Highlights
- The STEEER-AF trial found that a 16-week structured educational program for healthcare professionals significantly improved adherence to rhythm control guidelines (RR 1.51).
- In contrast, education did not significantly improve guideline adherence for stroke prevention, likely due to high baseline rates of oral anticoagulation use.
- Patients in the intervention group were 5.1% more likely to receive integrated AF management compared to the control group.
- The study highlights that while education can bridge complex implementation gaps, it may face ceiling effects in areas where practice is already well-established.
Introduction: The Implementation Gap in Atrial Fibrillation
Atrial fibrillation (AF) remains a leading cause of stroke, heart failure, and cardiovascular morbidity worldwide. While the European Society of Cardiology (ESC) and other major bodies provide clear Class I and III recommendations for AF management, a persistent gap remains between these evidence-based guidelines and real-world clinical practice. This ‘implementation gap’ often results in suboptimal patient outcomes. The STEEER-AF trial was designed to rigorously test whether a structured, professional educational intervention could bridge this gap by improving healthcare professional (HCP) adherence to guidelines regarding stroke prevention and rhythm control.
The STEEER-AF Study Design
STEEER-AF was a large-scale, cluster-randomized clinical trial conducted across 70 centers in six countries. The study recruited 1,732 patients with AF during routine clinical practice. The randomization occurred at the center level, accounting for baseline adherence to ESC recommendations to ensure balanced cohorts.
The Intervention
Healthcare professionals in the intervention centers participated in a 16-week structured educational program. This program involved approximately 9 hours of online engagement, focusing on the nuances of AF management, including patient selection for rhythm control and stroke risk stratification. The control centers continued with standard practice, receiving no additional educational resources beyond their usual professional development.
Primary Endpoints
The trial utilized two co-primary endpoints to assess the impact of the intervention: patient-level adherence to Class I and III guidelines for stroke prevention and adherence to guidelines for rhythm control. Adherence was determined using a standardized, pre-published decision tree algorithm to ensure objective evaluation across all centers.
Key Findings: Differential Success in Care Implementation
The results of the STEEER-AF trial, published in Nature Medicine, provide a nuanced look at the efficacy of professional education in cardiology.
Stroke Prevention: A Ceiling Effect?
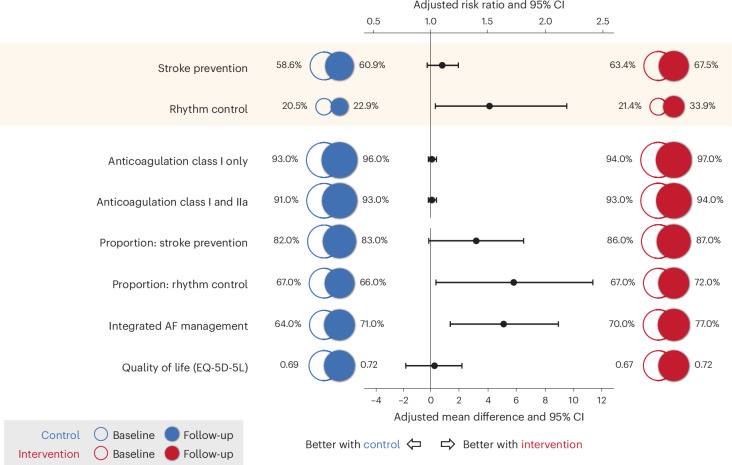
At baseline, adherence to stroke prevention guidelines was relatively high at 61.0%. At the follow-up (median 7.7 months), adherence rose to 67.5% in the intervention group and 60.9% in the control group. However, the adjusted risk ratio (RR) was 1.10 (95% CI 0.97 to 1.24; P = 0.13), indicating that the improvement was not statistically significant. A major factor contributing to this result was the already high rate of oral anticoagulation (OAC) prescription, which was 94% at baseline across both groups. This suggests a potential ‘ceiling effect’ where educational interventions struggle to move the needle in areas where practice is already largely optimized.
Table 2.
Primary and secondary outcomes
| Outcome | Intervention | Control | Risk ratio (95% CI); P value | Risk or mean difference (95% CI); P value | ||
|---|---|---|---|---|---|---|
| Baseline (N = 865) | Follow-up (N = 765) | Baseline (N = 867) | Follow-up (N = 773) | |||
| Co-primary outcomes | ||||||
| Stroke prevention guideline adherence, n (%) | 548 (63.4%) | 516 (67.5%) | 508 (58.6%) | 471 (60.9%) | 1.10 (0.97 to 1.24), P = 0.13 | 6.0% (−1.5% to 13.4%), P = 0.12 |
| Rhythm control guideline adherence, n (%) | 185 (21.4%) | 259 (33.9%) | 178 (20.5%) | 177 (22.9%) | 1.51 (1.04 to 2.18), P = 0.03 | 11.2% (1.6% to 20.7%), P = 0.02 |
| Secondary outcomes | ||||||
| Anticoagulation class I indication, n (%)a | 608 (94.4%) | 559 (97.2%) | 602 (92.8%) | 556 (95.7%) | 1.02 (0.99 to 1.05), P = 0.26 | 1.6% (−1.1% to 4.3%), P = 0.26 |
| Anticoagulation class I and IIa, n (%)b | 723 (93.1%) | 649 (94.5%) | 717 (91.2%) | 653 (93.3%) | 1.01 (0.98 to 1.05), P = 0.40 | 1.3% (−1.7% to 4.3%), P = 0.40 |
| Proportion of relevant guidelines with adherence for stroke prevention, mean (s.d.) | 0.86 (0.21) | 0.87 (0.20) | 0.82 (0.25) | 0.83 (0.25) | – | 3.2% (−0.1% to 6.5%), P = 0.06 |
| Proportion of relevant guidelines with adherence for rhythm control, mean (s.d.) | 0.67 (0.27) | 0.72 (0.28) | 0.67 (0.25) | 0.66 (0.27) | – | 5.8% (0.4% to 11.3%), P = 0.04 |
| Patient-reported integrated AF management, mean (s.d.) | 0.70 (0.28) | 0.77 (0.26) | 0.64 (0.29) | 0.71 (0.26) | – | 5.1% (1.4% to 8.9%), P = 0.01 |
| Patient-reported quality of life | ||||||
| EQ-5D-5L index score, mean (s.d.) | 0.84 (0.20) | 0.81 (0.28) | 0.83 (0.21) | 0.80 (0.27) | – | 0.00 (−0.03% to 0.03%), P = 0.95 |
| Visual analog scale, mean (s.d.) | 67.3 (19.3) | 71.6 (18.5) | 68.6 (19.1) | 71.6 (16.7) | – | 0.3 (−1.7% to 2.2%), P = 0.79 |
Fig. 2. Co-primary and secondary outcomes.
Rhythm Control: A Significant Breakthrough
In contrast, rhythm control management showed a much wider implementation gap at baseline, with overall adherence at only 21.0%. Following the intervention, adherence in the educational group increased to 33.9%, compared to 22.9% in the control group. This resulted in a statistically significant adjusted risk ratio of 1.51 (95% CI 1.04 to 2.18; P = 0.03). The adjusted risk difference was 11.2%, highlighting that education is particularly effective when addressing complex therapeutic areas with lower baseline adherence.
Integrated Management and Quality of Life
The study also assessed integrated AF management, a holistic approach to care. Patients in the intervention group reported a significant 5.1% improvement in achieving integrated management compared to controls (P = 0.01). Interestingly, despite these improvements in clinical adherence, there were no significant differences in patient-reported quality of life (QoL) scores between the two groups during the study period.
Expert Commentary: Interpreting the Data
The STEEER-AF trial underscores a critical lesson in medical education: the effectiveness of an intervention is highly dependent on the baseline ‘room for improvement.’ Stroke prevention, particularly the use of anticoagulants, has been the focus of massive public health campaigns for decades, leading to high baseline adherence. Rhythm control, however, involves more complex decision-making, including the timing of cardioversion, antiarrhythmic drug selection, and catheter ablation—areas where clinicians often feel less confident and where guidelines are more frequently updated.
Biological and Methodological Plausibility
The decision tree algorithm used in this trial (Extended Data Tables 3 and 4) reveals that the primary points of failure in adherence were often related to the ‘appropriate evaluation’ phase. Education likely succeeded in the rhythm control arm because it provided clinicians with the tools to better evaluate patient indications for advanced therapies. The lack of impact on QoL might be attributed to the short follow-up period (7.7 months), as the symptomatic benefits of rhythm control and the preventive benefits of anticoagulation often take longer to manifest in patient-reported metrics.
Conclusion and Clinical Implications
The STEEER-AF trial demonstrates that a structured, 16-week educational program can significantly improve clinician adherence to complex rhythm control guidelines. While it did not significantly impact stroke prevention—likely due to high existing adherence—the trial proves that targeted education is a viable strategy for improving the quality of AF care. For health policy experts and hospital administrators, these findings suggest that educational resources should be prioritized for clinical areas with the largest implementation gaps and the most complex decision-making pathways.
Funding and Clinical Trial Registration
This study was supported by various grants and institutional funding as noted in the primary publication. ClinicalTrials.gov registration: NCT04396418.
References
- Kotecha D, Bunting KV, Mehta S, et al. Education of healthcare professionals to improve guideline adherence in atrial fibrillation: the STEEER-AF cluster-randomized clinical trial. Nat Med. 2025 Aug;31(8):2647-2654. doi: 10.1038/s41591-025-03751-2 IF: 50.0 Q1 .
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373-498.