Highlights
- Prognostic relevance of ASPECTS regions shifts based on the time from last known well to treatment.
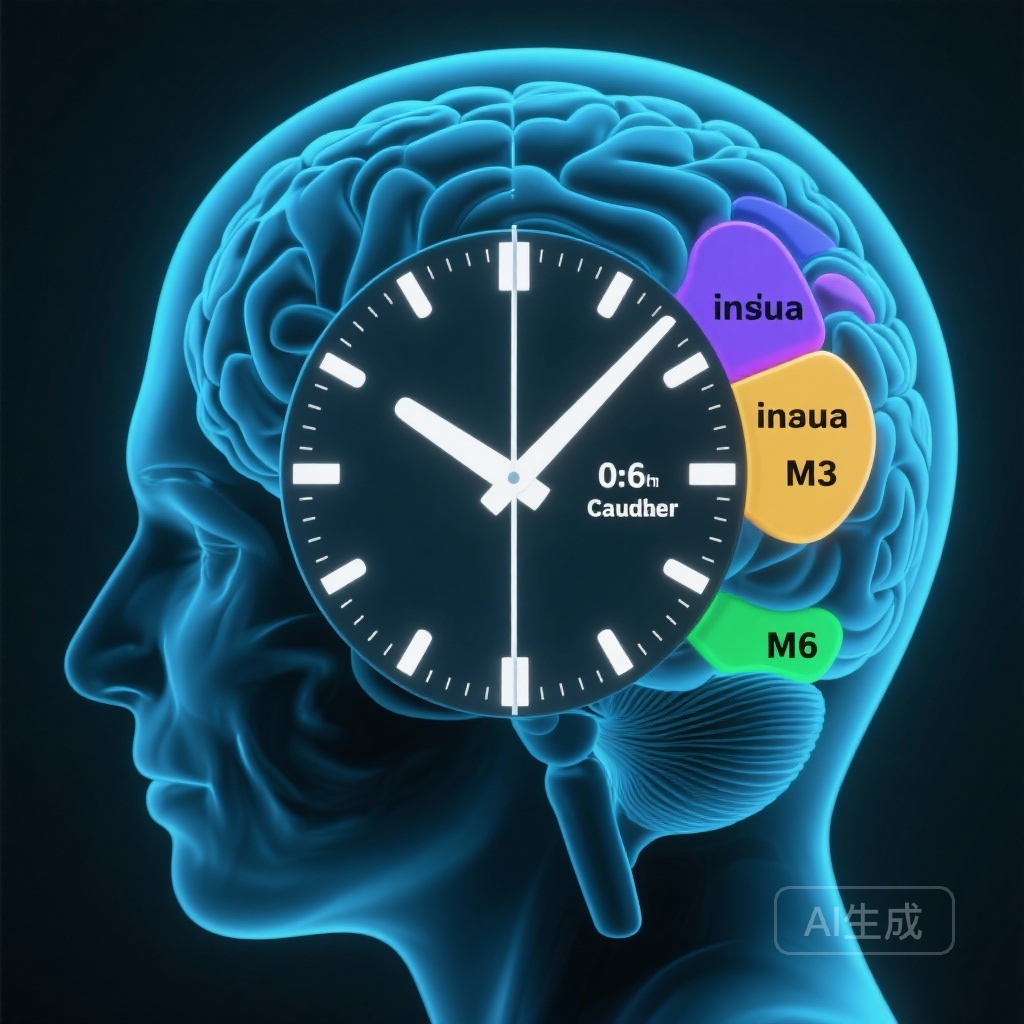
- In the early window (0-6 hours), involvement of the insula, caudate nucleus, and M6 territory independently predicts poor 90-day outcomes.
- In the extended window (6-24 hours), M3 and M5 regions emerge as the primary topographic predictors of clinical failure.
- Automated ASPECTS assessment provides objective topological data that may refine patient selection for endovascular therapy.
Introduction: The Evolution of Patient Selection in LVO
The management of acute ischemic stroke (AIS) due to large vessel occlusion (LVO) has shifted from a strict time-based paradigm to a tissue-based approach. While the Alberta Stroke Program Early CT Score (ASPECTS) is a ubiquitous tool in clinical practice for quantifying early ischemic changes, its total score often masks the functional importance of specific brain regions. Clinicians have long suspected that not all ASPECTS points are created equal; an infarct in the eloquent cortex or deep nuclei may carry different prognostic weight than one in the peripheral white matter. Furthermore, the relevance of these regions may fluctuate as the ischemic penumbra evolves over time. Understanding the topological impact on outcomes across different time windows—early (0–6 hours) and extended (6–24 hours)—is crucial for refining perioperative decision-making and optimizing patient outcomes in the era of thrombectomy.
Study Design and Methodology
This study represents a robust post-hoc analysis of data derived from two significant randomized clinical trials: DEVT and RESCUE BT. The researchers analyzed a cohort of 1,040 patients who underwent endovascular treatment (EVT) for LVO stroke. To ensure objectivity and reproducibility, pretreatment ASPECTS was evaluated using Fast-Processing of Ischemic Stroke (FPIS) software, an automated tool designed to minimize inter-observer variability.Patients were included if they presented with at least one ASPECTS region showing signs of infarction (ASPECTS ≤ 9). The cohort was stratified into two groups based on the time from last known well to puncture: the early window (0–6 hours, n=564) and the extended window (6–24 hours, n=476). The primary endpoint was a poor clinical prognosis at 90 days, defined as a modified Rankin Scale (mRS) score of 3 to 6. Multivariable logistic regression was employed to isolate the independent prognostic value of specific brain regions while adjusting for confounders such as age, baseline NIHSS, and comorbidities.
Key Findings: Regional Topography and the Clock
The analysis revealed distinct patterns of regional vulnerability that differed significantly between the two time windows.
The Early Window (0–6 Hours)
In patients treated within the first six hours of symptom onset, three specific regions were identified as independent predictors of poor 90-day outcomes:
1. The Insula
Involvement of the insula was associated with a 1.636 times higher odds of a poor outcome (95% CI: 1.130-2.367). The insula is a critical hub for autonomic regulation and sensory-motor integration; its early involvement often signifies a more severe proximal occlusion and rapid core expansion.
2. The Caudate Nucleus
The caudate nucleus showed an even stronger association (OR: 1.730, 95% CI: 1.012-2.957). As part of the basal ganglia, damage to the caudate is frequently linked to cognitive and motor deficits that can significantly impede long-term recovery.
3. The M6 Region
The M6 territory (superior parietal lobe) was the strongest predictor in this window (OR: 1.773, 95% CI: 1.041-3.022). Ischemia in this area often impacts complex motor planning and spatial awareness, contributing to high mRS scores.
The Extended Window (6–24 Hours)
For patients in the extended window, the topographic predictors shifted toward different cortical territories:
1. The M3 Region
The M3 territory (lower frontal-temporal) emerged as a powerful predictor of failure (OR: 2.153, 95% CI: 1.110-4.175). This region includes critical areas for language and executive function, and its late-stage infarction may indicate the exhaustion of collateral flow.
2. The M5 Region
The M5 territory (lateral temporal) was also significantly associated with poor prognosis (OR: 1.775, 95% CI: 1.190-2.649). Damage here often leads to significant disability due to its role in auditory processing and memory.
Expert Commentary: Clinical Implications and Biological Plausibility
The findings from this post-hoc analysis challenge the traditional use of the ASPECTS total score as a monolithic predictor. The shift in relevant regions between the early and extended windows likely reflects the underlying pathophysiology of ischemic progression. In the early window, deep gray matter structures like the caudate and the insula—which are highly sensitive to ischemia and have limited collateral supply—act as ‘canaries in the coal mine.’ Their involvement early on suggests a rapid loss of salvageable tissue.In contrast, in the extended window, patients who still have a favorable total ASPECTS score likely possess robust collateral circulation. In these ‘slow progressors,’ the eventual infarction of cortical regions like M3 and M5 becomes the decisive factor in clinical failure. This suggests that for late-presenting patients, clinicians should pay particular attention to these specific cortical landmarks even if the overall score remains relatively high.However, it is important to acknowledge the study’s limitations. As a post-hoc analysis, the results are hypothesis-generating. Furthermore, while the use of automated software increases reliability, it may not fully capture subtle variations in collateral status or individual neuroanatomy. Despite these caveats, the study provides a compelling argument for a more nuanced, ‘topographic’ approach to stroke imaging.
Conclusion
This study demonstrates that different infarct regions have varying predictive power for clinical outcomes depending on the time window of presentation. By identifying that the insula, caudate, and M6 are critical early, while M3 and M5 are vital in the extended window, this research provides clinicians with a more granular tool for risk stratification. These insights may help identify treatment-eligible patients who are in the greatest need of rapid reperfusion and assist in managing expectations for long-term recovery. Moving forward, integrating these topological weighted scores into automated triage systems could significantly enhance the precision of stroke care.
References
Xiong X, Yang D, Wan J, Yang Y, Fan S, Guo C, Liu X, Yang J, Li L, Li G, Zi W, Kong W, Li F. Relationship between ASPECTS-region and clinical outcome in patients with large vessel occlusion stroke: a post-hoc analysis of randomized clinical trial. Int J Surg. 2026 Jan 1;112(1):999-1006. doi: 10.1097/JS9.0000000000003327. PMID: 40990520.