The Shift Toward T-Cell Redirection in Early Relapse
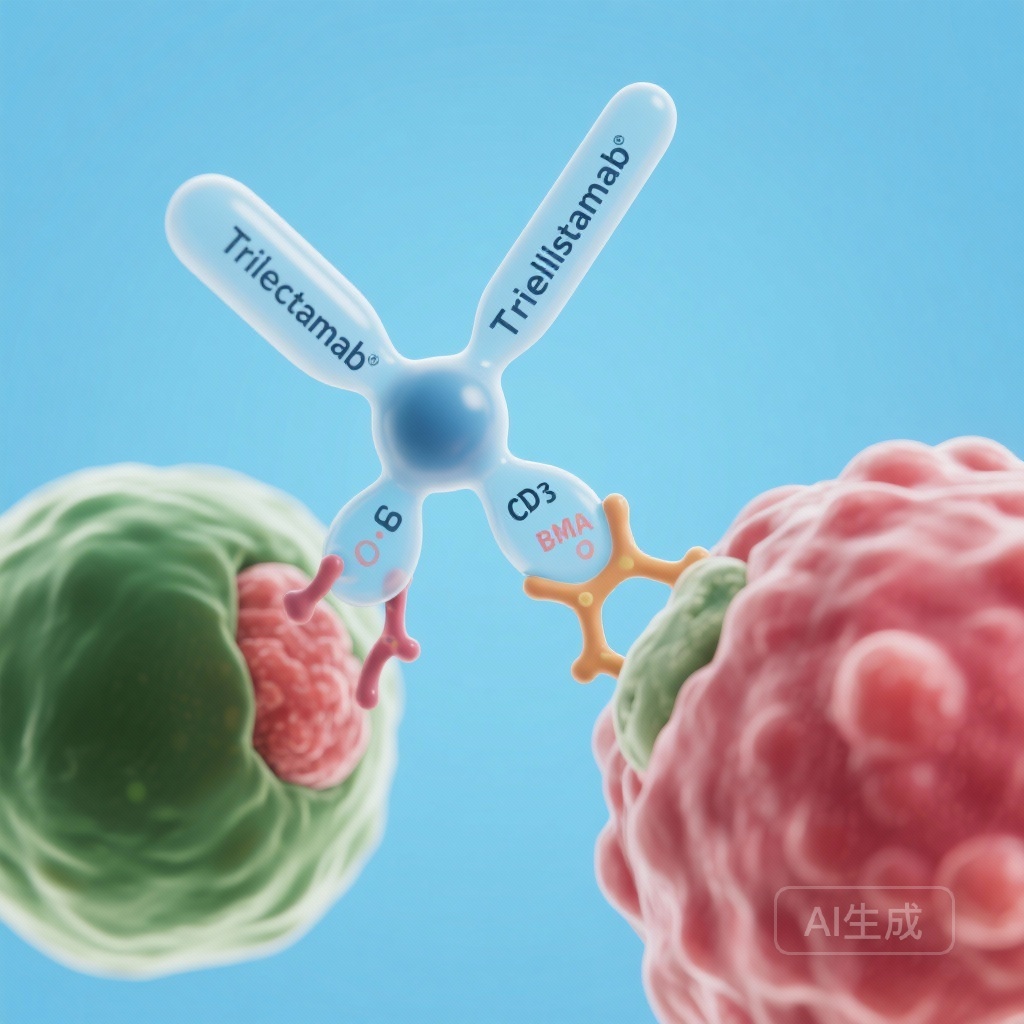
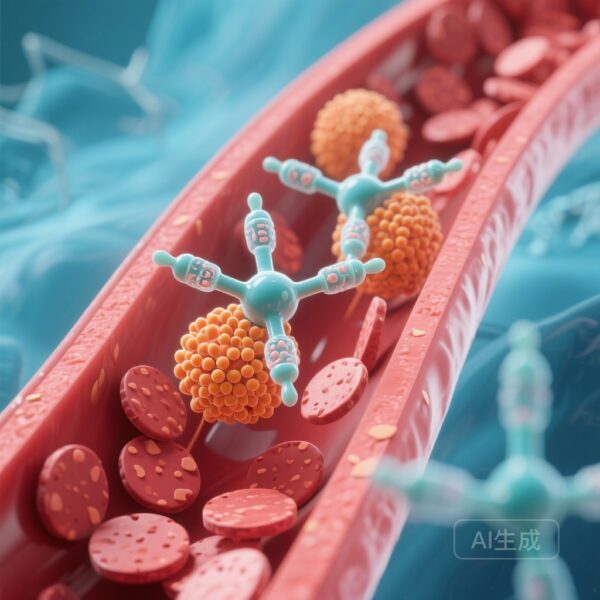
The management of multiple myeloma (MM) has been revolutionized over the last decade by the introduction of proteasome inhibitors (PIs), immunomodulatory drugs (IMiDs), and anti-CD38 monoclonal antibodies. Despite these advancements, the disease remains characterized by successive relapses, with each subsequent line of therapy typically yielding shorter durations of response. The emergence of T-cell redirecting therapies, specifically bispecific antibodies (BsAbs) targeting B-cell maturation antigen (BCMA), has opened a new frontier. Teclistamab, a first-in-class BCMA-directed T-cell engager, initially demonstrated remarkable efficacy as a monotherapy in heavily pretreated populations. However, the logical clinical progression involves moving these potent agents into earlier lines of therapy and combining them with established standards of care, such as daratumumab, to optimize synergy and overcome resistance mechanisms.
MajesTEC-3: A Deep Dive into Phase 3 Methodology
The MajesTEC-3 trial (NCT05083169) represents a pivotal phase 3 investigation designed to evaluate whether the combination of teclistamab and daratumumab could outperform standard-of-care triplet regimens in patients who have experienced early relapse.
Patient Selection and Study Population
The study enrolled 587 patients who had received between one and three previous lines of therapy. This population represents a critical clinical window where patients are often fit enough to tolerate intensive immunotherapy but are already showing signs of resistance to initial regimens. Patients were randomly assigned in a 1:1 ratio to receive either the teclistamab-daratumumab combination or an investigator’s choice of standard care, which included daratumumab plus dexamethasone combined with either pomalidomide (DPd) or bortezomib (DVd).
Study Endpoints and Assessment
The primary endpoint was progression-free survival (PFS), as determined by an independent review committee using International Myeloma Working Group (IMWG) criteria. Secondary endpoints were comprehensive, including overall response rate (ORR), the rate of complete response (CR) or better, and minimal residual disease (MRD) negativity at a sensitivity of 10^-5. This robust design aimed not only to measure the delay in disease progression but also the depth and quality of the molecular response.
Efficacy Outcomes: A New Benchmark in RRMM
The results of MajesTEC-3, reported at a median follow-up of 34.5 months, have established a new efficacy benchmark for relapsed multiple myeloma.
Unprecedented Progression-Free Survival
The most striking finding was the significant prolongation of PFS in the teclistamab-daratumumab group. The hazard ratio (HR) for progression or death was 0.17 (95% CI, 0.12 to 0.23; P<0.001), representing an 83% reduction in risk compared to the DPd or DVd control group. The estimated 36-month PFS rate was 83.4% for the combination arm versus 29.7% for the control arm. In the context of multiple myeloma clinical trials, a hazard ratio of 0.17 is exceptionally rare and suggests a profound therapeutic advantage for the bispecific-monoclonal antibody combination.
Depth of Response and MRD Negativity
Beyond PFS, the quality of responses was significantly superior in the teclistamab-daratumumab group. The overall response rate (ORR) reached 89.0%, compared to 75.3% in the control group. More importantly, the rate of achieving a complete response or better was more than double that of the control group (81.8% vs. 32.1%).
Furthermore, the achievement of MRD negativity (10^-5) was observed in 58.4% of patients in the experimental arm, compared to just 17.1% in the standard-of-care arm. This high rate of MRD negativity is clinically significant as it is increasingly recognized as a surrogate marker for long-term survival in myeloma. The ability to achieve such deep responses in the relapsed setting suggests that the combination of BCMA targeting and CD38 targeting effectively clears the bone marrow of malignant clones more efficiently than traditional combinations.
Comparing Monotherapy vs. Combination: MajesTEC-1 vs. MajesTEC-3
To fully appreciate the MajesTEC-3 results, one must look at the foundation laid by MajesTEC-1. In the MajesTEC-1 phase 1-2 study, teclistamab was administered as a monotherapy to a much more heavily pretreated population (median of 5 prior lines; 77.6% triple-class refractory). In that setting, teclistamab achieved an ORR of 63.0% and a median PFS of 11.3 months.
When we compare these to MajesTEC-3, two things become clear. First, using teclistamab earlier (1-3 prior lines) and in combination with daratumumab leads to significantly higher response rates (89% ORR) and a dramatically longer PFS. Second, the synergy between daratumumab and teclistamab likely enhances T-cell function or sensitizes myeloma cells to T-cell-mediated lysis. Daratumumab is known to deplete CD38-positive immunosuppressive regulatory T cells and myeloid-derived suppressor cells, potentially creating a more favorable microenvironment for teclistamab-activated T cells to exert their anti-tumor effects.
Safety and Tolerability Profile
The enhanced efficacy of the teclistamab-daratumumab combination comes with a specific safety profile that requires proactive management.
Cytokine Release Syndrome and Neurotoxicity
In line with its mechanism of action as a T-cell redirector, teclistamab is associated with cytokine release syndrome (CRS). In the MajesTEC-1 monotherapy study, CRS occurred in 72.1% of patients, though the vast majority were low-grade (Grade 3 in only 0.6%). In MajesTEC-3, the overall safety profile was consistent with the known toxicities of both agents. Clinicians must remain vigilant during the step-up dosing phase, as this is when the risk for CRS and immune effector cell-associated neurotoxicity syndrome (ICANS) is highest.
Infections and Hematologic Toxicity
Serious adverse events were reported in 70.7% of the teclistamab-daratumumab group compared to 62.4% in the control group. A significant concern with BCMA-targeted therapies is the risk of high-grade infections due to both treatment-induced neutropenia and the depletion of normal plasma cells (hypogammaglobulinemia). In MajesTEC-1, infections occurred in 76.4% of patients. In MajesTEC-3, the rate of death from adverse events was slightly higher in the experimental arm (7.1% vs 5.9%). This highlights the need for rigorous supportive care, including intravenous immunoglobulin (IVIG) replacement, prophylactic antimicrobials, and careful monitoring of absolute neutrophil counts.
Clinical Implications and Future Directions
The MajesTEC-3 trial provides definitive evidence that T-cell redirecting bispecific antibodies should not be reserved only for the end-stage, triple-class refractory setting. By moving teclistamab into earlier lines of therapy and combining it with daratumumab, clinicians can achieve unprecedented control over the disease.
However, several questions remain for the clinical community. These include the optimal duration of therapy, the potential for fixed-duration treatment in patients achieving sustained MRD negativity, and the management of long-term infectious risks. Furthermore, as bispecifics move earlier in the treatment algorithm, the sequencing of subsequent therapies—including CAR-T cell therapy—will require further investigation. For now, the combination of teclistamab and daratumumab stands as a potent new standard for patients with relapsed or refractory multiple myeloma after 1-3 prior lines of therapy.
Conclusion
The integration of teclistamab and daratumumab represents a major leap forward in myeloma care. With an 83% reduction in the risk of progression and nearly 60% of patients achieving MRD negativity, this combination offers a level of efficacy previously unseen in the early relapsed setting. While the management of toxicities—particularly infections and CRS—remains a challenge, the potential for long-term disease control makes this a transformative option for clinicians and patients alike.
Funding and Trial Information
The MajesTEC-3 trial was funded by Johnson & Johnson. ClinicalTrials.gov number: NCT05083169. The MajesTEC-1 trial was funded by Janssen Research and Development. ClinicalTrials.gov numbers: NCT03145181 and NCT04557098.
References
1. Costa LJ, Bahlis NJ, Perrot A, et al. Teclistamab plus Daratumumab in Relapsed or Refractory Multiple Myeloma. N Engl J Med. 2025. doi:10.1056/NEJMoa2514663.
2. Moreau P, Garfall AL, van de Donk NWCJ, et al. Teclistamab in Relapsed or Refractory Multiple Myeloma. N Engl J Med. 2022;387(6):495-505. doi:10.1056/NEJMoa2203478.