Highlights
- GBD 2021 estimates 31,780 incident primary CNS cancers in the US in 2021; age-standardized incidence was 6.91 per 100,000 (95% UI 6.58–7.12).
- Between 1990 and 2021, incidence remained essentially unchanged, while age-standardized mortality fell 8.4% and DALYs declined 15.8%, consistent with improved survival and/or reduced disability.
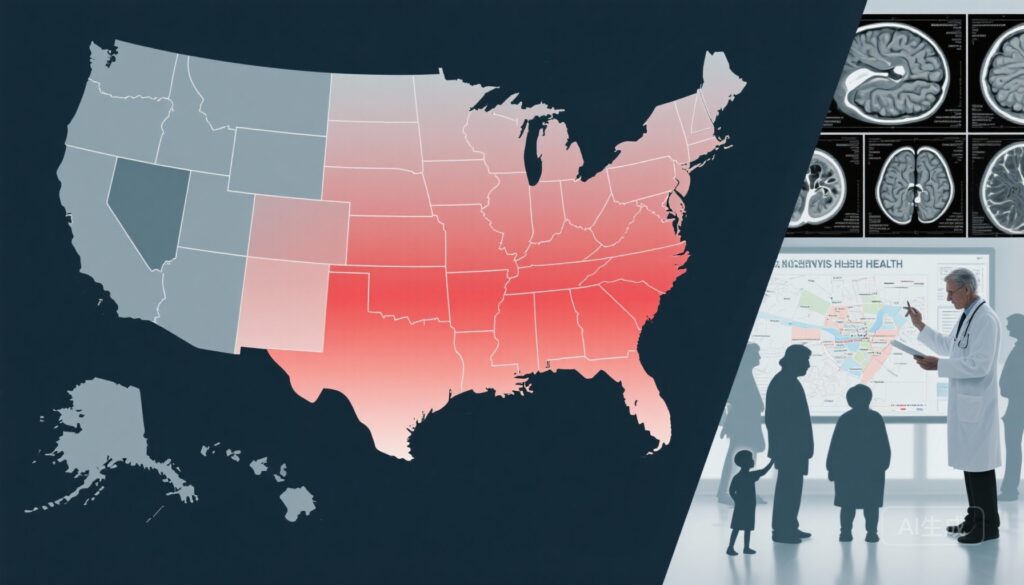
- Marked geographic and socioeconomic disparities persist: higher burdens concentrated in Mississippi, Alabama, Kentucky, West Virginia, and certain Midwest divisions; DALYs and mortality inversely correlated with SDI (ρ ≈ -0.64 to -0.69).
- Age-specific trends diverge: notable reductions in incidence for children 70 years); burden remains higher in males.
Background
Primary tumors of the brain and central nervous system (collectively CNS cancers) account for approximately 2% of all cancers worldwide but are disproportionately impactful due to high mortality, potential for profound neurologic disability, and intensive resource needs for diagnosis, therapy, and survivorship care. CNS tumors include biologically heterogeneous entities (e.g., gliomas, meningiomas, CNS lymphomas, embryonal tumors) with distinct age distributions, prognoses, and treatment paradigms. Reliable, geographically granular burden estimates are essential to inform workforce planning, regional referral systems, research prioritization, and equitable delivery of high-complexity neuro-oncologic care.
The Global Burden of Disease (GBD) Study provides model-based, comparable estimates across conditions, locations, and time. The GBD 2021 United States CNS cancer analysis (Han et al., JAMA Neurol. 2025) updated estimates through 2021, enabling nuanced assessment of temporal trends, state-level variation, age and sex patterns, and relationships with the Sociodemographic Index (SDI).
Study design
This cross-sectional, repeated analysis used GBD 2021 methods applied to US-specific data. Key features:
- Data sources: 183 inputs spanning cancer registries, vital records, and other datasets harmonized by GBD investigators.
- Population: United States residents of all ages and both sexes; estimates provided at national and state/division levels from 1990–2021.
- Outcomes: Incidence, prevalence, mortality, disability-adjusted life-years (DALYs), years of life lost (YLLs), and years lived with disability (YLDs), presented as overall and age-standardized rates per 100,000 with 95% uncertainty intervals (UIs).
- Analytic approach: GBD standard cause-of-death modeling, incidence-prevalence-mortality reconciliation, and redistribution of ill-defined causes where appropriate; correlation analyses with SDI to assess social gradients.
- Therapeutic advances: more effective surgical techniques, adoption of multimodality therapy (e.g., temozolomide for glioblastoma, precision radiotherapy), and improved supportive care lowering perioperative and treatment-related mortality.
- Diagnostic improvements: higher-resolution neuroimaging leading to earlier detection and diagnosis of less advanced disease in some age groups, or conversely increases in detection among the elderly.
- Changes in histologic mix captured only partially by aggregate CNS-cancer metrics — declining high-mortality histologies or relative increases in less aggressive subtypes could shift aggregate mortality downward even if overall incidence remains stable.
- Health system factors: better post-diagnostic care networks and survivorship services in higher-SDI areas versus persistent access gaps in lower-SDI states.
- Aggregation heterogeneity: GBD aggregates all primary CNS cancers. Different trends by histology (e.g., gliomas vs meningiomas vs embryonal tumors) are clinically crucial but not fully resolved in the headline estimates. Histology- and molecular-level surveillance remains essential.
- Modeling assumptions: GBD uses statistical redistribution and modeling to fill registry gaps; estimates therefore carry uncertainty dependent on input data quality and coding practices over time and across states.
- Data lag and external influences: The study extends through 2021; pandemic-related disruptions in care pathways and diagnostics may have transient or long-term effects not fully captured or separable from secular trends.
- Attribution limitations: Correlation with SDI does not prove causation; unmeasured confounders (e.g., environmental exposures, local referral networks) could explain some spatial patterns.
- Persistently high-burden states warrant proactive outreach, regional multidisciplinary tumor boards, and referral pathways to improve timeliness and quality of neuro-oncology care.
- Vulnerable age cohorts—particularly older adults with rising incidence—need tailored diagnostic algorithms and geriatric-informed treatment decision-making to balance efficacy and quality of life.
- Targeted resource allocation is needed to strengthen neurosurgical and neuro-oncology capacity in lower-SDI regions, including telemedicine-enabled tumor boards and hub-and-spoke models.
- Investments in registry completeness and histology/molecular reporting at the state level will improve surveillance precision and permit more actionable, subtype-specific interventions.
- Public-health interventions should address upstream determinants (access to care, insurance coverage, transportation, and social support) that likely mediate the SDI–outcome relationship.
- Histology- and molecular-specific time-trend analyses using high-quality registry data (e.g., SEER, CBTRUS) are needed to clarify drivers of aggregate changes.
- Mixed-methods studies exploring barriers to specialized care in high-burden states would inform pragmatic interventions to reduce disparities.
- Han HJ, Kim YS, Park S, et al; GBD 2021 US CNS Cancer Collaborators. Burden of Central Nervous System Cancer in the United States, 1990-2021. JAMA Neurol. 2025 Nov 3:e254286. doi:10.1001/jamaneurol.2025.4286.
- Central Brain Tumor Registry of the United States (CBTRUS). Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2014–2018. CBTRUS, 2021. (Access via cbtrus.org)
- Murray CJL, Aravkin AY, Zheng P, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222.
- Ostrom QT, Gittleman H, Truitt G, et al. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016. Neuro-Oncology. 2019;21(Suppl 5):v1–v100.
- National Comprehensive Cancer Network. NCCN Guidelines for Central Nervous System Cancers. Available at: nccn.org (access current guideline versions for treatment recommendations).
GBD aggregates primary CNS cancers rather than presenting histology-specific time trends in full detail, which is an important methodological caveat when interpreting drivers of change.
Key findings
Overall burden and temporal trends
In 2021, the United States experienced an estimated 31,780 incident cases of primary CNS cancer (95% UI 29,971.1–32,843.9). The age-standardized incidence rate was 6.91 per 100,000 (95% UI 6.58–7.12). Age-standardized DALYs and mortality rates were 134.38 (95% UI 129.83–137.95) and 4.1 (95% UI 3.87–4.22) per 100,000, respectively.
From 1990 to 2021, the age-standardized incidence did not change significantly overall, but there were meaningful declines in disease burden: DALYs decreased by 15.77% (95% UI -17.75% to -13.68%) and mortality decreased by 8.41% (95% UI -11.09% to -6.22%). These reductions likely reflect a combination of improved diagnosis, better perioperative and oncologic care, and changes in the distribution of tumor subtypes and age structure.
Geographic heterogeneity
Substantial interstate and divisional variability was identified. Persistently higher burdens were concentrated in the southeastern states and some central divisions, notably: Mississippi, Alabama, Kentucky, and West Virginia, along with West North Central and East South Central divisions (e.g., Kansas and neighboring states highlighted in the GBD report). These higher-burden areas showed elevated age-standardized mortality and DALYs over the past three decades.
Potential contributors include socioeconomic disadvantage, limited access to specialized neurosurgical and neuro-oncology centers, delayed diagnosis, and regional differences in comorbidities and environmental exposures; disentangling these requires further local-level study.
Age and sex patterns
The burden displays a bimodal age distribution. Young children (70 years) showed increasing incidence trends. This pattern reflects heterogeneous etiologies: declines in certain pediatric tumor categories (possibly due to diagnostic/registry effects or genuine epidemiologic change) and increased detection or true rises in tumors among the elderly, where age-related susceptibility and cumulative exposures may play roles.
Sex differences are consistent and persistent: males carried a higher disease burden than females across most metrics. The male predominance aligns with established epidemiology for several aggressive CNS tumor types (e.g., high-grade gliomas), whereas some tumor classes (e.g., meningiomas) are more common in females, underscoring the value of histology-specific surveillance.
Socioeconomic correlation
GBD investigators quantified the relationship between SDI and CNS cancer outcomes: DALYs and mortality rates were negatively correlated with SDI (ρ = -0.6860 and ρ = -0.6391, P < .001). In other words, states with lower SDI experienced higher mortality and disability from CNS cancers. This strong inverse relationship highlights the social determinants of neuro-oncologic outcomes and supports prioritization of disadvantaged regions for capacity-building and access interventions.
Interpretation and plausible drivers
The stability of incidence with concurrent declines in mortality and DALYs suggests improved survival or reduced disease severity at population scale rather than decreases in new disease occurrence. Contributing factors may include:
Expert commentary and limitations
Expert observers would note the strengths of this analysis: comprehensive data synthesis, standardized metrics enabling temporal and geographic comparisons, and attention to SDI gradients that inform policy. However, several important limitations temper interpretation:
Guideline context: The observed mortality declines are broadly consistent with incremental improvements recommended in neuro-oncology practice guidelines (e.g., NCCN CNS Tumors Guidelines) emphasizing evidence-based multimodal therapy and referral to specialized centers. To maximize population impact, guidelines must be paired with implementation strategies to reduce the observed geographic and socioeconomic gaps.
Implications for clinicians, health systems, and policy
For clinicians:
For health systems and policymakers:
For researchers:
Conclusion
The GBD 2021 US CNS cancer analysis provides a nuanced portrait: stable national incidence with meaningful declines in mortality and DALYs, yet persistent and important geographic, age, sex, and socioeconomic disparities. These findings argue for dual strategies: maintain and accelerate population-level advances in diagnosis and therapy while prioritizing targeted investments to close geographic and SDI-related gaps. Improving histology- and molecular-level surveillance, strengthening regional neuro-oncology networks, and implementing context-sensitive access solutions are practical next steps to convert declining mortality into equitable gains in population health.
Funding and clinicaltrials.gov
Funding: See the original GBD 2021 US CNS Cancer Collaborators publication (Han et al., JAMA Neurol. 2025) for detailed funding declarations. The broader Global Burden of Disease initiative has historically received support from multiple sources, including academic institutions and philanthropic organizations such as the Bill & Melinda Gates Foundation through the Institute for Health Metrics and Evaluation.
ClinicalTrials.gov: Not applicable to the GBD observational modeling study. Individual clinical interventions referenced are evaluated in clinical trials cataloged on ClinicalTrials.gov; clinicians should consult that registry for active therapeutic studies in CNS tumors.