Introduction: The Quest to Mitigate Neurological Risks in TAVI
Transcatheter aortic valve implantation (TAVI) has revolutionized the management of severe symptomatic aortic stenosis, evolving from a last-resort treatment for inoperable patients to the standard of care across all surgical risk profiles. However, despite technical refinements and increased operator experience, periprocedural neurological complications remain a significant concern. The procedure involves the manipulation of catheters through calcified aortas and the expansion of prosthetic valves, which can liberate embolic material—including calcium, thrombus, and arterial wall tissue—into the cerebral circulation.
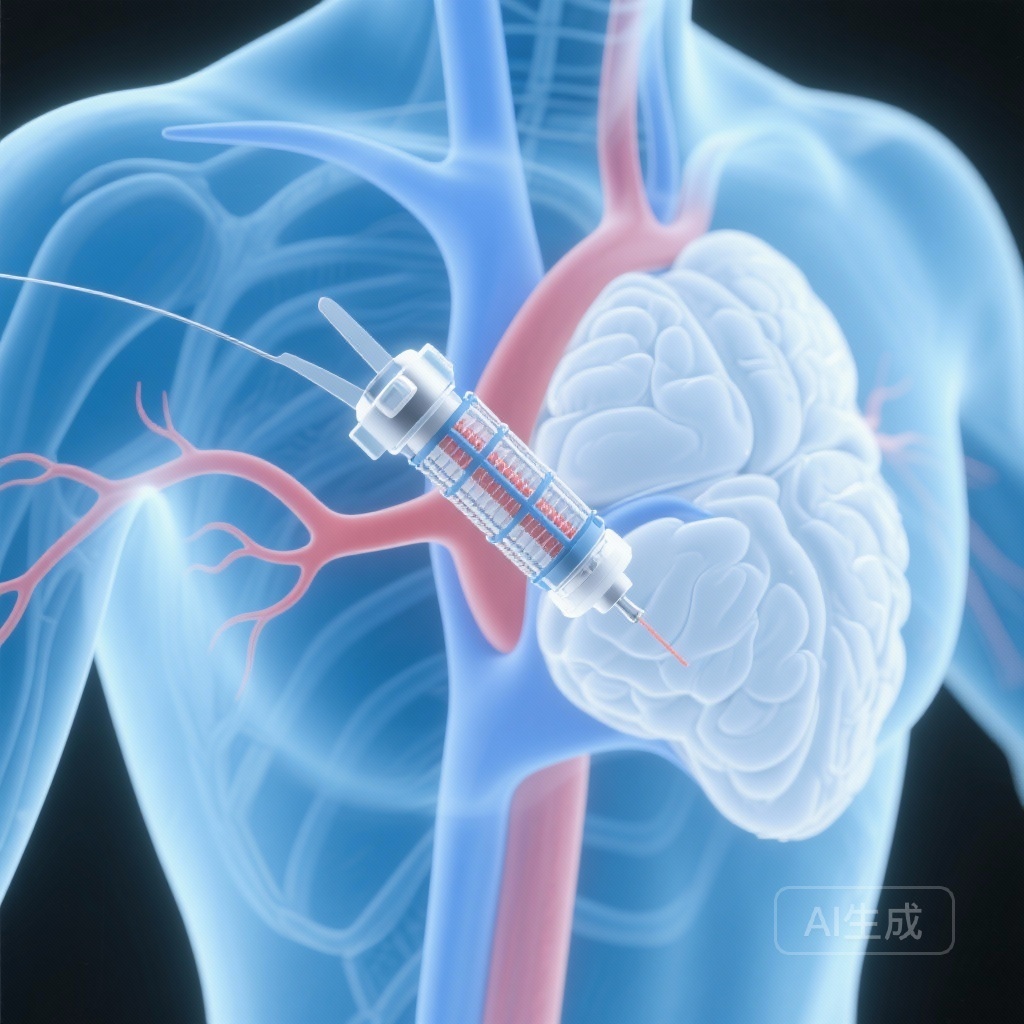
To address this, cerebral embolic protection (CEP) devices were developed to capture or deflect this debris. The SENTINEL device, a dual-filter system placed in the brachiocephalic and left common carotid arteries, is the most widely studied of these interventions. While earlier, smaller studies suggested a reduction in new lesion volume on brain MRI, the clinical benefit regarding hard endpoints like stroke and cognitive function remained debated. The BHF PROTECT-TAVI trial was designed to provide a definitive answer regarding the utility of routine CEP in a large, real-world population.
The Clinical Burden of Cerebral Embolization
Cerebral embolization during TAVI is almost universal, as evidenced by silent ischemic lesions on diffusion-weighted MRI in over 90% of patients. While many of these lesions are clinically silent, they have been hypothesized to contribute to post-operative delirium and long-term neurocognitive decline. The incidence of clinically overt stroke within 72 hours of TAVI typically ranges from 1% to 3%, and these events are associated with a significantly higher risk of mortality and long-term disability. Given the aging population undergoing TAVI, preserving cognitive function is as critical as preventing motor deficits. Therefore, the medical community looked toward the BHF PROTECT-TAVI trial to determine if the routine use of CEP should become the standard of care.
Study Design: The BHF PROTECT-TAVI Framework
Trial Methodology and Population
The BHF PROTECT-TAVI trial (British Heart Foundation Randomized Trial of Routine Cerebral Embolic Protection in Transcatheter Aortic Valve Implantation) was a multicenter, randomized, controlled trial conducted across 33 centers in the United Kingdom. The trial enrolled 7,635 participants with aortic stenosis scheduled for TAVI. Participants were randomized in a 1:1 ratio to receive either TAVI with the SENTINEL CEP device (CEP group) or standard TAVI without CEP (control group).
The trial was uniquely powered to detect differences in clinical stroke. Furthermore, a pre-specified secondary analysis was conducted on 3,535 participants to evaluate the impact of CEP on neurocognitive function, making it the largest study to date to assess cognitive outcomes in the context of TAVI and embolic protection.
Endpoints and Statistical Rigor
The primary endpoint for the main trial was the incidence of stroke within 72 hours of the TAVI procedure or before hospital discharge. For the cognitive sub-study, the primary outcome was the mean change in the telephone version of the Montreal Cognitive Assessment (t-MoCA) from baseline to a 6-to-8-week follow-up. The t-MoCA is a validated tool for assessing cognitive domains including attention, memory, and executive function, with a total score ranging from 0 to 22. A secondary cognitive endpoint was defined as a drop of 3 or more points in the t-MoCA score, representing a clinically significant decline.
Key Findings: Stroke Incidence and Safety
The results of the primary trial, published in the New England Journal of Medicine, were neutral. Among the 7,635 participants, a primary-outcome event (stroke within 72 hours) occurred in 2.1% of the CEP group compared to 2.2% of the control group (risk difference, -0.02 percentage points; 95% CI, -0.68 to 0.63; P = 0.94).
When examining the severity of strokes, disabling stroke occurred in 1.2% of the CEP group and 1.4% of the control group, a difference that was not statistically significant. Mortality rates at the time of discharge were also similar between the groups (0.8% in the CEP group vs. 0.7% in the control group). Regarding safety, access-site complications occurred in 8.1% of the CEP group and 7.7% of the control group, and serious adverse events related to the CEP device were rare (0.6%).
Secondary Analysis: Impact on Neurocognitive Function
The cognitive analysis, published in Circulation, included 1,763 patients in the CEP group and 1,772 in the control group. The median age was 81 years, and the baseline median t-MoCA score was 18, indicating a degree of baseline cognitive frailty in this elderly population.
At the 6-to-8-week follow-up, both groups showed a slight improvement in cognitive scores, with a median t-MoCA of 20. The mean adjusted change in total t-MoCA score was 0.83 in the CEP group and 0.91 in the control group. The difference between the two groups was -0.07 (95% CI, -0.22 to 0.09; P=0.42), showing no benefit of the CEP device in preserving or improving cognitive function.
Furthermore, the incidence of a significant cognitive decline (a drop of ≥3 points) was 8.7% in the CEP group and 8.0% in the control group (risk difference 0.72%; P=0.44). Subgroup analyses based on age, sex, baseline cognitive status, and surgical risk scores also failed to identify any specific population that derived a cognitive benefit from CEP use.
Expert Commentary and Clinical Implications
Interpreting the Null Results
The findings of BHF PROTECT-TAVI are consistent with the previously published PROTECTED TAVI trial (2022), which also found no significant reduction in the primary endpoint of all-stroke. While the earlier trial suggested a potential reduction in disabling strokes, BHF PROTECT-TAVI—with a larger sample size—did not confirm this trend.
Several factors may explain why a device that successfully captures embolic debris does not translate into improved clinical outcomes. First, the SENTINEL device does not provide full cerebral coverage; it protects the brachiocephalic and left common carotid arteries but leaves the left vertebral artery (and thus the posterior circulation) vulnerable. Second, periprocedural strokes in TAVI are multifactorial. Beyond macro-embolization during valve deployment, strokes can be caused by micro-emboli, periprocedural hypotension, or new-onset atrial fibrillation, none of which are mitigated by a mechanical filter.
The Role of CEP in Modern Practice
The results of BHF PROTECT-TAVI suggest that the routine, unselected use of CEP in all TAVI procedures is not supported by current evidence. From a health policy and cost-effectiveness perspective, the addition of a CEP device increases procedural costs and complexity without a measurable improvement in patient-centered outcomes like stroke prevention or cognitive preservation.
However, some clinicians argue that CEP may still have a role in “high-risk” cases, such as those with heavily calcified aortic arches or valves, or in patients undergoing valve-in-valve procedures. Yet, it must be noted that even in the subgroup analyses of BHF PROTECT-TAVI, no specific group showed a clear benefit. The slight improvement in t-MoCA scores across both groups post-TAVI likely reflects the hemodynamic benefits of relieving aortic stenosis, which may improve cerebral perfusion, or potentially a practice effect of the cognitive test itself.
Conclusion: Re-evaluating Routine Prophylaxis
The BHF PROTECT-TAVI trial provides high-quality, randomized evidence that the routine use of the SENTINEL cerebral embolic protection device during TAVI does not reduce the risk of periprocedural stroke or post-operative cognitive decline. While the device is safe and successfully captures debris, the clinical impact of this debris capture appears negligible in the context of modern TAVI practice. Future research should perhaps focus on identifying the specific mechanisms of periprocedural stroke that occur despite embolic protection and exploring alternative strategies for neuroprotection in the most vulnerable patients.
Funding and Clinical Trial Information
The BHF PROTECT-TAVI trial was funded by the British Heart Foundation and Boston Scientific.
ClinicalTrials.gov Identifier: ISRCTN16665769.
References
1. Kennedy J, Blackman DJ, et al. Impact of Cerebral Embolic Protection on Cognitive Function After Transcatheter Aortic Valve Implantation: Data From the BHF PROTECT-TAVI Randomized Trial. Circulation. 2025;152(18):1268-1278.
2. Kharbanda RK, Kennedy J, et al. Routine Cerebral Embolic Protection during Transcatheter Aortic-Valve Implantation. N Engl J Med. 2025;392(24):2403-2412.
3. Kapadia SR, Makkar R, et al. Cerebral Embolic Protection during Transcatheter Aortic-Valve Replacement. N Engl J Med. 2022;387(14):1253-1263. (PROTECTED TAVI Trial for context).