Highlights
– The STRIDES trial evaluated four common interventions for preventing vasovagal reactions (VVR) in the largest study of its kind, involving 1.4 million donors and over 4.1 million donations.
– None of the tested interventions—500 mL isotonic drinks, 3-minute post-donation rest, modified applied muscle tension (AMT), or psychosocial preparatory materials—showed a significant reduction in syncope with loss of consciousness compared to standard care.
– The absolute event rate for the primary outcome was remarkably stable at approximately 10.5 to 10.7 per 10,000 donations, regardless of the intervention arm.
– These findings suggest that in high-resource settings with established safety protocols, incremental additions to donor care may provide negligible benefit, offering an opportunity to streamline blood service operations.
Background: The Burden of Vasovagal Reactions
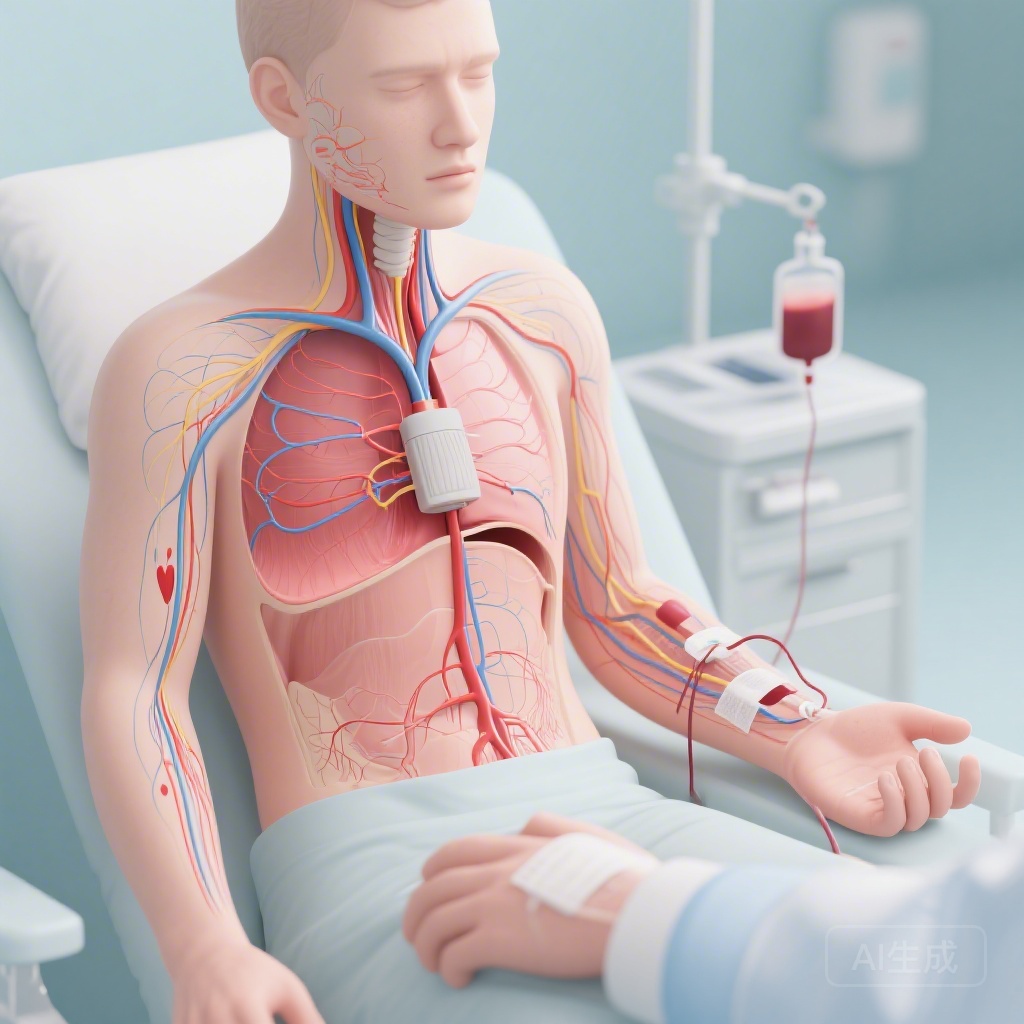
Vasovagal reactions (VVR) remain the most frequent acute systemic complication associated with whole blood donation. These reactions, characterized by a sudden drop in heart rate and blood pressure, range from mild symptoms like lightheadedness and nausea to severe episodes involving loss of consciousness (syncope), seizures, or physical injury due to falls. For blood services worldwide, VVRs are more than a clinical concern; they represent a significant barrier to donor retention, as a negative experience often discourages donors from returning. Furthermore, severe reactions incur substantial medicolegal costs and require immediate clinical intervention, disrupting the flow of donation centers.
Over the years, various blood services have implemented a range of preventive strategies. These include pre-donation hydration, muscle tension exercises, and psychological support. However, many of these practices were adopted based on small-scale physiological studies or pilot trials that lacked the statistical power to definitively prove efficacy in a real-world, high-volume setting. The STRIDES trial was designed to provide high-level, evidence-based clarity on whether these interventions truly provide added value over current standard practices in a large-scale national service.
Study Design: The STRIDES Trial Framework
The STRIDES trial (STrategies to Reduce vAsovagal Reactions in Blood Donors) was a massive cluster-randomised, stepped-wedge, crossover trial conducted across 73 blood donation sites in England. The study’s scale is unprecedented in the field of transfusion medicine, capturing data from 1,379,095 donors who made a total of 4,134,712 donations between November 2019 and November 2022.
The Stepped-Wedge Crossover Approach
The trial utilized a sophisticated design where each donation site (cluster) was randomly allocated to a sequence for implementing one or more of the four interventions over four distinct nine-month periods. This design allowed for both between-site and within-site comparisons while maintaining operational feasibility across a national network. To minimize carry-over effects and ensure robust data, the trial incorporated factorial design elements. The primary endpoint was defined as an in-session vasovagal reaction with loss of consciousness (LOC), which is considered the most clinically significant and objective measure of a severe reaction.
The Four Interventions Evaluated
The trial tested four specific interventions against the standard practices currently employed by NHS Blood and Transplant (NHSBT) in England:
1. Isotonic Drink: Donors were provided with a 500 mL isotonic drink prior to donation, compared with the standard practice of 500 mL of plain water.
2. Extended Chair Rest: Donors were required to remain in the donation chair for 3 minutes post-procedure, an increase from the standard 2-minute rest period.
3. Modified Applied Muscle Tension (AMT): Donors were taught a modified version of AMT exercises, compared to the current AMT instructions already in use.
4. Psychosocial Intervention: Donors were provided with preparatory psychosocial materials designed to reduce anxiety and manage expectations, compared to receiving no such specific materials.
Key Findings: A Neutral Result with High Precision
The results of the STRIDES trial provide a clear, albeit neutral, answer to the efficacy of these interventions. Despite the massive sample size, the study found no evidence that any of the four interventions significantly outperformed standard practices.
Primary Outcome: Syncope with Loss of Consciousness
The primary outcome—vasovagal reactions with loss of consciousness—occurred 4,388 times across the 4.1 million donations. The statistical analysis, conducted on an intention-to-treat basis, yielded a joint p-value of 0.21, indicating that the interventions as a whole did not have a significant effect.
The individual odds ratios (OR) for each intervention were as follows:
– Isotonic drink: OR 0.98 (95% CI 0.92–1.04)
– Extended chair rest: OR 0.99 (95% CI 0.92–1.06)
– Modified AMT: OR 1.12 (95% CI 1.00–1.26)
– Psychosocial intervention: OR 1.03 (95% CI 0.93–1.14)
Notably, the modified AMT intervention showed a trend toward an increase in reactions, although the lower bound of the confidence interval rested at 1.00. The absolute event rates were 10.7 per 10,000 donations in the control groups and 10.5 per 10,000 in the intervention groups, a difference that is clinically negligible.
Secondary Outcomes
The findings for total in-session vasovagal reactions (including those without loss of consciousness) mirrored the primary results. While the absolute event rates for total VVRs were higher (60,517 total reactions), none of the interventions demonstrated a clear or consistent benefit in reducing these milder episodes compared to standard care.
Critical Interpretation and Expert Commentary
The neutrality of the STRIDES trial results is significant for several reasons. In clinical research, a large-scale neutral trial is often as informative as one with a positive result, particularly when it challenges established but poorly evidenced practices.
The Ceiling Effect in Standard Care
One plausible explanation for the lack of additional benefit is the “ceiling effect.” The current standard of care in England—which already includes pre-donation water, 2-minute rest, and basic muscle tension—may already be achieving the maximum possible reduction in VVRs that can be reached through these types of simple behavioral or dietary interventions. Once a certain threshold of safety is met, incremental changes like adding electrolytes to the water or extending rest by sixty seconds may not offer enough physiological leverage to further reduce the incidence of syncope.
Biological Plausibility vs. Practical Efficacy
Physiologically, isotonic drinks are known to expand plasma volume more effectively than plain water in some contexts, and extended rest should theoretically allow for better orthostatic adjustment. However, the STRIDES trial highlights the gap between small-scale physiological changes and broad clinical outcomes. In the complex environment of a blood donation center, where psychological factors, donor fatigue, and individual biological variability all play roles, these subtle physiological interventions may be drowned out by other variables.
Study Strengths and Limitations
The primary strength of this study is its sheer scale and the pragmatic nature of the design. By using an opt-out consent model and integrating the trial into daily operations, the researchers achieved a level of generalizability that is rarely seen. However, the study does have limitations. As a cluster-randomised trial, there is always a risk of site-level confounding, although the stepped-wedge crossover design was specifically chosen to mitigate this. Additionally, the study was conducted within a single national health system (NHS England), and while the results are likely applicable to other high-resource settings, they may not translate directly to regions where standard donor care is less robust.
Conclusion and Global Policy Implications
The STRIDES trial provides a powerful evidence base for blood services globally to evaluate their own preventive protocols. The lack of clear benefit from these four interventions suggests that blood services can safely focus on streamlining their operations rather than adding more complex or time-consuming preventive steps.
For instance, the finding that a 3-minute rest provides no advantage over a 2-minute rest has direct implications for donor throughput and chair utilization. Similarly, the lack of benefit from isotonic drinks over plain water allows services to avoid the higher costs and logistical requirements of stocking specialized beverages. By simplifying donation practices and removing ineffective interventions, blood services can save significant resources without compromising donor safety. The focus should now shift toward identifying high-risk donors through predictive modeling and perhaps investigating more targeted interventions for those specific individuals, rather than applying broad measures to the entire donor population.
Funding and Clinical Trial Information
This research was funded by NHS Blood and Transplant and the NIHR Blood and Transplant Research Unit in Donor Health and Behaviour. The trial is registered with ISRCTN (ISRCTN 10412338).
References
1. Kaptoge S, McMahon A, Wu Y, et al. Preventive interventions for vasovagal reactions in whole blood donors: a cluster-randomised, stepped-wedge, crossover trial of 73 sites involving 1.4 million donors in England. Lancet Haematol. 2026 Feb;13(2):e64-e73. doi: 10.1016/S2352-3026(25)00319-9.
2. Thijssen DH, et al. Applied muscle tension: a review of its effectiveness in preventing vasovagal reactions. Blood. 2014;123(21):3352-3360.
3. Newman BH. Donor-related adverse events of blood donation. Transfus Med Rev. 2004;18(3):193-207.