The Shift in Geriatric Endocrine Surgery
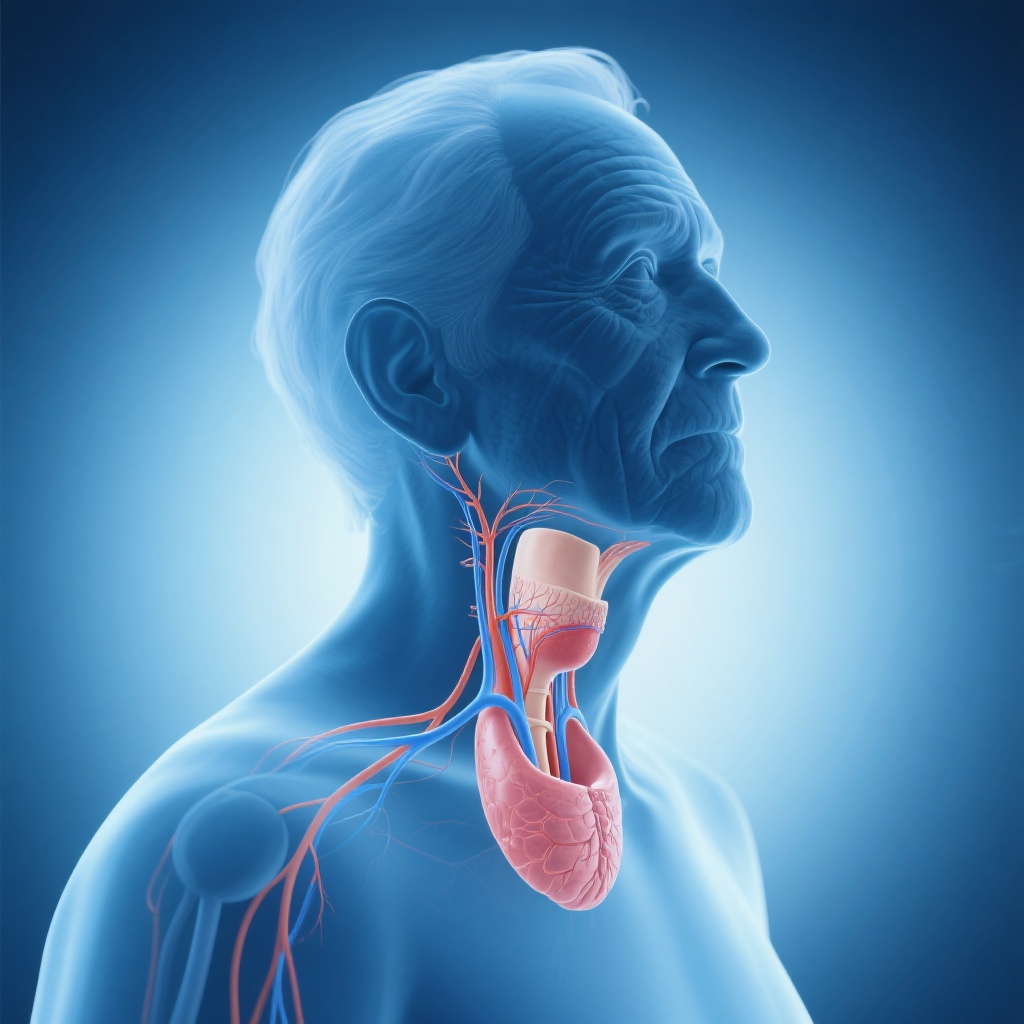
As the global population ages, the prevalence of thyroid pathology—ranging from multinodular goiter to thyroid malignancies—is rising among older adults. Historically, clinicians have often approached thyroidectomy in patients aged 65 and older with a degree of caution, fueled by concerns regarding physiological reserve, multimorbidity, and an perceived increased risk of postoperative complications. However, as surgical techniques such as intraoperative nerve monitoring and minimally invasive approaches have matured, the paradigm for geriatric surgery has shifted. The central question remains: does advanced age independently dictate a poorer safety profile for thyroidectomy, or are the risks manageable within the context of modern perioperative care?
Highlights of the Meta-Analysis
A recent comprehensive systematic review and meta-analysis by Ghani et al. (2026) published in JAMA Otolaryngology–Head & Neck Surgery provides critical clarity on this issue. The study’s primary highlights include:
- Older adults (≥65 years) exhibit significantly higher relative odds of recurrent laryngeal nerve (RLN) injury and postoperative hematoma compared to younger cohorts.
- The relative risk of mortality is statistically higher in the elderly, though the absolute incidence remains extremely low (0.3%).
- Incidence rates of hypocalcemia and wound-related complications do not differ significantly between older and younger patients.
- Despite statistical differences, the absolute increase in complications is small, suggesting that thyroidectomy remains a safe intervention for appropriately selected older patients.
Study Design and Methodological Framework
To evaluate the association between age and thyroidectomy safety, researchers conducted a systematic search across Ovid MEDLINE, CINAHL, Ovid Embase, and the Cochrane Library. The review focused on cohort studies comparing thyroidectomy outcomes between older adults (defined as ≥65 years) and younger patients. The study selection process was rigorous, following PRISMA guidelines and utilizing the ROBINS-I tool to assess the risk of bias in nonrandomized studies.
The final analysis included 11 studies encompassing a massive dataset of 427,886 patients. Within this population, 104,232 (24.4%) were classified as older adults. The meta-analysis employed random-effects models to pool data, focusing on primary outcomes such as RLN injury, hypocalcemia, hematoma, and mortality.
Key Findings: Dissecting the Complication Profile
Recurrent Laryngeal Nerve (RLN) Injury
One of the most feared complications of thyroid surgery is RLN injury, which can lead to vocal cord paralysis and significant morbidity. The meta-analysis found that older adults had a higher incidence of overall RLN injury compared to younger patients (2.3% vs. 1.0%). This resulted in an odds ratio (OR) of 1.58 (95% CI, 1.15-2.16). While the 58% increase in relative risk is statistically significant, the absolute difference of 1.3% suggests that the vast majority of older patients undergo the procedure without nerve compromise.
Postoperative Hematoma
Hematoma is a critical surgical emergency in thyroidectomy due to the risk of airway compression. The data showed that older patients were more than twice as likely to develop a hematoma (2.4% vs. 1.0%; OR, 2.32; 95% CI, 1.70-3.16). This finding is particularly relevant for clinicians managing older patients who may be on antiplatelet or anticoagulant therapies for cardiovascular comorbidities, highlighting the need for meticulous intraoperative hemostasis and vigilant postoperative monitoring.
The Mortality Paradox
The study reported a significantly higher relative risk of mortality in the older group (OR, 11.09). However, this figure must be interpreted with extreme caution. The absolute mortality rate for older adults was only 0.3%, compared to 0.01% in younger patients. While the relative difference is stark, the absolute risk remains remarkably low, reinforcing the safety of the procedure even in the geriatric population.
Hypocalcemia and Wound Complications
Interestingly, the study found no significant difference in the rates of overall hypocalcemia (OR, 0.80; 95% CI, 0.61-1.05) or wound complications (OR, 1.38; 95% CI, 0.92-2.06). This suggests that the parathyroid glands and the wound healing process in older adults are not inherently more vulnerable to the stresses of thyroid surgery than those in younger individuals.
Mechanistic Insights and Clinical Plausibility
The increased risk of RLN injury and hematoma in older adults may be attributed to several biological and clinical factors. With age, the thyroid gland may undergo changes such as increased fibrosis or the development of larger, more vascular goiters, which can obscure surgical planes and increase the technical difficulty of the dissection. Furthermore, age-related changes in vascular integrity and the higher prevalence of hypertension in the elderly likely contribute to the increased hematoma rate.
From a mortality perspective, the slightly higher rate in older adults is likely reflective of a higher burden of systemic comorbidities—such as cardiovascular and respiratory disease—rather than the surgical procedure itself. This underscores the importance of preoperative optimization and frailty assessment rather than age-based exclusion from surgery.
Expert Commentary and Clinical Implications
The findings of this meta-analysis serve as a vital tool for patient counseling and shared decision-making. Clinicians should not use age as a sole contraindication for thyroidectomy. Instead, the focus should shift toward individualized risk stratification. For an older patient with a symptomatic goiter or a suspicious thyroid nodule, the small absolute increase in risk must be weighed against the benefits of surgical intervention and the potential risks of disease progression.
Perioperative planning should be tailored for the elderly. This includes a thorough medication review (particularly for blood thinners), aggressive management of blood pressure to prevent postoperative hematoma, and perhaps a more conservative approach in patients with significant frailty. The use of intraoperative nerve monitoring (IONM) may also be particularly beneficial in this demographic to further mitigate the risks of RLN injury.
Conclusion: A Balanced Perspective
In conclusion, while older adults (≥65 years) face statistically higher odds of recurrent laryngeal nerve injury, hematoma, and mortality following thyroidectomy, the absolute incidence of these complications remains low. Thyroidectomy is an inherently safe procedure in the geriatric population. These findings support the continued use of thyroid surgery in older patients when indicated, provided that surgeons and anesthesiologists perform careful preoperative assessments and maintain high standards of perioperative care. The goal of modern endocrine surgery should be to ensure that age does not become a barrier to receiving standard-of-care surgical treatment.
References
Ghani A, Ayesh AR, Rajaram H, Ganegoda SM, Alogakos M, Sato A, Hage K, Than CA, Nakanishi H, Shin J, Romero-Velez G. Thyroidectomy Outcomes in Older Adults: A Systematic Review and Meta-Analysis. JAMA Otolaryngol Head Neck Surg. 2026 Feb 5:e255345. doi: 10.1001/jamaoto.2025.5345. Epub ahead of print. PMID: 41642589.