Introduction
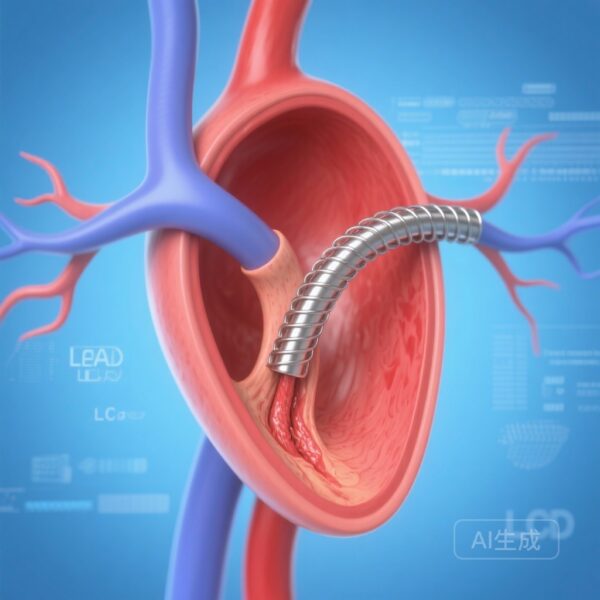
The management of coronary artery disease (CAD) in patients with diabetes mellitus remains one of the most significant challenges in interventional cardiology. Despite advancements in second-generation drug-eluting stents (DES), diabetic patients continue to experience higher rates of restenosis, stent thrombosis, and major adverse cardiovascular events (MACE) compared to their non-diabetic counterparts. This increased risk is driven by complex metabolic pathways that promote systemic inflammation, endothelial dysfunction, and a more aggressive neointimal proliferative response. The ABILITY Diabetes Global trial was designed to evaluate whether a novel stent technology, the Abluminus DES+, could improve outcomes in this high-risk population by enhancing drug delivery through a unique abluminal and balloon-surface coating.
Key Highlights
- The Abluminus DES+ failed to meet the primary non-inferiority endpoints for both ischemia-driven target-lesion revascularization (ID-TLR) and target-lesion failure (TLF) compared to the XIENCE everolimus-eluting stent.
- At 12 months, the rate of ID-TLR was significantly higher in the Abluminus group (4.8%) compared to the XIENCE group (2.1%).
- Safety outcomes, including target-vessel myocardial infarction, were also more frequent in the Abluminus group, although cardiovascular and all-cause mortality remained similar between groups.
- Landmark analyses between 12 and 24 months showed no significant divergence in event rates, suggesting the primary difference in performance occurs within the first year post-implantation.
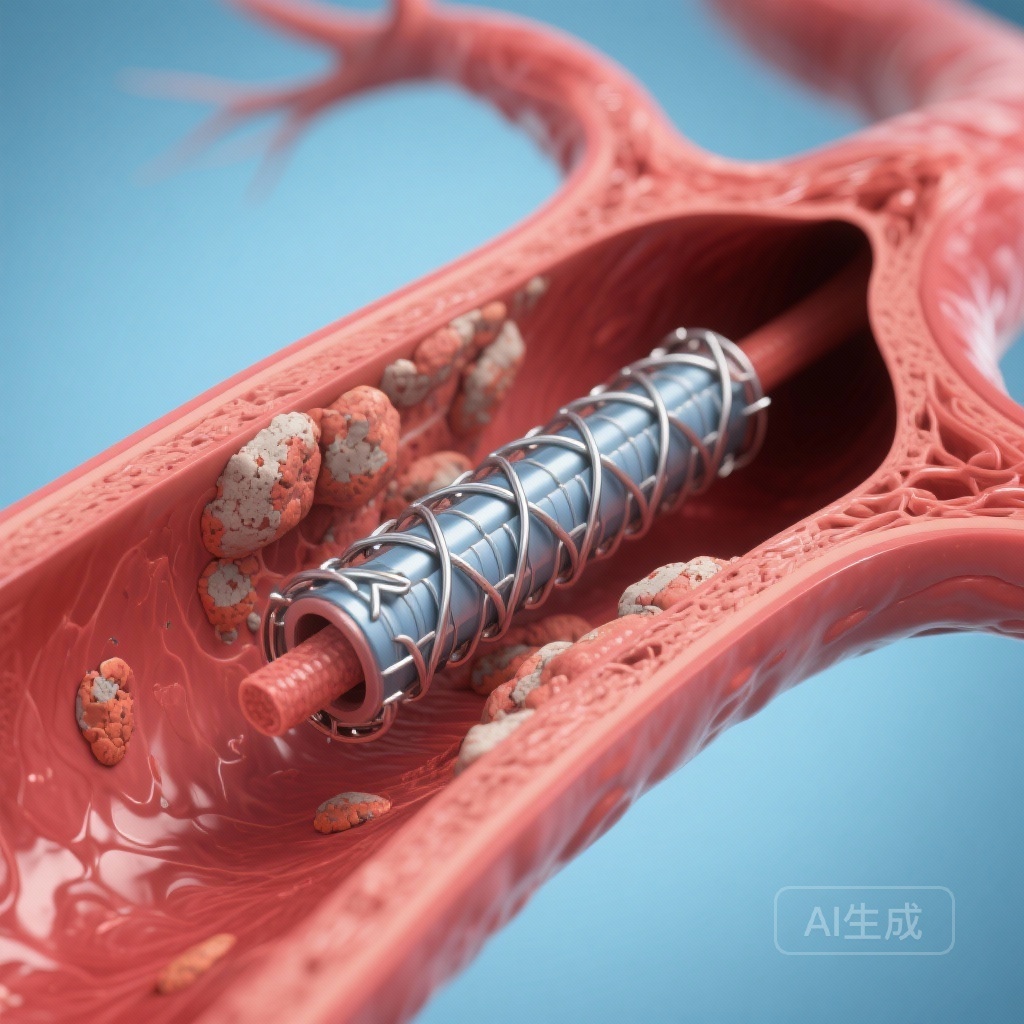
The Rationale for the Abluminus DES+ Technology
The Abluminus DES+ is a thin-strut cobalt-chromium sirolimus-eluting stent (SES). What distinguishes it from traditional DES is its hybrid coating technology: sirolimus is applied not only to the abluminal surface of the stent struts but also to the surface of the delivery balloon. This design is intended to provide a more uniform and comprehensive drug delivery to the vessel wall, including the areas between the stent struts (the ‘inter-strut’ zones). Theoretically, this approach should provide superior suppression of neointimal hyperplasia, which is particularly relevant in diabetic patients who often present with diffuse disease and smaller vessel calibers.
Study Design and Methodology
The ABILITY Diabetes Global trial was a large-scale, multicenter, prospective, randomized controlled trial conducted across 74 sites in 16 countries. The study enrolled 3,032 adults with type 1 or type 2 diabetes undergoing percutaneous coronary intervention (PCI) for de novo coronary lesions. Participants were randomized in a 1:1 ratio to receive either the Abluminus DES+ or the XIENCE EES, the latter of which features a durable polymer and is widely considered a gold standard in clinical practice.
Clinical Endpoints
The trial utilized two co-primary endpoints at 12 months, assessed in the per-protocol population:
1. Ischemia-driven target-lesion revascularization (ID-TLR):
Defined with a non-inferiority margin of 2.8%.
2. Target-lesion failure (TLF):
A composite of cardiovascular death, target-vessel myocardial infarction (TV-MI), or ID-TLR, with a non-inferiority margin of 3.0%.Operators were unmasked to the allocation due to the physical differences in the delivery systems, but clinical follow-up staff and the clinical events committee remained blinded to maintain the integrity of the data.
Detailed Findings and Statistical Analysis
The trial results were definitive in their rejection of the non-inferiority hypothesis. Between June 2020 and September 2022, 1,514 patients were assigned to Abluminus and 1,518 to XIENCE. The median age was 68 years, and 29% of the cohort was female.
Primary Endpoint Results at 12 Months
In the per-protocol analysis, the Abluminus DES+ group experienced an ID-TLR rate of 4.8% (67 patients), while the XIENCE EES group had a significantly lower rate of 2.1% (30 patients). The absolute risk difference was 2.7% (95% CI 1.3–4.1), which failed to meet the non-inferiority criterion (p=0.44).Similarly, for TLF, the Abluminus group reached 9.7% (137 patients) compared to 6.2% (89 patients) in the XIENCE group. The absolute risk difference was 3.5% (95% CI 1.5–5.5), again failing the non-inferiority test (p=0.68). Notably, for both co-primary endpoints, the lower bound of the 95% confidence interval for the risk difference excluded zero, indicating a statistically significant superiority of the XIENCE stent over the Abluminus stent.
Safety and Secondary Outcomes
The rate of target-vessel myocardial infarction was higher in the Abluminus group (5.2% vs. 3.1%). However, there were no statistically significant differences observed in cardiovascular death (2.9% vs. 2.1%) or all-cause death (3.7% vs. 3.3%). Long-term follow-up at 24 months mirrored these findings. Interestingly, landmark analyses performed between 12 and 24 months showed that the hazard curves for both groups remained parallel, suggesting that the excess risk associated with the Abluminus stent is concentrated in the early phase following the index procedure.
Expert Commentary and Clinical Interpretation
The failure of the Abluminus DES+ to achieve non-inferiority against the XIENCE EES in this specific population raises several important questions regarding stent design and drug delivery kinetics. While the concept of balloon-surface coating is innovative, the clinical application may be more complex than anticipated.
Mechanistic Considerations
One possible explanation for the findings relates to the drug delivery mechanism. The protocol recommended a balloon inflation time of at least 45 seconds to facilitate drug transfer from the balloon to the vessel wall. In a real-world clinical setting, achieving consistent and effective drug transfer across diverse lesion morphologies—especially calcified or fibrotic lesions common in diabetic patients—may be inconsistent. Furthermore, the XIENCE EES utilizes a fluorinated durable polymer that has been optimized over decades to provide controlled drug release and high biocompatibility, set against which any new technology faces a very high bar.
Context within Existing Literature
The results of ABILITY Diabetes Global contrast with some smaller studies that suggested potential benefits for drug-coated balloons or hybrid systems. However, when compared to the broader landscape of DES trials in diabetes, such as the SUGAR trial or the TUXEDO-India trial, it becomes clear that the durable-polymer EES remains a formidable comparator. The findings underscore that ‘more drug’ or ‘different delivery’ does not automatically translate to ‘better outcomes’ if the platform or the elution profile is not perfectly optimized for the diabetic vascular environment.
Conclusion
The ABILITY Diabetes Global trial provides high-quality evidence that the Abluminus DES+ is not non-inferior to the XIENCE EES in patients with diabetes. The higher rates of TLR and TLF observed with the Abluminus stent suggest that the XIENCE EES should remain the preferred choice for this high-risk patient subset. This trial highlights the persistent difficulty in improving outcomes for diabetic patients undergoing PCI and serves as a reminder that innovative technologies must be rigorously validated against established standards before widespread clinical adoption. Future research should focus on further refining stent polymers and exploring adjunctive pharmacotherapies to address the residual ischemic risk that remains prevalent in the diabetic population.
Funding and Trial Registration
This trial was funded by Concept Medical. It is registered with ClinicalTrials.gov under the identifier NCT04236609.
References
1. Abizaid A, Mehran R, et al. Abluminus DES+ sirolimus-eluting stent versus everolimus-eluting stent in patients with diabetes and coronary artery disease (ABILITY Diabetes Global): results from a multicentre, randomised controlled trial. Lancet. 2026 Jan 17;407(10525):227-236. doi: 10.1016/S0140-6736(25)02157-9.
2. Kedhi E, et al. Second-generation everolimus-eluting stents versus first-generation paclitaxel-eluting stents in patients with diabetes: a patient-level pooled analysis. Lancet. 2010;375(9710):201-209.
3. Kaul U, et al. Everolimus-Eluting Stents or Sirolimus-Eluting Stents in Patients with Diabetes Mellitus. N Engl J Med. 2015;373(18):1709-1719.