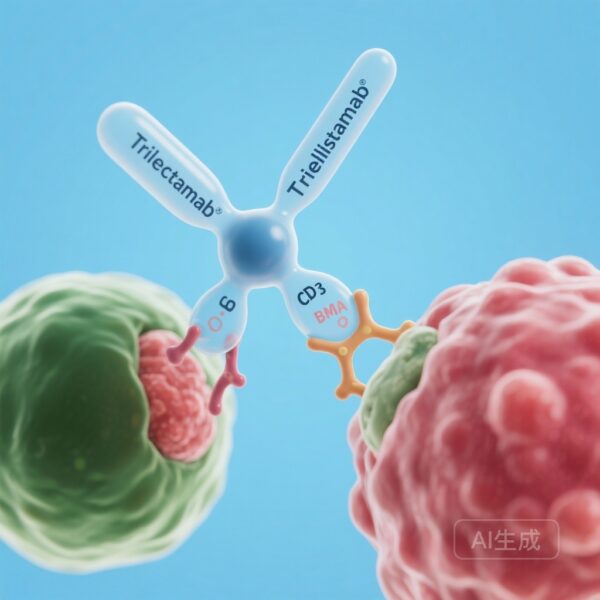
Mechanistic Insight: Why Ianalumab?
Ianalumab is not just another rituximab. While rituximab targets CD20, ianalumab targets the B-cell activating factor (BAFF) receptor. It possesses a dual mechanism of action: it causes direct B-cell depletion via antibody-dependent cellular cytotoxicity (ADCC) and simultaneously blocks the BAFF-receptor signaling pathway, which is essential for B-cell survival and maturation. By targeting the BAFF receptor, ianalumab may more effectively deplete the B-cell subsets responsible for producing the pathogenic autoantibodies found in ITP, potentially leading to a more profound and durable reset of the immune system than traditional agents.
Key Findings: Improved Durability and Response
The results of the VAYHIT2 trial provide compelling evidence for the efficacy of this combination therapy. At the 12-month mark, the probability of being free from treatment failure was significantly higher in both ianalumab groups compared to the placebo arm.
Primary Outcome Results
- 9-mg Ianalumab Group: 54% FTF (95% CI, 39 to 67)
- 3-mg Ianalumab Group: 51% FTF (95% CI, 36 to 64)
- Placebo Group: 30% FTF (95% CI, 18 to 43)
The hazard ratios for treatment failure were 0.55 (P=0.04) and 0.58 (P=0.045) for the 9-mg and 3-mg groups, respectively, indicating a nearly 45% reduction in the risk of treatment failure when ianalumab was added to the regimen.
Secondary and Stable Response
The 9-mg ianalumab group also outperformed the placebo group in terms of stable response at 6 months (62% vs. 39%, P=0.045). This suggests that the higher dose of ianalumab is particularly effective at stabilizing platelet counts during the critical period when eltrombopag is being tapered or has already been discontinued.
Safety and Tolerability Considerations
The overall frequency of adverse events was similar across the three cohorts, suggesting that the addition of ianalumab does not drastically alter the immediate safety profile of ITP treatment. However, clinicians must note the disparity in serious adverse events (SAEs). The 16% SAE rate in the 9-mg group, compared to 6% in the 3-mg group and 4% in the placebo group, warrants careful patient selection and monitoring. Most SAEs in these types of trials are related to infections or infusion-related reactions, emphasizing the need for vigilance when employing potent B-cell depleting agents.
Expert Commentary and Clinical Implications
The VAYHIT2 trial represents a shift toward a more proactive, curative-intent strategy in ITP management. Historically, clinicians have followed a step-wise approach, adding therapies only when others fail. This trial suggests that early combination therapy—using a B-cell depleting agent and a TPO-RA together—can produce better long-term outcomes than using a TPO-RA alone.
However, several questions remain. The trial’s definition of treatment failure is a composite, and while it reflects clinical reality, the specific impact of ianalumab on long-term (multi-year) treatment-free remission is still being characterized. Additionally, the higher rate of serious adverse events in the 9-mg group suggests a dose-response relationship for toxicity that must be weighed against the marginal efficacy gain over the 3-mg dose. In practice, hematologists may need to balance the desire for a “cure” with the risk of immunosuppression-related complications.
Conclusion: A New Chapter in ITP Management
The VAYHIT2 trial successfully demonstrates that a short course of ianalumab, when added to eltrombopag, provides a superior and more durable response in patients with second-line ITP compared to eltrombopag monotherapy. By extending the time to treatment failure and increasing the likelihood of a stable response after TPO-RA discontinuation, ianalumab offers a promising tool for clinicians seeking to move beyond chronic maintenance therapy toward a goal of sustained remission. As we move forward, further data on long-term safety and the optimal timing of this combination will be essential to refining its role in the hematological armamentarium.
Funding and Registration
This study was funded by Novartis. ClinicalTrials.gov number: NCT05653219.