Introduction: Challenging the Long-Standing Surgical Paradigm
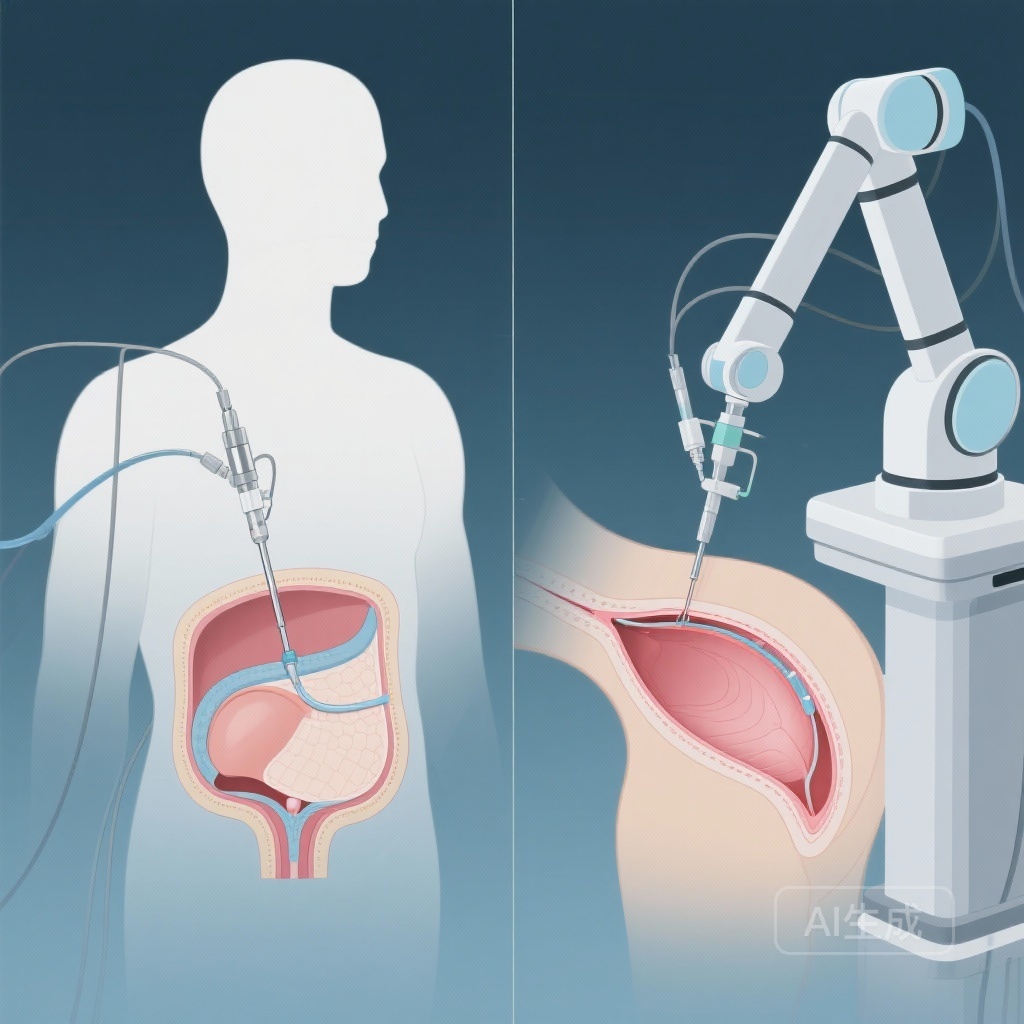
The selection of the surgical route for hysterectomy in benign cases has long been guided by a clear hierarchy. For decades, the American College of Obstetricians and Gynecologists (ACOG) and the Society of Gynecologic Surgeons (SGS) have recommended vaginal hysterectomy (VH) as the preferred approach whenever feasible. This recommendation was largely rooted in data from the late 1990s and early 2000s, suggesting that VH offered the fastest recovery, lowest cost, and fewest complications compared to the traditional abdominal route or early laparoscopic techniques. However, the surgical landscape has shifted dramatically. With the maturation of laparoscopic technology and the widespread adoption of robotic-assisted platforms, the relative advantages of the vaginal route have come under renewed scrutiny. A contemporary analysis published in the American Journal of Obstetrics and Gynecology by Meyer et al. (2025) provides a critical update to this debate, suggesting that the vaginal route may no longer hold a clear clinical advantage over laparoscopic approaches.
Study Design and Methodology
To evaluate contemporary outcomes, researchers conducted a massive cohort study using data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, spanning from 2012 to 2022. This database is renowned for its prospectively collected, high-quality clinical data, making it a robust source for assessing short-term surgical outcomes.
Population and Inclusion Criteria
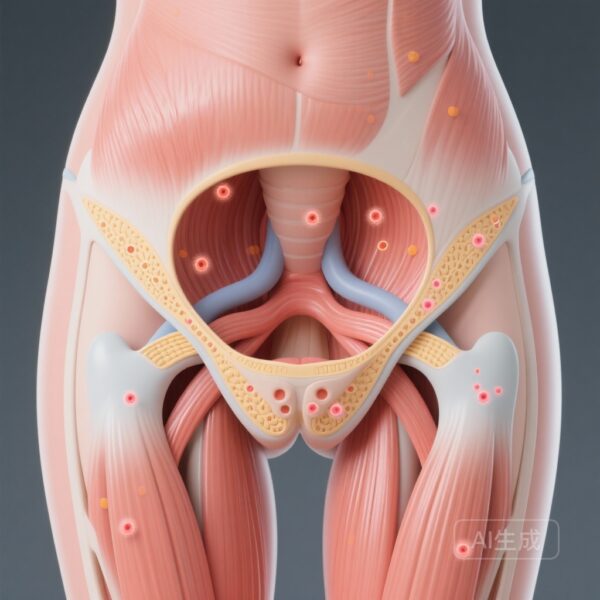
The study focused on women undergoing hysterectomy for benign indications. To ensure a fair comparison, the researchers excluded abdominal hysterectomies, supracervical procedures, and emergent surgeries. The primary comparison was between Vaginal Hysterectomy (VH) and Laparoscopic/Robotic Hysterectomy (LH).
Statistical Rigor: Propensity Score Matching
Given the inherent biases in surgical route selection (where VH might be chosen for smaller uteri or patients with higher pelvic organ prolapse), the study utilized propensity score matching (PSM). This technique paired patients in a 1:1 ratio based on demographics, comorbidities, uterine weight (stratified at 250 g), and whether concomitant procedures were performed. This resulted in a well-balanced cohort of 83,436 women (41,718 per group).
Endpoints
The primary endpoint was the occurrence of any complication within 30 days of surgery, classified by the Clavien-Dindo system. Secondary endpoints included operative duration, the necessity of overnight admission, and the total length of hospital stay (LOS).
Key Findings: A Shift in the Safety Profile
The results of this decade-long analysis present a compelling challenge to the traditional ‘vaginal-first’ mantra. While complication rates remained low in both groups—a testament to the safety of modern minimally invasive gynecology—the laparoscopic route demonstrated a statistically significant advantage in several key areas.
Overall Complications
Postoperative complications occurred in 8.2% of the VH group compared to 6.4% in the LH group. After adjusting for confounding variables, the vaginal route was associated with a 23% increase in the odds of experiencing a complication (Adjusted Odds Ratio [aOR], 1.23; 95% CI, 1.15-1.31). This finding is particularly striking because it contradicts earlier meta-analyses that frequently cited VH as the safer option.
Specific Morbidities
The risk profile differed significantly between the two routes:VH was associated with higher risks of:
LH was associated with higher risks of:
The higher rate of UTIs and infections in the VH group may be related to the inherent nature of the vaginal surgical field and potential differences in catheterization protocols. Conversely, the increased risk of PE in the laparoscopic group likely stems from the physiological impact of pneumoperitoneum and the trend toward longer operative times.
Operative Efficiency vs. Hospital Stay
One area where VH maintained its traditional advantage was operative time. On average, vaginal hysterectomies were completed in 109.6 minutes, compared to 137.0 minutes for laparoscopic procedures (P < .001). However, this surgical efficiency did not translate into a shorter hospital stay.The study found that patients undergoing VH were more likely to require longer hospitalizations:
Expert Commentary: Interpreting the Data
The results of this study are likely to spark significant debate within the gynecologic surgery community. For years, surgeons have been taught that VH is the ‘ultimate’ minimally invasive procedure because it avoids all abdominal incisions. However, these data suggest that the ‘incisionless’ nature of VH may be offset by other factors.
The ‘Lost Art’ of Vaginal Hysterectomy
One potential explanation for the rising complication rates in VH is the ‘volume-outcome’ relationship. As laparoscopic and robotic training has become the cornerstone of residency programs, the volume of vaginal hysterectomies has declined. This reduction in volume may lead to a decrease in surgical proficiency, potentially explaining the higher rates of organ/space infections and reoperations seen in the VH cohort.
Technological Evolution
Laparoscopic surgery has benefited from massive technological investments over the last decade, including 4K visualization, advanced vessel-sealing devices, and robotic precision. These advancements allow for meticulous hemostasis and clear anatomical identification, which may explain the lower transfusion and infection rates compared to VH, where much of the dissection is performed with limited direct visualization.
Limitations and Context
It is important to acknowledge the limitations of this study. While NSQIP provides excellent 30-day data, it does not capture long-term outcomes such as pelvic organ prolapse or sexual function. Furthermore, the database does not specify the reason for the surgical route choice, which can be influenced by surgeon preference or institutional culture.
Conclusion: Moving Toward Individualized Selection
The analysis by Meyer et al. indicates that the gap between vaginal and laparoscopic hysterectomy has not only closed but may have shifted in favor of laparoscopy regarding short-term complications and length of stay. While vaginal hysterectomy remains a valuable and efficient tool—particularly in cases of significant prolapse or when avoiding abdominal entry is paramount—it should no longer be viewed as the default ‘superior’ route for all benign indications.Modern surgical practice should move toward a more nuanced, individualized approach. The data suggest that laparoscopic hysterectomy is a highly safe and effective alternative that may offer superior postoperative recovery profiles for many women. Further prospective trials are needed to refine these findings and perhaps update national guidelines to reflect the realities of contemporary surgical practice.
References
Meyer R, Hamilton KM, Ezike O, et al. Vaginal hysterectomy vs laparoscopic hysterectomy for benign indications: complications and length of stay in a national analysis of contemporary data. Am J Obstet Gynecol. 2025;232(4):S0002-9378. doi:10.1016/j.ajog.2025.10.027.