Introduction: The Unmet Need in Acral Melanoma
For years, the management of advanced melanoma has been revolutionized by the advent of immune checkpoint inhibitors, specifically those targeting the programmed cell death 1 (PD-1) pathway. However, much of the foundational evidence for these therapies was derived from populations with cutaneous melanoma, which is characterized by high ultraviolet (UV) radiation-induced mutational burdens. In contrast, acral melanoma—a subtype occurring on non-sun-exposed surfaces such as the palms, soles, and nail beds—represents a distinct biological and clinical entity.
Acral melanoma is the most common subtype in Asian, African, and Latin American populations, yet it often exhibits a lower tumor mutational burden (TMB) and a more immunosuppressive microenvironment compared to cutaneous melanoma. Consequently, the efficacy of standard PD-1 inhibitors in the acral subtype has historically been less robust, leaving clinicians with a significant therapeutic gap. The MELATORCH trial was designed to address this deficit, evaluating the efficacy and safety of toripalimab, a high-affinity humanized IgG4 monoclonal antibody against PD-1, against the traditional chemotherapy standard, dacarbazine.
Study Design and Methodology
The MELATORCH study was a multicenter, open-label, randomized Phase 3 clinical trial conducted across several high-volume oncology centers. The trial enrolled 256 treatment-naive patients with histologically confirmed stage III or IV melanoma. A significant majority of the cohort (62.7%) presented with the acral subtype, making this one of the most comprehensive trials focused on this specific population.
Participants were randomized in a 1:1 ratio to receive either toripalimab (240 mg intravenously every 2 weeks) or dacarbazine (1000 mg/m2 intravenously every 3 weeks). The primary endpoint was progression-free survival (PFS) as determined by a blinded independent central review (BICR) using RECIST v1.1. Secondary endpoints included the objective response rate (ORR), duration of response (DOR), overall survival (OS), and safety. Notably, the trial design allowed for crossover, permitting patients in the dacarbazine arm to receive toripalimab upon documented radiographic progression, which reflects ethical standards in contemporary oncology trials.
Key Findings: Efficacy and Survival Outcomes
The results of the MELATORCH trial represent a significant milestone in the treatment of acral melanoma. At the data cutoff, the analysis revealed that toripalimab significantly outperformed dacarbazine in its primary objective.
Progression-Free Survival
Toripalimab reduced the risk of disease progression or death by 29.2% compared to dacarbazine. The hazard ratio (HR) was 0.71 (95% CI, 0.53-0.95), with a statistically significant P-value of 0.02. The median PFS as assessed by BICR provided clear evidence of clinical benefit, establishing toripalimab as a superior first-line option over conventional chemotherapy. Consistent PFS benefits were observed across various predefined subgroups, reinforcing the generalizability of these findings to the broader acral melanoma population.
Response Rates and Durability
The objective response rate (ORR) also favored the immunotherapy arm. Toripalimab achieved an ORR of 11.0% (95% CI, 6.2%-17.8%), compared to 8.6% (95% CI, 4.4%-14.9%) for dacarbazine. While these percentages may appear lower than those seen in cutaneous melanoma trials, they must be interpreted within the context of the acral subtype’s inherent resistance to therapy. Furthermore, the duration of response (DOR) was markedly longer in the toripalimab group, at 13.8 months versus 6.9 months for dacarbazine. This suggests that when patients do respond to toripalimab, the benefits are substantially more durable than those provided by cytotoxic chemotherapy.
Safety Profile and Tolerability
Safety is a paramount consideration in the first-line setting, particularly for therapies intended for long-term use. In the MELATORCH trial, toripalimab demonstrated an acceptable and manageable safety profile, consistent with the known class effects of PD-1 inhibitors.
Grade 3 or higher treatment-related adverse events (TRAEs) occurred in 28.3% of patients in the toripalimab group. The most frequent high-grade adverse events included increased lipase (8.7%), anemia (3.9%), and elevations in γ-glutamyltransferase, hyponatremia, and blood triglycerides (each at 3.1%). These immune-related adverse events (irAEs) were generally reversible with standard management protocols, including dose interruptions or corticosteroid intervention. The incidence of treatment discontinuation due to toxicity was low, suggesting that toripalimab is well-tolerated for the majority of patients over the prescribed 2-year treatment period.
Expert Commentary and Clinical Implications
Clinical experts highlight that the MELATORCH trial is a practice-changing study for the Asian oncology landscape and for global regions with a high prevalence of acral melanoma. For decades, dacarbazine remained a default comparator despite its limited efficacy, largely due to the lack of subtype-specific Phase 3 data for modern immunotherapies.
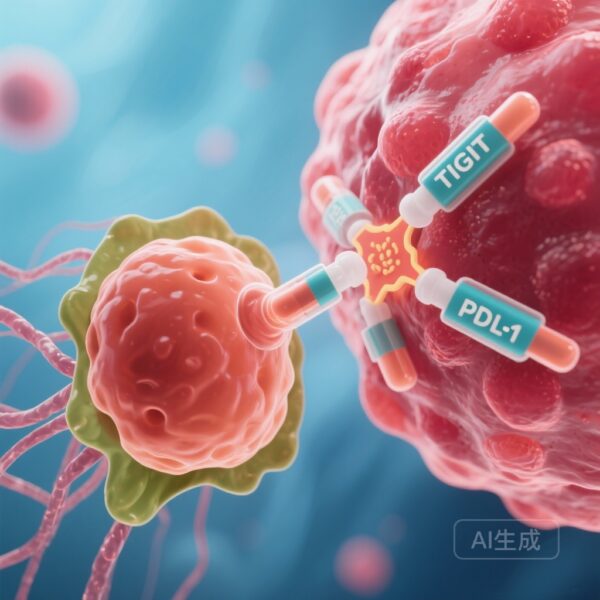
Mechanistic Insights
Toripalimab’s efficacy in this trial may be attributed to its unique binding characteristics. As a potent anti-PD-1 antibody, it exhibits high affinity and slow dissociation rates, which may provide more sustained blockade of the PD-1/PD-L1 axis even in tumors with lower TMB. The fact that toripalimab demonstrated superiority in a population where other PD-1 inhibitors have occasionally struggled suggests that its pharmacological profile is well-suited for the acral microenvironment.
Addressing Limitations
While the PFS benefit is clear, the trial’s open-label design and the crossover allowance may complicate the long-term assessment of overall survival (OS). However, in modern oncology, PFS is increasingly recognized as a clinically meaningful endpoint, especially when coupled with improvements in the duration of response and a favorable safety profile.
Conclusion
The Phase 3 MELATORCH randomized clinical trial successfully demonstrates that toripalimab is a superior first-line treatment for advanced acral melanoma compared to dacarbazine. By providing a statistically significant and clinically meaningful improvement in progression-free survival, toripalimab offers a new standard of care for a patient population that has long faced limited therapeutic options. These findings underscore the importance of subtype-specific research in melanoma and pave the way for further investigation into combination strategies involving toripalimab to further enhance response rates in this challenging disease.
Funding and Trial Registration
This study was supported by Shanghai Junshi Biosciences Co., Ltd. The trial is registered at ClinicalTrials.gov with the identifier NCT03430297.
References
1. Sheng X, Huang G, Fang M, et al. Toripalimab vs Dacarbazine as First-Line Therapy for Advanced Melanoma of Acral Subtype: The Phase 3 MELATORCH Randomized Clinical Trial. JAMA Oncol. 2026;e255751. doi:10.1001/jamaoncol.2025.5751.
2. Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. CheckMate 067: 10-Year Outcomes With Combined Nivolumab Plus Ipilimumab in Advanced Melanoma. J Clin Oncol. 2024.
3. Nakamura Y, Namikawa K, Yoshino S, et al. Anti-PD-1 antibody monotherapy for patients with acral and mucosal melanoma. Jpn J Clin Oncol. 2020;50(3):262-268.