Highlight
The addition of tiragolumab, an anti-TIGIT monoclonal antibody, to atezolizumab and chemotherapy resulted in a confirmed objective response rate (ORR) of 67.7%, compared to 53.8% for atezolizumab plus chemotherapy and 47.8% for chemotherapy alone.
The triple-drug combination maintained a manageable safety profile, with grade 3-4 adverse events occurring at rates similar to the doublet and chemotherapy-only arms (79% vs 80% and 74%, respectively).
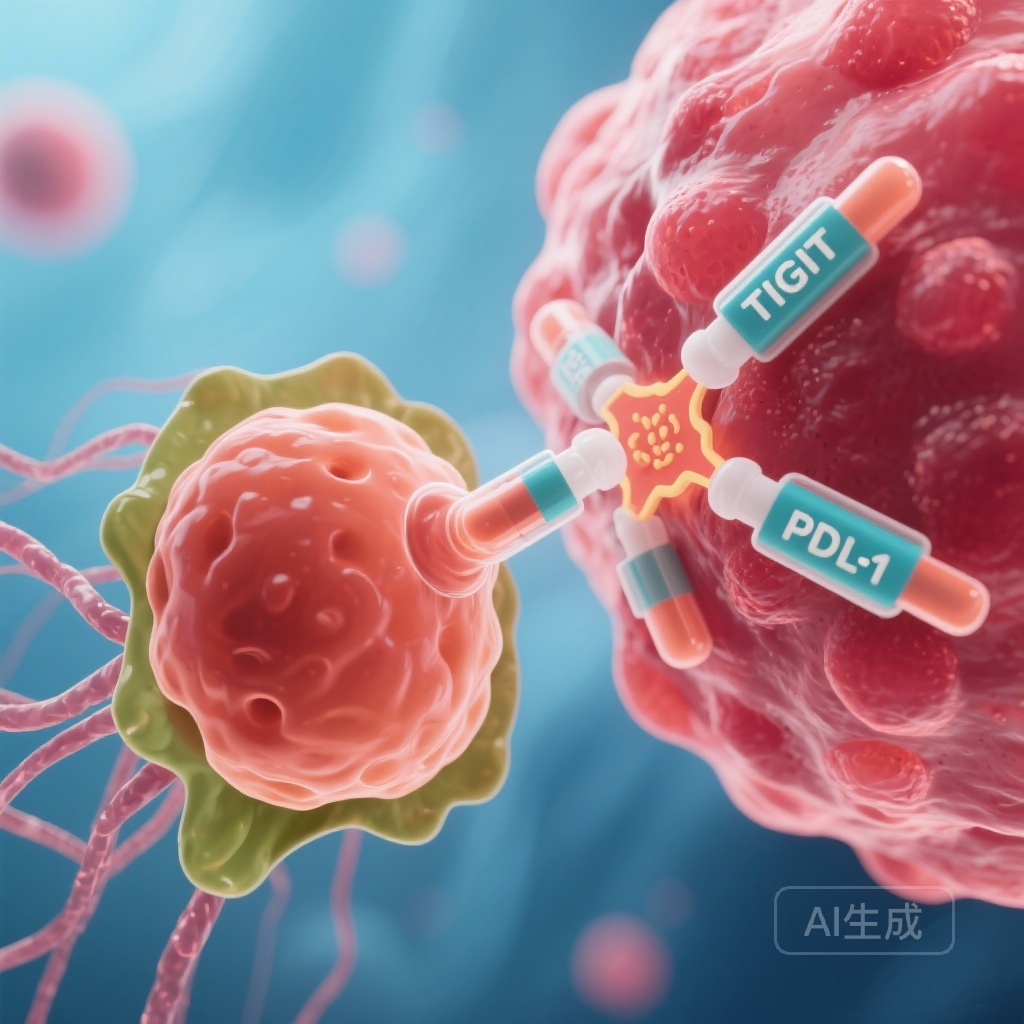
These findings from the MORPHEUS-EC trial provide strong clinical evidence for the dual inhibition of TIGIT and PD-L1 pathways in the first-line treatment of advanced esophageal cancer.
Introduction and Disease Burden
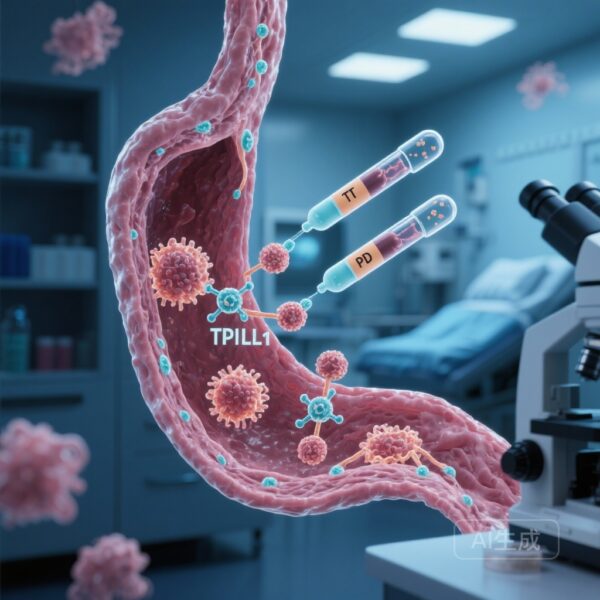
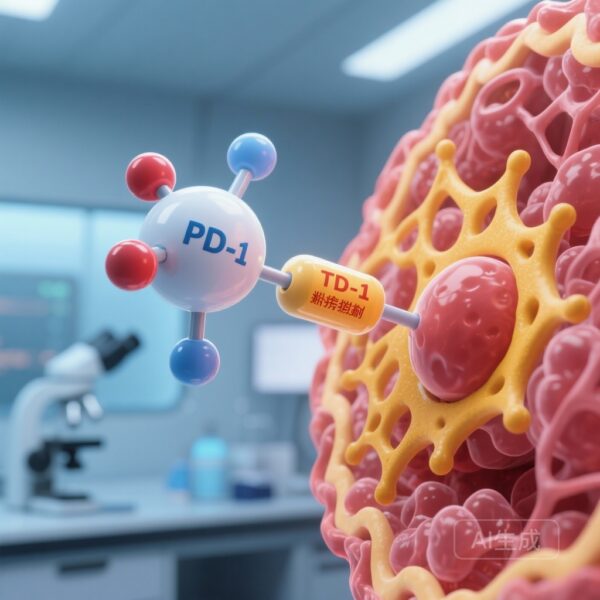
Esophageal cancer remains one of the most aggressive malignancies of the gastrointestinal tract, characterized by high mortality rates and limited therapeutic options in the advanced stages. For decades, platinum-based chemotherapy served as the cornerstone of first-line treatment for locally advanced unresectable or metastatic disease. While the recent integration of immune checkpoint inhibitors targeting the programmed death-1 (PD-1) or programmed death-ligand 1 (PD-L1) pathway has improved survival outcomes, many patients still do not derive long-term benefit or eventually experience disease progression. There is a critical unmet need for novel therapeutic combinations that can overcome primary and secondary resistance to current immunotherapy regimens.
The T-cell immunoreceptor with immunoglobulin and ITIM domains (TIGIT) has emerged as a promising co-inhibitory receptor. TIGIT is expressed on activated T cells and natural killer (NK) cells and acts as a brake on the immune system, similar to PD-1/PD-L1. Preclinical evidence suggests that the simultaneous blockade of TIGIT and PD-L1 can synergistically enhance T-cell activation and restore antitumor immunity. The MORPHEUS-EC trial was designed to evaluate this synergy in the clinical setting for treatment-naive patients with advanced esophageal cancer.
The MORPHEUS-EC Study Design
MORPHEUS-EC (NCT03281369) is a phase 1b/2, randomized, open-label, umbrella study conducted across 20 international sites, including Taiwan, South Korea, Australia, Israel, the UK, and the USA. This multi-arm design allowed for the rapid evaluation of various combination therapies against standard-of-care controls.
The study enrolled 152 patients aged 18 years or older with treatment-naive, locally advanced unresectable or metastatic esophageal cancer. Key inclusion criteria included an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Patients were randomized to one of three groups:
Experimental Arm: Tiragolumab + Atezolizumab + Chemotherapy
Patients received tiragolumab (600 mg intravenously) plus atezolizumab (1200 mg intravenously) combined with a chemotherapy backbone of cisplatin (80 mg/m2) and fluorouracil (800 mg/m2 per 24 hours on days 1-5) every 21 days.
Comparator Arm: Atezolizumab + Chemotherapy
Patients received atezolizumab (1200 mg intravenously) and the same chemotherapy backbone every 21 days.
Control Arm: Chemotherapy Alone
Patients received cisplatin and fluorouracil alone on a 21-day cycle.
The primary endpoint of the study was the investigator-assessed confirmed objective response rate (ORR) according to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Secondary endpoints included safety, progression-free survival (PFS), and overall survival (OS).
Efficacy Results: Improving the Objective Response Rate
Between June 2020 and November 2022, the trial successfully randomized 152 patients. The demographic distribution was notable, with 64% of participants being Asian and 33% White, reflecting the global burden of the disease. Most participants (89%) were male, consistent with the known epidemiology of esophageal cancer.
At the time of data cutoff, the results for the primary endpoint were highly encouraging for the TIGIT-containing triplet. The confirmed ORR was 67.7% (95% CI 54.7-79.1) in the tiragolumab plus atezolizumab and chemotherapy group. In contrast, the ORR was 53.8% (95% CI 41.0-66.3) in the atezolizumab plus chemotherapy group and 47.8% (95% CI 26.8-69.4) in the chemotherapy-only group. This numerical increase in ORR suggests a substantial additive effect of tiragolumab in inducing tumor shrinkage.
The median survival follow-up was approximately 10.9 months for the tiragolumab triplet arm and 11.4 months for the atezolizumab doublet arm. While the study was not primarily powered for long-term survival comparisons, the early signals of clinical activity supported the transition to larger, phase 3 confirmatory studies. The depth of response and the durability of these responses are currently under further investigation as the trial continues.
Safety and Tolerability Profile
The safety of combining multiple immunotherapies with cytotoxic chemotherapy is a paramount concern for clinicians. In MORPHEUS-EC, the incidence of adverse events (AEs) was relatively consistent across the three treatment arms, indicating that the addition of tiragolumab did not lead to a prohibitive increase in toxicity.
Grade 3-4 adverse events were reported in 79% of patients in the tiragolumab triplet group, 80% in the atezolizumab doublet group, and 74% in the chemotherapy group. Serious adverse events (SAEs) occurred in 58%, 51%, and 48% of patients, respectively. The most frequent treatment-related adverse events across all groups were gastrointestinal in nature, specifically nausea (ranging from 72% to 78%) and decreased appetite (ranging from 43% to 47%). Importantly, no treatment-related deaths were reported in any of the cohorts, suggesting that the triple-drug regimen is manageable in a closely monitored clinical setting.
Immune-related adverse events (irAEs), which are specific to checkpoint inhibitors, were observed but were generally consistent with the known safety profiles of atezolizumab and tiragolumab. Clinicians managing these patients should remain vigilant for signs of pneumonitis, colitis, or endocrine dysfunctions, which are typical for this class of therapy.
Clinical Implications and Mechanistic Insights
The results of MORPHEUS-EC contribute significantly to the evolving paradigm of “dual checkpoint inhibition” in oncology. The rationale for targeting TIGIT alongside PD-L1 is based on the complex immune landscape of the tumor microenvironment. Esophageal tumors often express high levels of PVR (poliovirus receptor, also known as CD155), which is the primary ligand for TIGIT. When TIGIT binds to PVR, it suppresses the activity of T cells and NK cells. By blocking both TIGIT and PD-L1, the therapy effectively removes two major inhibitory signals, potentially leading to a more robust and sustained immune attack against the cancer cells.
The trial also highlights the importance of the chemotherapy backbone. Chemotherapy can induce “immunogenic cell death,” releasing tumor antigens that further prime the immune system, making the PD-L1 and TIGIT blockade even more effective. This synergistic interaction likely explains the high ORR observed in the experimental arm.
From a clinical perspective, an ORR of nearly 68% in the first-line setting is highly significant. For patients with locally advanced disease, such a high response rate may increase the possibility of conversion to surgical resectability or provide significant palliative relief from symptoms like dysphagia in the metastatic setting.
Conclusion and Future Directions
The MORPHEUS-EC trial successfully met its objective of demonstrating the enhanced activity of tiragolumab when combined with atezolizumab and chemotherapy. The observed improvement in objective response rates, coupled with a manageable safety profile, positions the tiragolumab-based triplet as a potent candidate for the future standard of care in advanced esophageal cancer.
The medical community now looks toward the results of the phase 3 SKYSCRAPER-08 trial (NCT04540211), which has been designed to validate these findings in a larger patient population with more rigorous survival endpoints. If the phase 3 data confirm the benefits seen in MORPHEUS-EC, it will likely lead to the regulatory approval of tiragolumab and change the treatment algorithms for clinicians worldwide.
Funding and ClinicalTrials.gov
This study was funded by F. Hoffmann-La Roche-Genentech. The trial is registered with ClinicalTrials.gov under the identifier NCT03281369.
References
Sun JM, Chao Y, Kim SB, et al. First-line tiragolumab plus atezolizumab and chemotherapy in patients with previously untreated, locally advanced unresectable or metastatic oesophageal cancer (MORPHEUS-EC): a randomised, open-label, phase 1b/2 trial. Lancet Oncol. 2026 Jan;27(1):90-102. doi: 10.1016/S1470-2045(25)00402-4. PMID: 41449151.