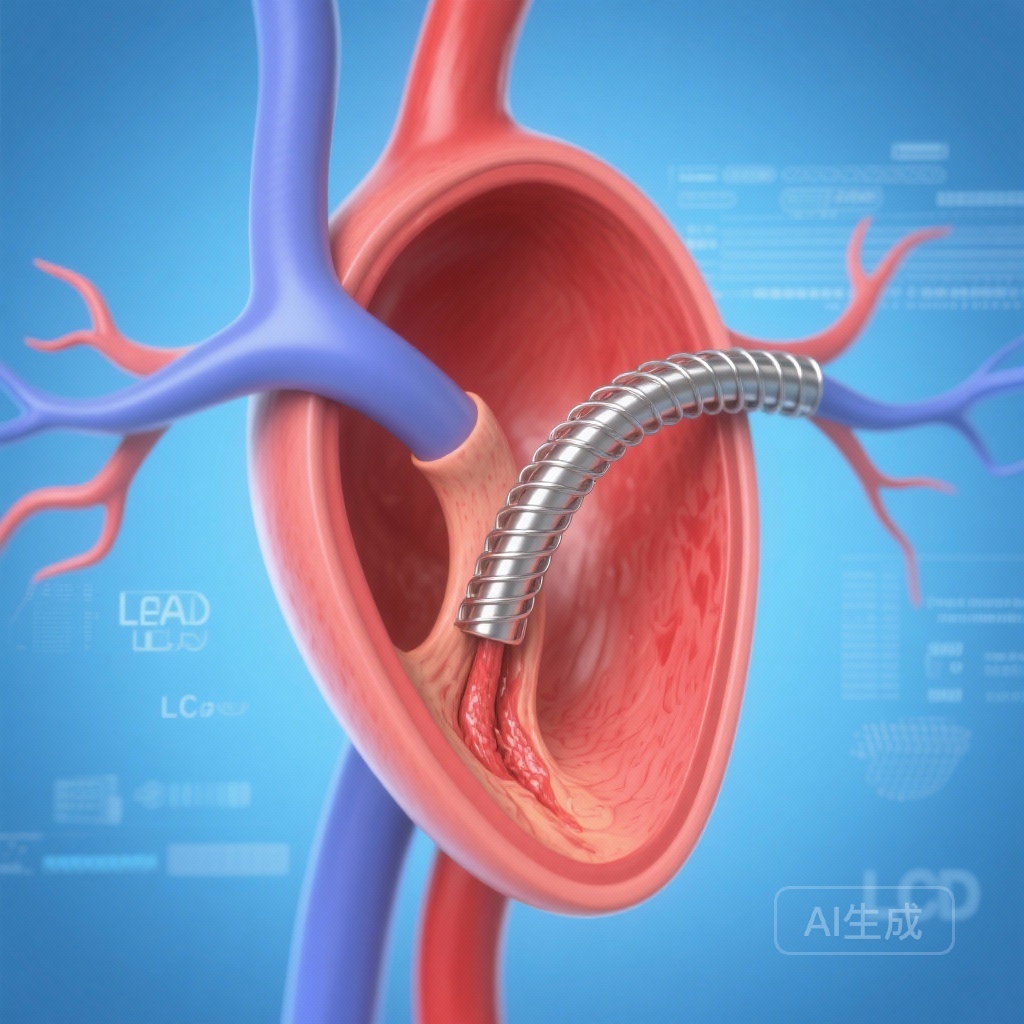
Introduction: The Persistent Challenge of Left Main Bifurcation
Percutaneous coronary intervention (PCI) of the left main (LM) coronary artery bifurcation remains one of the most technically demanding procedures in interventional cardiology. Given the vast myocardial territory at risk, the long-term durability of stenting strategies is of paramount importance. The European Bifurcation Club Left Main (EBC MAIN) trial previously established that at 3 years post-procedure, a stepwise provisional stenting approach was associated with a lower rate of target lesion revascularization (TLR) compared to an upfront dual-stenting strategy. However, the specific anatomical patterns of failure—where exactly the restenosis occurs and how it relates to the initial technique—have remained poorly defined until now.
This subanalysis of the EBC MAIN trial provides a critical deep dive into the morphology of restenosis. By understanding precisely where stenting fails, clinicians can better tailor their procedural choices and anticipate long-term outcomes for patients with complex coronary anatomy.
The EBC MAIN Trial: Context and Background
The original EBC MAIN trial was a randomized clinical study comparing two primary strategies for LM bifurcation lesions: the stepwise provisional approach (typically involving one stent in the main vessel) versus an upfront dual-stenting strategy (using techniques such as DK-crush, Culotte, or T-stenting). While the primary endpoint focused on major adverse cardiac events (MACE), the higher incidence of TLR in the dual-stenting arm raised significant questions regarding the mechanism of late failure.
Bifurcation lesions are inherently prone to restenosis due to complex flow dynamics, shear stress alterations, and the mechanical challenges of ensuring full drug-eluting stent coverage at the ostium of the side branch. In the case of the LM, the side branch is almost always the circumflex (LCx) artery, which often exits at a sharp angle and possesses a unique ostial anatomy that is difficult to navigate and scaffold perfectly.
Study Methodology: Analyzing the Patterns of Failure
This subanalysis focused on the cohort of patients from the EBC MAIN trial who required TLR during the 3-year follow-up period. Out of the original trial population, 48 patients met the criteria for target lesion revascularization and had their restenosis patterns analyzed by an independent core laboratory. Restenosis was defined as a diameter stenosis of 50% or greater within the treated segment.
The mean age of this cohort was 70.3 years, with a predominance of male patients (72.9%). Within this group, 31 patients had been randomized to upfront dual-stenting, and 17 to the stepwise provisional approach. Notably, four patients in the provisional group eventually received a second stent during the index procedure, resulting in a final treatment distribution of 35 dual-stented patients and 13 single-stented patients for the analysis of restenosis location.
Key Findings: The Vulnerability of the Circumflex Ostium
The most striking finding of the study was the overwhelming prevalence of restenosis at the circumflex ostium. Regardless of the initial stenting strategy, the LCx ostium was the culprit lesion for revascularization in 71% of all cases.
Consistency Across Techniques
In patients treated with dual-stenting, 77% of restenosis events involved the LCx ostium. In those treated with a single stent (provisional approach), 54% involved the LCx ostium. While the percentage was numerically higher in the dual-stent group, the difference did not reach statistical significance (P=0.115), suggesting that the LCx ostium is a biologically and mechanically vulnerable site regardless of how many stents are placed.
Isolated Restenosis Patterns
The study identified isolated ostial circumflex restenosis as the single most common pattern, occurring in 58% of the total cohort. This suggests that in many cases, the main vessel (LM to Left Anterior Descending [LAD]) remains patent and healthy, while the failure is localized specifically to the entry point of the LCx.
Quantitative Analysis of Stenosis
During the 3-year follow-up, the mean percentage of diameter stenosis at the circumflex ostium was remarkably similar between the two groups. Dual-stented patients showed a mean stenosis of 64.6%, while single-stented patients showed 60.5% (coefficient -0.12; 95% CI, -0.46 to 0.22; P=0.473). This data reinforces the conclusion that neither strategy effectively eliminates the risk of late LCx ostial narrowing.
The Impact of Stent Directionality: LAD vs. LCx
An interesting technical observation emerged regarding the choice of the “main vessel” in single-stenting. Traditionally, the LAD is considered the primary vessel, and the LCx is treated as the side branch. However, in some anatomical variations, the operator may choose to stent from the LM into the LCx.
The subanalysis found that single stenting from the LM to the LCx was associated with significantly worse subsequent mean diameter stenosis at the LAD ostium compared to the traditional LM-to-LAD approach (49.8% vs. 19.8%; P=0.049). This suggests that the LAD ostium may be more sensitive to being “jalled” or shifted when the LCx is treated as the primary vessel, further complicating the decision-making process in cases where the LCx is the more dominant or diseased vessel.
Mechanistic Insights: Why the Circumflex Fails
Several factors contribute to the LCx ostium being the “Achilles’ heel” of LM bifurcation PCI:
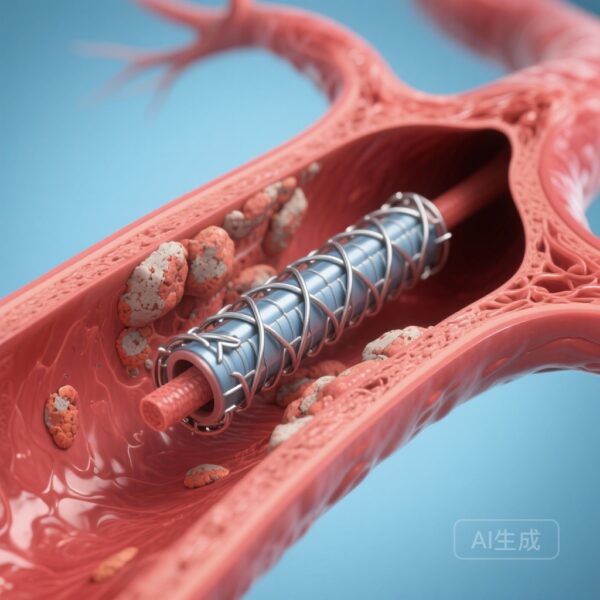
1. Carina Shift: During stent expansion in the main vessel, the carina (the ridge of tissue between the two branches) can be displaced toward the side branch, causing immediate or late narrowing.
2. Incomplete Apposition: The wide angle often found at the LM-LCx junction makes it difficult for stent struts to fully appose the vessel wall, leading to areas of low shear stress and subsequent neointimal hyperplasia.
3. Mechanical Stress: The heart’s contraction causes significant movement and bending at the LM bifurcation, particularly affecting the LCx. This constant mechanical strain can lead to stent fatigue or localized vessel wall irritation.
4. Drug Delivery Gaps: In dual-stent techniques, the complexity of overlapping layers (such as in the ‘crush’ or ‘culotte’ techniques) can sometimes lead to non-uniform drug delivery or localized inflammation.
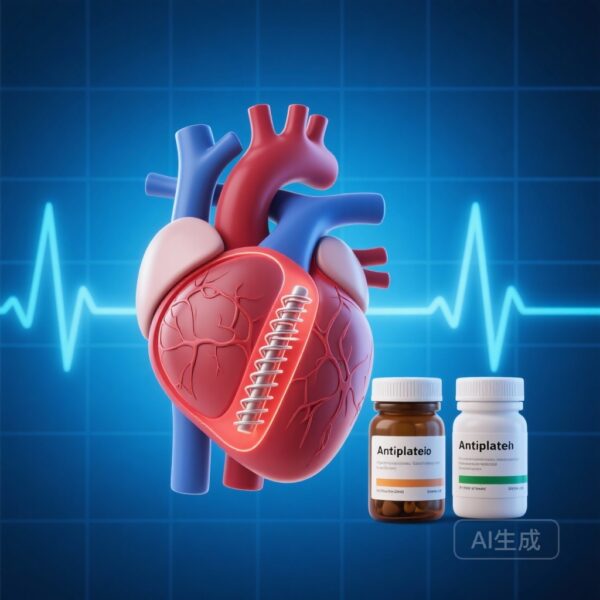
Clinical Implications for the Interventionalist
For the practicing clinician, these results reinforce the EBC MAIN trial’s primary conclusion: the stepwise provisional approach should remain the default strategy for most LM bifurcation lesions. Since dual-stenting does not appear to protect the LCx ostium from restenosis any better than a single-stent approach—and is associated with higher TLR rates overall—the added complexity of a two-stent strategy is often not justified as an upfront choice.
However, the high rate of LCx failure in both groups highlights an unmet medical need. The study suggests that we need better tools for treating the LCx ostium. This might include the more frequent use of drug-coated balloons (DCBs) for side branch protection, more precise intravascular imaging (IVUS or OCT) to ensure optimal stent expansion and ostial coverage, or the development of dedicated bifurcation stents designed specifically for the unique geometry of the LM.
Conclusion: Refining the Approach to Left Main PCI
The EBC MAIN subanalysis provides a sobering reminder that despite advances in stent technology, the circumflex ostium remains a stubborn challenge. With 71% of revascularization events localized to this site, the focus of future research must shift toward improving the durability of side branch interventions. For now, the stepwise provisional approach remains the most evidence-based path forward, offering equivalent LCx stability with lower overall procedural complexity and fewer reinterventions compared to upfront dual-stenting.
Funding and Registration
The EBC MAIN trial was supported by various institutional grants and research funds. ClinicalTrials.gov Identifier: NCT02497014.
References
1. Maznyczka A, et al. Patterns of Restenosis After Left Main Bifurcation Single- or Dual-Stenting: An EBC MAIN Trial Subanalysis. Circ Cardiovasc Interv. 2025;18(11):e015546.
2. Hildick-Smith D, et al. The European Bifurcation Club Left Main Study (EBC MAIN): 3-Year Outcomes of the Randomized Comparison of Provisional vs. Systematic Dual-Stenting Strategies for Left Main Bifurcation Lesions. European Heart Journal. 2023.
3. Lasson JF, et al. Percutaneous coronary intervention for coronary bifurcation disease: 15th consensus document from the European Bifurcation Club. EuroIntervention. 2021.