Introduction: The Complex Interplay of Risk in Coronary Artery Disease
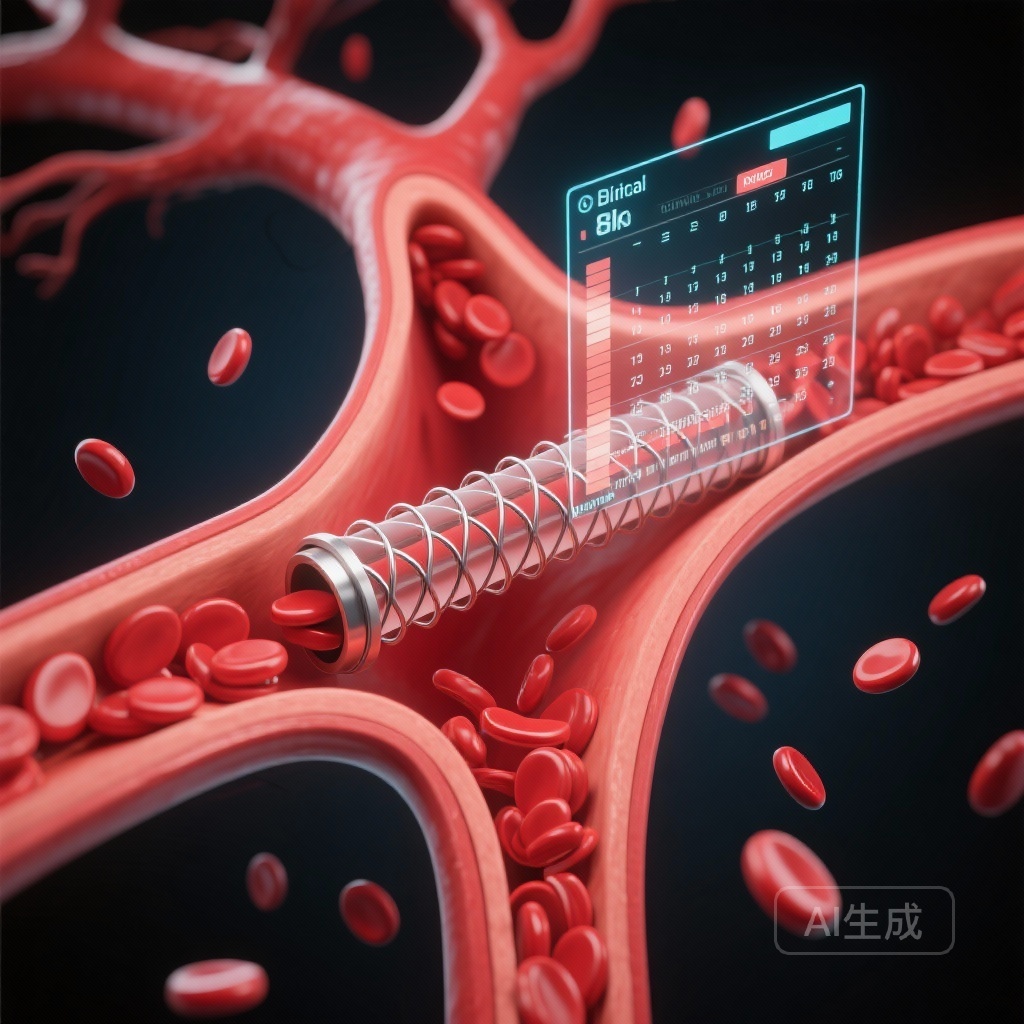
Despite significant advancements in drug-eluting stent (DES) technology and potent antiplatelet therapies, patients undergoing percutaneous coronary intervention (PCI) remain at risk for recurrent ischemic events. Conventionally, clinical management has focused on two primary pillars of risk: the biological response to antiplatelet therapy, often measured as platelet reactivity (PR), and the patient’s overall clinical profile. While both are known to influence outcomes, the temporal nature of their impact—how their predictive value changes from the acute phase to the long-term maintenance phase—has remained insufficiently characterized. A deeper understanding of this temporal divergence is essential for optimizing personalized secondary prevention strategies.
The PTRG-DES Registry: Study Design and Population
To address these gaps, the Platelet function and Genotype-Related Long-Term Prognosis in Drug-Eluting Stent-Treated Patients With Coronary Artery Disease (PTRG-DES) registry was utilized. This large-scale, multicenter registry provided a robust cohort of 11,714 patients who underwent PCI and had documented mean platelet reactivity unit (PRU) values. The study aimed to assess the interaction between biological platelet reactivity and clinical risk assessment using the Thrombolysis in Myocardial Infarction Risk Score for Secondary Prevention (TRS2P).
Methodology and Risk Stratification
The investigators stratified patients based on two distinct metrics:
-
Clinical Risk:
Stratified using the TRS2P score, which incorporates variables such as age, diabetes, hypertension, smoking status, prior stroke, peripheral artery disease, heart failure, prior myocardial infarction, and renal dysfunction. Patients were categorized as low clinical risk (score 0-1) or high clinical risk (score ≥2).
-
Platelet Reactivity (PR):
Stratified using PRU values obtained via the VerifyNow assay. High platelet reactivity (HPR) was defined as a PRU ≥252, while non-HPR was defined as a PRU <252.
The primary outcome of the study was a composite of cardiac death, myocardial infarction (MI), and stent thrombosis. To understand the temporal influence of these factors, the researchers performed landmark analyses at two critical time points: 1 month and 12 months post-PCI.
Key Findings: A Synergistic Burden of Risk
The study population exhibited a mean PRU of 217.8 ± 78.7 and a mean TRS2P score of 1.56 ± 1.12. Over the long-term follow-up period, the primary composite outcome occurred in 335 patients (5.3%). The results demonstrated a clear additive effect between biological and clinical risk factors.
The Gradient of Adverse Outcomes
The incidence of the primary outcome followed a predictable but stark gradient across the risk groups:
- High Clinical Risk + HPR: 9.4%
- High Clinical Risk + Non-HPR: 5.9%
- Low Clinical Risk + HPR: 4.8%
- Low Clinical Risk + Non-HPR: 3.9%
Notably, patients in the highest risk tier (both high clinical risk and HPR) faced a 3.25-fold higher risk of experiencing a major adverse event compared to the lowest risk group (hazard ratio [HR], 3.25; 95% CI, 2.38–4.42; P<0.001). This confirms that while clinical risk factors provide a baseline for prognosis, the presence of HPR significantly compounds that risk.
The Temporal Shift: Platelets vs. Comorbidities
Perhaps the most clinically significant finding of the PTRG-DES analysis is the temporal divergence of risk predictors. The landmark analysis revealed a “hand-off” in predictive dominance over time.
The Acute Phase (Within 1 Month)
In the first 30 days following PCI, the risk of cardiac death, MI, and stent thrombosis was predominantly driven by platelet reactivity. During this window, the healing of the vessel wall is incomplete, and the thrombogenicity of the newly implanted stent is at its peak. Patients with HPR are particularly vulnerable to acute thrombotic complications, making biological response to P2Y12 inhibitors the primary determinant of safety in the early post-procedural period.
The Maintenance Phase (Beyond 1 Month)
Conversely, beyond the initial 1-month mark, the predictive power of HPR diminished, and the TRS2P score emerged as the dominant predictor of outcomes. This suggests that once the acute procedural risk has stabilized, the patient’s underlying systemic atherosclerotic burden and comorbid conditions—such as diabetes, renal dysfunction, and prior vascular events—dictate the long-term prognosis. In this chronic phase, the risk is less about the stent itself and more about the progression of systemic coronary artery disease and non-stent-related events.
Expert Commentary and Clinical Implications
The PTRG-DES registry findings provide a roadmap for more nuanced, personalized medicine in cardiology. For the clinician, these data suggest that a “one-size-fits-all” approach to antiplatelet therapy may be suboptimal. In the early phase, ensuring adequate platelet inhibition is paramount, especially in patients identified as having HPR. This may justify the use of more potent P2Y12 inhibitors or guided therapy in the acute setting.
However, as patients move into the chronic phase of recovery, the focus must shift toward aggressive management of clinical risk factors. While continued antiplatelet therapy remains necessary, the absolute benefit of maintaining high-intensity platelet inhibition may be overshadowed by the need to manage blood pressure, lipids, and glycemic control—the components that drive the TRS2P score. The study also highlights the potential for “de-escalation” strategies: patients who are at low clinical risk and have stable platelet reactivity after the first month may be ideal candidates for less intensive antiplatelet regimens to reduce bleeding risk without significantly compromising ischemic safety.
Study Limitations
While the study is powered by a large registry, it is important to note its observational nature. The timing of PRU testing and the specific antiplatelet regimens used were at the discretion of the treating physicians, which may introduce selection bias. Additionally, while the TRS2P is a validated tool, it may not capture every nuance of a patient’s clinical risk, such as socioeconomic factors or adherence to secondary prevention medications.
Conclusion
The analysis of the PTRG-DES registry underscores that platelet reactivity and clinical risk factors are not redundant, but rather additive predictors of outcome after PCI. Platelet reactivity serves as a critical sentinel for early thrombotic risk, whereas the clinical risk score (TRS2P) provides a more accurate forecast of long-term stability and systemic events. By integrating both biological and clinical assessments, physicians can better tailor the intensity and duration of therapy to the specific temporal needs of the patient, potentially improving both short-term safety and long-term survival.
Funding and Registration
The PTRG-DES registry is registered at ClinicalTrials.gov (Unique identifier: NCT04734028). The study was supported by various institutional research grants and clinical research funds associated with the participating PTRG Investigators.
References
Kang J, Park S, Park KW, et al. Long-Term Impact of Platelet Reactivity and Clinical Risk on Clinical Outcomes in Patients With Coronary Artery Disease: Analysis of the PTRG-DES Registry. Circ Cardiovasc Interv. 2025 Oct;18(10):e015737. doi: 10.1161/CIRCINTERVENTIONS.125.015737. Epub 2025 Sep 22. PMID: 40977391.