Introduction
The first 30 days following primary percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI) represent a critical window of vulnerability. During this period, patients are at the highest risk for major adverse cardiovascular events (MACE), most notably stent thrombosis and recurrent myocardial infarction. Ensuring potent and consistent platelet inhibition is paramount to improving clinical outcomes. While current guidelines generally favor potent P2Y12 inhibitors like ticagrelor or prasugrel over clopidogrel, the use of a double-dose or twice-daily clopidogrel regimen has been proposed as a potentially more accessible or cost-effective alternative, particularly in regions where clopidogrel resistance is prevalent or newer agents are less accessible. The TADCLOT trial sought to address this clinical uncertainty by directly comparing ticagrelor with a twice-daily clopidogrel regimen in a high-risk STEMI population.
Highlights
1. The TADCLOT trial found that ticagrelor was not statistically superior to twice-daily clopidogrel in reducing MACE at 30 days post-primary PCI.
2. Sub-analysis revealed a significant reduction in MACE with ticagrelor during the first 7 and 14 days, suggesting a potential early pharmacodynamic advantage.
3. Safety outcomes, including clinically significant and major bleeding, were similar between the ticagrelor and twice-daily clopidogrel cohorts.
4. The study highlights the potential utility of intensified clopidogrel dosing in specific clinical settings, though ticagrelor remains the more potent option in the immediate post-procedural phase.
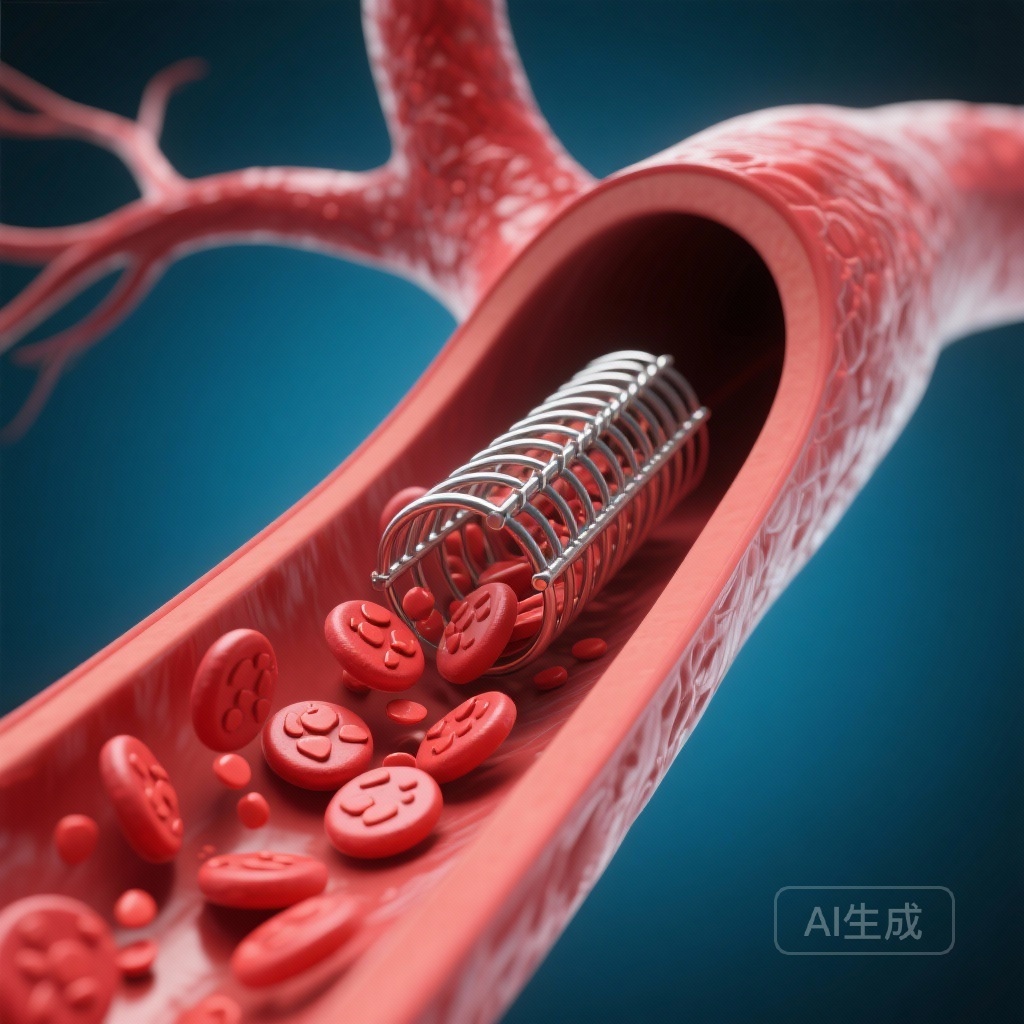
Background and Disease Burden
STEMI remains a leading cause of morbidity and mortality worldwide. Despite the success of primary PCI in restoring coronary blood flow, the procedure itself triggers a pro-thrombotic state. The activation of platelets through the P2Y12 receptor is a central mechanism in this process. Standard-dose clopidogrel (75 mg once daily) is characterized by significant inter-individual variability in antiplatelet response, often attributed to genetic polymorphisms in the CYP2C19 enzyme. This variability can lead to high on-treatment platelet reactivity (HTPR), which is strongly associated with adverse outcomes.
Ticagrelor, a direct-acting and reversible P2Y12 inhibitor, provides faster, more potent, and more consistent platelet inhibition than clopidogrel. While large-scale trials like PLATO established ticagrelor’s superiority over standard clopidogrel, the question remained whether an intensified clopidogrel regimen—specifically a twice-daily 75 mg dose—could bridge the efficacy gap. This is particularly relevant in South Asian populations, where the prevalence of loss-of-function CYP2C19 alleles is notably higher than in Western populations.
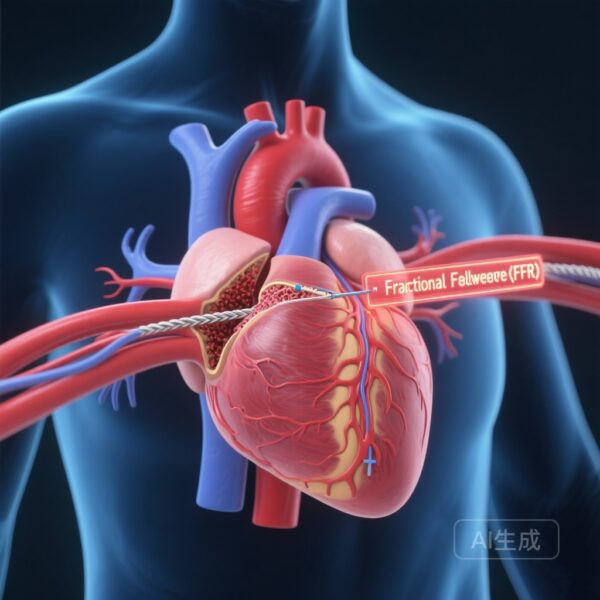
Study Design and Methodology
The TADCLOT (Twice-A-Day CLOpidogrel vs Ticagrelor) trial was a double-blind, randomized superiority trial conducted at the National Institute of Cardiovascular Diseases in Karachi, Pakistan. Between February 2024 and January 2025, the researchers enrolled 2,201 patients presenting with STEMI within 24 hours of symptom onset who underwent successful primary PCI.
Patients were randomized in a 1:1 ratio to one of two treatment arms:
1. Ticagrelor Arm: A 180-mg loading dose followed by 90 mg twice daily for one month.
2. Twice-Daily Clopidogrel Arm: A 600-mg loading dose followed by 75 mg twice daily for one month.
All patients received background aspirin therapy. The primary endpoint was MACE at one month, defined as a composite of death, myocardial infarction (MI), stent thrombosis, stroke, or target lesion revascularization (TLR). Secondary endpoints included the individual components of the primary endpoint and safety outcomes, specifically clinically significant bleeding according to the Bleeding Academic Research Consortium (BARC) types 2, 3, or 5.
Key Findings and Results
Primary Efficacy Outcomes
At the 30-day mark, the primary MACE endpoint occurred in 24 patients (2.2%) in the ticagrelor group compared to 32 patients (2.9%) in the twice-daily clopidogrel group. This difference resulted in a hazard ratio (HR) of 0.75 (95% CI: 0.44-1.27; P = 0.28). While the trend favored ticagrelor, the results did not reach statistical significance, and the absolute risk difference was only -0.7%.
Early Temporal Benefits
One of the most intriguing findings of the TADCLOT trial was the temporal distribution of events. When looking at earlier time points, ticagrelor demonstrated a clear advantage:
– At 7 days: MACE rates were significantly lower with ticagrelor (HR: 0.15; 95% CI: 0.04-0.5; P = 0.002).
– At 14 days: The benefit persisted, with ticagrelor significantly reducing events (HR: 0.46; 95% CI: 0.23-0.91; P = 0.02).
The loss of statistical significance by day 30 suggests that the most critical period for the superior potency of ticagrelor is the first two weeks following PCI.
Secondary Endpoints and Safety
Cardiovascular death or definite stent thrombosis occurred in 1.9% of the ticagrelor group vs. 2.5% of the clopidogrel group (HR: 0.77). Safety outcomes were encouraging for both arms. Clinically significant bleeding (BARC 2, 3, or 5) was rare, occurring in 0.5% of the ticagrelor group and 0.4% of the clopidogrel group (HR: 1.50; 95% CI: 0.42-5.31). Major bleeding (BARC 3 or 5) was also infrequent and similar between the two groups (0.3% vs. 0.2%).
Expert Commentary
The TADCLOT trial provides a nuanced look at antiplatelet strategies in the modern era of primary PCI. The failure to reach statistical significance for the primary endpoint at 30 days may be attributed to several factors. First, the overall event rates in both arms were lower than the investigators had initially anticipated, which likely underpowered the study to detect a small but potentially clinically relevant difference at one month.
However, the significant reduction in MACE during the first 14 days reinforces the biological plausibility that the immediate post-PCI phase requires the most aggressive platelet inhibition. Ticagrelor’s rapid onset of action and independence from hepatic metabolic activation likely explain this early lead. The fact that twice-daily clopidogrel performed comparably by day 30 suggests that once the initial hyper-thrombotic phase of the ruptured plaque and fresh stent settles, the marginal benefit of more potent inhibition may diminish.
From a global health perspective, these findings are significant. In many low- and middle-income countries, the cost of ticagrelor can be a barrier to adherence. If twice-daily clopidogrel provides a safety and efficacy profile that is “good enough” after the first two weeks, it might offer a pragmatic alternative for long-term maintenance, though this trial only looked at the first 30 days.
Limitations
The study was conducted at a single, high-volume center, which may limit the generalizability of the findings to centers with different procedural volumes or patient demographics. Furthermore, the trial was not powered to detect differences in individual components of MACE, such as stent thrombosis, which occurred at very low rates. Lastly, the study did not perform genetic testing for CYP2C19 polymorphisms, which could have provided deeper insights into why certain patients in the clopidogrel arm experienced events.
Conclusion
In patients with STEMI undergoing primary PCI, ticagrelor was not superior to twice-daily clopidogrel in reducing MACE at 30 days. However, ticagrelor did provide a significant reduction in ischemic events within the first two weeks, emphasizing its role as a preferred agent in the acute phase. Both regimens demonstrated excellent safety profiles with low rates of major bleeding. These results suggest that while ticagrelor remains a standard of care for the immediate post-PCI period, twice-daily clopidogrel may be a viable and safe intensified regimen where newer P2Y12 inhibitors are not the first choice.
Funding and Registration
This trial was registered at ClinicalTrials.gov (NCT06318481). The study was supported by institutional funding from the National Institute of Cardiovascular Diseases, Karachi, Pakistan.
References
1. Hakeem A, Shah JA, Kumar R, et al. Twice-Daily Clopidogrel vs Ticagrelor to Reduce Short-Term Major Adverse Cardiovascular Events After Primary Percutaneous Coronary Intervention: The TADCLOT Trial. J Am Coll Cardiol. 2025;86(23):2330-2345.
2. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
3. Mehta SR, Tanguay JF, Eikelboom JW, et al. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. Lancet. 2010;376(9748):1233-1243.