Highlights
- ICP-332, a highly selective Tyrosine Kinase 2 (TYK2) inhibitor, achieved superior EASI-75 responses (64%) compared to placebo (8%) at just 4 weeks.
- Treatment led to a remarkable 78.2% reduction in EASI scores for the 80-mg cohort, signaling rapid clinical onset.
- The safety profile was characterized by mild-to-moderate treatment-emergent adverse events (TEAEs), with no reported severe systemic complications typical of non-selective JAK inhibitors.
- Selective TYK2 inhibition represents a targeted therapeutic strategy that may bypass the hematologic and metabolic side effects associated with pan-JAK inhibition.
Background
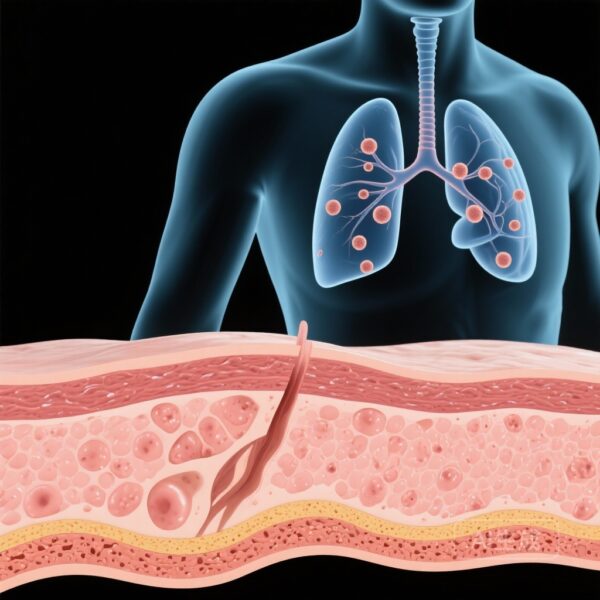
Atopic dermatitis (AD) is a chronic, relapsing inflammatory skin disease characterized by intense pruritus, impaired skin barrier function, and a complex immune-mediated pathogenesis. The standard of care for moderate to severe AD has evolved from broad immunosuppressants to targeted biologics (e.g., dupilumab, tralokinumab) and oral Janus kinase (JAK) inhibitors (e.g., abrocitinib, upadacitinib). However, while pan-JAK inhibitors are highly effective, their inhibition of JAK1, JAK2, and JAK3 pathways can lead to off-target effects, including cytopenias, lipid elevations, and an increased risk of venous thromboembolism (VTE).
Tyrosine kinase 2 (TYK2) is a member of the JAK family that specifically mediates signaling for interleukin (IL)-12, IL-23, and Type I interferons (IFN). Crucially, TYK2 does not participate in the signaling of IL-2, IL-4, or erythropoietin, which are mediated by other JAK isoforms. By selectively targeting TYK2, ICP-332 aims to inhibit the pro-inflammatory cascades central to AD while minimizing the systemic risks associated with broader JAK inhibition. This review analyzes the recently published Phase 2 data (NCT05702268) regarding ICP-332’s clinical utility.
Key Content
Study Design and Patient Population
The randomized, double-blind, placebo-controlled Phase 2 trial was conducted across 19 specialized centers in China. The study enrolled 75 adults (18–75 years) with a confirmed diagnosis of moderate to severe AD for at least one year. Participants were required to have a history of inadequate response to topical therapies. Baseline characteristics showed a mean age of 37–44 years and a male predominance (72%). Patients were randomized in a 1:1:1 ratio to receive either 80 mg ICP-332, 120 mg ICP-332, or a placebo once daily for 4 weeks.
Efficacy Outcomes: Rapid and Robust Response
The efficacy of ICP-332 was evaluated primarily through the Eczema Area and Severity Index (EASI). At the 4-week mark, both dose groups showed statistically significant and clinically meaningful improvements over placebo:
- Percentage Change in EASI: The 80-mg group achieved a -78.2% reduction, and the 120-mg group achieved a -72.5% reduction, compared to a modest -16.7% in the placebo arm (P < .001).
- EASI-75 Achievement: 64.0% of patients in both the 80-mg and 120-mg groups reached EASI-75, representing a 56.0% difference over placebo.
- Investigator Global Assessment (vIGA-AD): Success (score of 0 or 1 with ≥2-point improvement) was significantly higher in the 80-mg group (36.0%) vs. placebo (4.0%; P = .005).
Notably, the 80-mg dose appeared slightly more effective than the 120-mg dose in certain parameters, suggesting that maximum efficacy may be reached at lower dosing thresholds, or reflecting the small sample size limitations of Phase 2 studies.
Safety and Tolerability Profile
The primary outcome of this trial was safety. TEAEs occurred in 76% of the 80-mg group and 75% of the 120-mg group, compared to 68% in the placebo group. Key observations included:
- Severity: All adverse events were categorized as mild (Grade 1) or moderate (Grade 2). No serious adverse events (SAEs) or deaths were reported.
- Common Adverse Events: The most frequent laboratory abnormality was a decrease in blood fibrinogen (44% in the 80-mg group, 21% in the 120-mg group). This finding warrants further investigation in larger cohorts to determine clinical relevance regarding coagulation.
- Absence of Class-Related Risks: Importantly, the trial did not observe cases of herpes zoster, tuberculosis, major adverse cardiovascular events (MACE), or VTE during the 4-week treatment window.
Expert Commentary
Mechanistic Selectivity and Clinical Implications
The results for ICP-332 are highly encouraging, particularly when viewed through the lens of “selectivity.” By inhibiting TYK2, ICP-332 modulates the IL-23/Th17 axis and IFN-α signaling, which are increasingly recognized as contributing factors in AD alongside the traditional Th2 pathway. The efficacy data rivals that of established JAK1 inhibitors like upadacitinib, yet the 4-week safety profile suggests a cleaner signature, likely due to the avoidance of JAK2 and JAK3 inhibition.
Controversies and Limitations
A primary point of discussion is the decrease in blood fibrinogen. While common in this trial, the mechanism linking TYK2 inhibition to fibrinogen levels is not yet fully elucidated, and it remains to be seen if this poses a long-term risk for bleeding or if it is a transient, non-consequential laboratory finding. Furthermore, the 4-week duration is extremely short for a chronic condition like AD. Longitudinal data are essential to confirm the durability of response and to monitor for delayed-onset toxicities or infectious risks.
Comparison with Deucravacitinib
As deucravacitinib (the first approved TYK2 inhibitor for psoriasis) has shown, this class offers a distinct safety profile compared to pan-JAK inhibitors. ICP-332’s performance in AD suggests that TYK2 inhibition may be a cross-indication strategy for multiple T-cell mediated skin diseases. However, head-to-head trials against dupilumab or JAK1 inhibitors would be necessary to define its exact place in the treatment algorithm.
Conclusion
The Phase 2 trial of ICP-332 demonstrates that selective TYK2 inhibition is a potent and generally well-tolerated approach for managing moderate to severe atopic dermatitis. With EASI reductions exceeding 70% within one month, ICP-332 stands as a promising candidate for Phase 3 development. Future research must focus on long-term safety, the clinical significance of fibrinogen changes, and the drug’s efficacy in diverse global populations beyond the initial Chinese cohort.
References
- Xu J, Zhang L, Liang Y, et al. Safety and Efficacy of ICP-332 for Moderate to Severe Atopic Dermatitis: A Phase 2 Randomized Clinical Trial. JAMA Dermatol. 2026 Jan 14. doi: 10.1001/jamadermatol.2025.5295. PMID: 41533373.
- Armstrong AW, et al. Deucravacitinib in Plaque Psoriasis: 2-Year Results From the Phase 3 POETIC Trials. J Am Acad Dermatol. 2023.
- Bieber T. Atopic dermatitis: an expanding therapeutic pipeline for a complex disease. Nat Rev Drug Discov. 2022;21(1):21-40.