Highlights
Efficacy Breakthrough
The addition of tafasitamab to the lenalidomide and rituximab (R2) regimen resulted in a 57% reduction in the risk of disease progression, relapse, or death compared to R2 plus placebo.
Survival Extension
Median progression-free survival (PFS) was significantly extended to 22.4 months in the tafasitamab group versus 13.9 months in the placebo group.
Manageable Safety Profile
While adverse events were common in both arms, the triplet combination maintained a safety profile consistent with the known toxicities of the individual agents, with no new safety signals identified.
Background: The Challenge of Relapsed Follicular Lymphoma
Follicular lymphoma (FL) remains the most common indolent non-Hodgkin lymphoma. Despite its generally slow progression, the clinical course is typically characterized by a repetitive cycle of remission and relapse. Each subsequent relapse often becomes more difficult to treat, as the duration of response tends to shorten with each line of therapy. While the combination of lenalidomide and rituximab—commonly known as the R2 regimen—has become a standard of care for relapsed or refractory (R/R) follicular lymphoma, there remains a critical unmet need for therapies that can offer deeper and more durable responses.
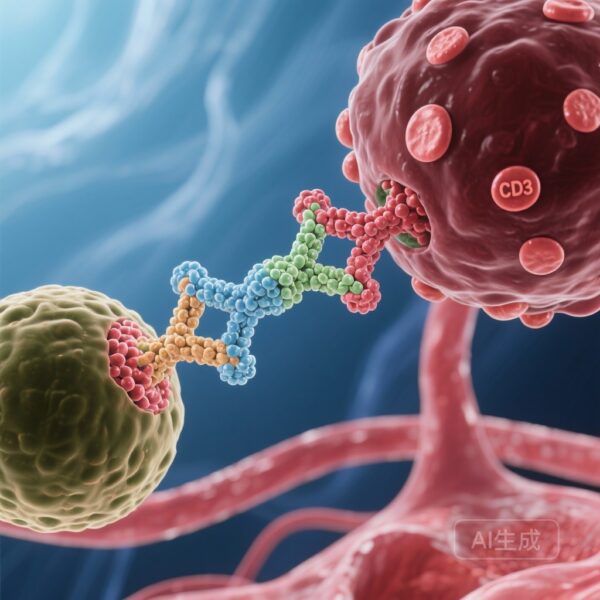
Tafasitamab is an Fc-enhanced, humanized monoclonal antibody directed against CD19. CD19 is broadly expressed throughout B-cell development and remains present on most B-cell malignancies, making it an ideal target for immunotherapy. By enhancing the Fc region, tafasitamab increases its affinity for effector cells like natural killer (NK) cells and macrophages, thereby boosting antibody-dependent cellular cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP). The inMIND trial was designed to test whether the addition of this CD19-targeted therapy could synergize with the immunomodulatory effects of lenalidomide and the CD20-targeting of rituximab to improve outcomes in R/R FL.
Study Design and Methodology
The inMIND trial was a global, phase 3, double-blind, randomized, placebo-controlled study conducted across 210 centers in North America, Europe, and the Asia-Pacific region. The study enrolled 548 adult patients with R/R follicular lymphoma who had received at least one prior line of systemic therapy. Participants were randomly assigned in a 1:1 ratio to receive either the tafasitamab triplet (tafasitamab, lenalidomide, and rituximab) or the placebo triplet (placebo, lenalidomide, and rituximab).
Dosing Schedule
The treatment consisted of up to 12 cycles, each lasting 28 days. In the tafasitamab arm, patients received 12 mg/kg intravenously on days 1, 8, 15, and 22 of cycles 1-3, and on days 1 and 15 of cycles 4-12. Lenalidomide was administered at 20 mg/day orally on days 1-21 of cycles 1-12. Rituximab was given at 375 mg/m2 intravenously on days 1, 8, 15, and 22 of cycle 1, and on day 1 of cycles 2-5. This intensive early dosing was designed to achieve rapid disease control while leveraging the synergistic potential of the three agents.
Endpoints and Assessment
The primary endpoint was investigator-assessed progression-free survival (PFS) in the intention-to-treat (ITT) population. Secondary endpoints included PFS as assessed by an independent review committee (IRC), overall response rate (ORR), and overall safety. The trial was robustly powered to detect a significant difference in PFS, reflecting its goal of establishing a new standard of care.
Key Findings: A New Standard for PFS
The results of the inMIND trial represent a significant milestone in the management of follicular lymphoma. Between April 2021 and August 2023, 548 patients were randomized. The demographic characteristics were well-balanced between the two groups, with a slight majority of male participants (55%).
Primary Efficacy Results
The primary analysis revealed a profound improvement in PFS for patients receiving the tafasitamab triplet. The median investigator-assessed PFS was 22.4 months (95% CI 19.2 to not evaluable) in the tafasitamab group, compared to 13.9 months (95% CI 11.5–16.4) in the placebo group. This translated to a hazard ratio (HR) of 0.43 (95% CI 0.32–0.58; p<0.0001), indicating a 57% reduction in the risk of progression or death. These findings were confirmed by an independent review committee, reinforcing the validity of the investigator assessments.
Secondary and Subgroup Analyses
While detailed secondary outcomes continue to mature, the early data suggests that the benefit of adding tafasitamab was consistent across various patient subgroups, including those who were refractory to their last line of therapy or those with early progression (POD24). This consistency is particularly encouraging for clinicians who manage high-risk patients who historically have poor outcomes with standard R2 therapy.
Safety and Tolerability
In any triplet combination therapy, safety is a paramount concern. In the inMIND trial, adverse events (AEs) were reported in 99% of patients in both the tafasitamab and placebo groups, reflecting the baseline toxicity of the R2 backbone. However, the addition of tafasitamab was generally well-tolerated.
Common Adverse Events
The most frequently reported AEs in the tafasitamab and placebo groups were neutropenia (49% vs 45%) and diarrhea (38% vs 28%). The higher incidence of diarrhea in the tafasitamab group was noted but was mostly low-grade and manageable with standard supportive care. Neutropenia remains a known risk of lenalidomide-based regimens, and the addition of tafasitamab did not significantly exacerbate this risk.
Serious Adverse Events and Mortality
Importantly, there were no deaths attributed to treatment-related adverse events in the tafasitamab group. In contrast, two patients in the placebo group experienced fatal treatment-related AEs. These safety data suggest that the tafasitamab triplet does not introduce prohibitive toxicity, making it a viable option for a broad range of patients, including those who may be older or have moderate comorbidities.
Expert Commentary and Clinical Implications
The inMIND trial is the first phase 3 study to demonstrate the efficacy of a triple-immunotherapy approach (targeting CD19 and CD20 while modulating the immune environment with lenalidomide) in R/R follicular lymphoma. The primary driver of this success appears to be the synergistic interaction between the three drugs. Lenalidomide is known to enhance the activity of NK cells, which in turn increases the efficacy of monoclonal antibodies like tafasitamab and rituximab through ADCC.
From a clinical perspective, a hazard ratio of 0.43 is exceptionally strong in the context of indolent lymphoma. It suggests that moving toward a more intensive, targeted triplet regimen early in the relapse setting can significantly delay the need for subsequent, potentially more toxic therapies like chemotherapy or CAR-T cell therapy. The use of a chemotherapy-free triplet also aligns with the evolving preference for targeted, immunotherapy-based approaches that preserve patient quality of life.
However, clinicians must remain vigilant regarding the management of hematological toxicities and gastrointestinal symptoms. Proactive monitoring and the use of growth factors where appropriate will be essential for maintaining patients on therapy to achieve the full benefit of the 12-cycle regimen.
Conclusion
The addition of tafasitamab to lenalidomide and rituximab provides a statistically significant and clinically meaningful improvement in progression-free survival for patients with relapsed or refractory follicular lymphoma. With a risk reduction of 57% and a manageable safety profile, this combination is poised to become a new standard-of-care treatment in this setting. Future research will likely focus on the long-term overall survival benefits and the potential for this triplet to be moved even earlier into the first-line setting for high-risk patients.
Funding and ClinicalTrials.gov
The inMIND trial was funded by Incyte. The trial is registered with ClinicalTrials.gov (NCT04680052) and EUDRA-CT (2020-004407-13). It remains active for long-term follow-up but is no longer enrolling new participants.
References
1. Sehn LH, Hübel K, Luminari S, et al. Tafasitamab, lenalidomide, and rituximab in relapsed or refractory follicular lymphoma (inMIND): a global, phase 3, randomised controlled trial. Lancet. 2026;407(10524):133-146. doi:10.1016/S0140-6736(25)01778-7.
2. Leonard JP, Trneny M, Izutsu K, et al. AUGMENT: A Phase III Study of Lenalidomide Plus Rituximab Versus Placebo Plus Rituximab in Relapsed or Refractory Indolent Lymphoma. J Clin Oncol. 2019;37(14):1188-1199.
3. Salles G, Duell J, González-Barca E, et al. Tafasitamab plus lenalidomide in relapsed or refractory diffuse large B-cell lymphoma (L-MIND): a multicentre, prospective, single-arm, phase 2 study. Lancet Oncol. 2020;21(7):978-988.