Highlights
- Exceptional technical success was achieved in 99.3% of 2,418 target visceral vessels.
- The estimated two-year primary patency rate for the BeGraft Peripheral Plus (BGP+) was 95.8%.
- Target vessel instability, a critical metric for long-term success, was observed in only 2.9% of cases.
- Freedom from branch-related re-intervention remained high at 98.4% at the two-year mark.
Introduction: The Evolution of Complex Aortic Repair
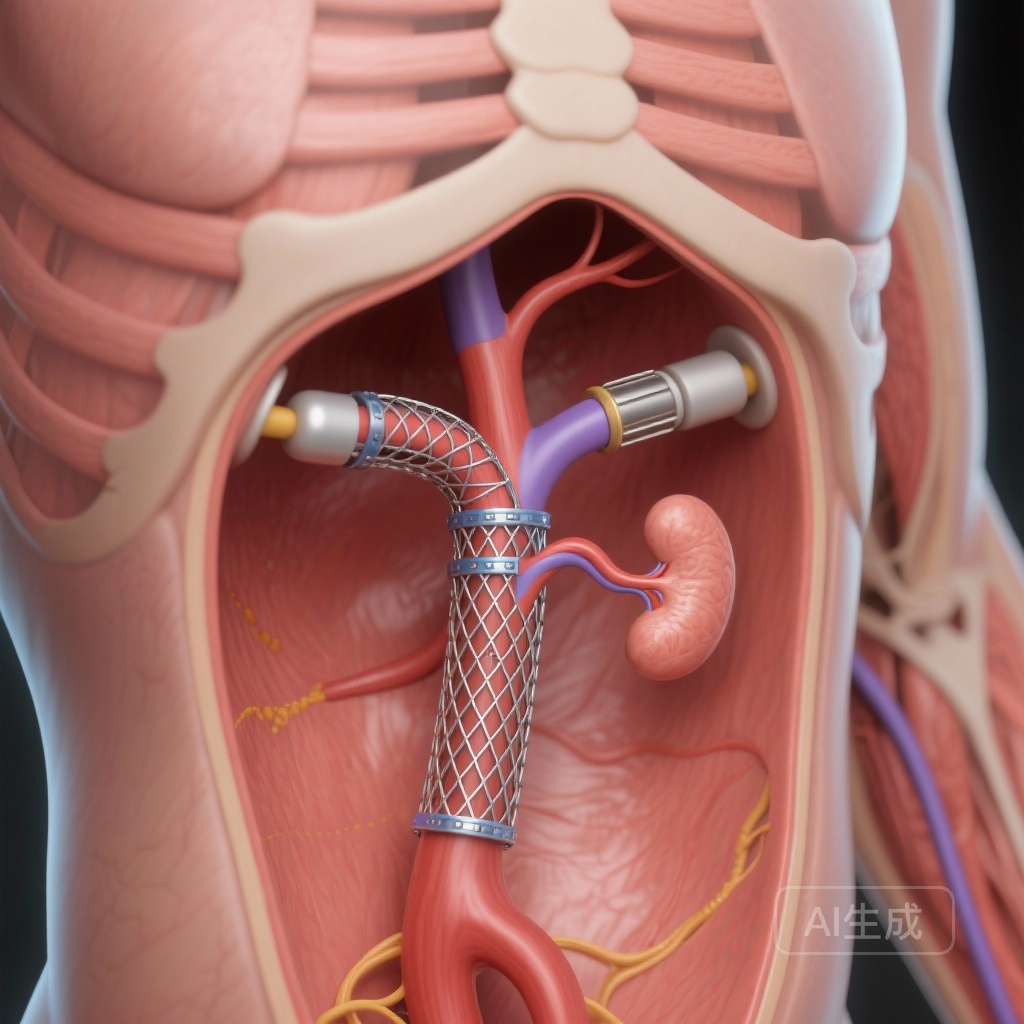
The management of thoracoabdominal aortic aneurysms (TAAAs) and complex abdominal aortic aneurysms (cAAAs) has undergone a paradigm shift over the last two decades. While open surgical repair was once the gold standard, it was associated with significant morbidity and mortality, particularly in elderly patients with multiple comorbidities. The advent of branched endovascular aortic repair (BEVAR) has provided a minimally invasive alternative that has significantly expanded the pool of treatable patients.
However, the long-term success of BEVAR is heavily dependent on the integrity of the “bridging stent”—the component that connects the main aortic endograft to the visceral arteries (celiac, superior mesenteric, and renal arteries). This junction is the “Achilles heel” of the procedure, as it is subjected to significant mechanical stress, including respiratory movement, cardiac pulsation, and anatomical angulation. Historically, clinicians used various off-label balloon-expandable or self-expanding stents. The BeGraft Peripheral Plus (BGP+) was designed specifically to address these challenges as a dedicated bridging stent. This article examines the short-term outcomes of this device based on a recent large-scale multicenter analysis.
Study Design and Methodology
This study, recently published in the European Journal of Vascular and Endovascular Surgery, aimed to provide real-world data on the performance of the BGP+ bridging stent graft. The researchers conducted a comprehensive analysis of patients treated with BEVAR that incorporated at least one outer branch for the renovisceral arteries.
Patient Population and Inclusion Criteria
The study included 729 patients who underwent BEVAR at multiple high-volume centers. These patients collectively had 2,418 target visceral vessels treated with BGP+ stents. The inclusion of such a large number of vessels provides significant statistical power to the findings and reflects the device’s performance across a wide range of anatomical variations and clinical scenarios.
Endpoints
The primary endpoints focused on technical success, branch patency (primary and secondary), and target vessel instability (TVI). TVI is a composite endpoint that includes branch-related death, branch occlusion, branch-related re-intervention, and the presence of type Ic, IIIb, or IIIc endoleaks. Secondary endpoints included 30-day mortality and the need for unplanned additional stents during the index procedure.
Detailed Clinical Outcomes
The results of the study underscore the high level of reliability offered by the BGP+ system in complex endovascular environments.
Technical Success and Immediate Results
Technical success—defined as the successful deployment of the bridging stent with preserved flow to the target vessel and the absence of major intraoperative complications—was achieved in 99.3% of the 2,418 branches. This remarkably high rate suggests that the BGP+ possesses the trackability and radial force necessary to navigate tortuous anatomy and provide a secure seal at the branch interface.
Patency Rates at One and Two Years
Long-term branch patency is the most critical measure of a bridging stent’s efficacy. The study reported:
1. Primary Patency: The estimated one-year primary patency was 98.3% (SE 0.3), which decreased slightly to 95.8% (SE 0.7) at two years. A total of 56 occlusions were noted over the follow-up period.
2. Secondary Patency: With re-intervention, the estimated one-year secondary patency was 99.2% (SE 0.2), and the two-year rate was 98.4% (SE 0.3).
These figures represent some of the most favorable patency data in the current literature for BEVAR bridging stents, particularly given the large sample size and the complex nature of the treated vessels.
Target Vessel Instability and Endoleaks
Target vessel instability (TVI) occurred in only 2.9% of branches. This low rate is indicative of the mechanical stability of the BGP+ stent. Specifically, the researchers identified seven type Ic endoleaks (T1cELs), one type 3b endoleak, and two type 3c endoleaks. The rarity of type III endoleaks (junctional or component failures) is particularly encouraging, as these often require complex secondary interventions.
Re-intervention and Safety
Freedom from branch-related re-intervention was 99.3% at one year and 98.4% at two years. The overall 30-day mortality rate was 6%, which is consistent with the global benchmarks for high-risk BEVAR procedures in patients with extensive thoracoabdominal disease.
An interesting finding was the deployment of 268 unplanned additional stents (11% of target vessels). The primary reason for these additional stents was the need for an extended seal (n = 185) or to address vessel angulation (n = 73). Only a tiny fraction were due to acute complications like vessel perforation (n = 5) or dissection (n = 4). This suggests that while the BGP+ is highly effective, the complexity of the visceral anatomy often necessitates intraoperative adjustments to ensure long-term durability.
Expert Commentary: Mechanistic Insights and Clinical Implications
The BeGraft Peripheral Plus is a balloon-expandable stent graft composed of a cobalt-chromium alloy scaffold covered with a thin ePTFE membrane. This combination provides a unique balance of high radial strength—necessary to resist the compressive forces of a calcified aortic branch—and flexibility, which is required to follow the natural curvature of the visceral arteries.
One of the most significant takeaways from this study is the confirmation of the “dedicated” stent approach. Historically, many vascular surgeons used stents designed for the iliac or peripheral arteries in the visceral positions during BEVAR. These off-label uses often resulted in higher rates of component separation or fatigue. The BGP+ results suggest that using a device optimized for the bridging role can minimize these risks.
However, the study also highlights the importance of the “landing zone” and the junctional seal. The high number of unplanned stents used to extend the seal suggests that surgeons should be prepared for anatomical challenges that exceed the length of a single stent. Furthermore, the 2.9% instability rate, while low, reminds clinicians that vigilant post-operative surveillance remains mandatory. The use of CT angiography (CTA) and duplex ultrasound in the follow-up period is essential to detect early signs of stenosis or endoleak before they progress to branch occlusion.
Limitations and Future Directions
While the study provides robust short-term data (median follow-up of 17 months), the nature of endovascular aortic repair requires five- to ten-year data to fully understand the late-term failure modes. The mechanical stresses on bridging stents are cumulative, and late component fatigue or intimal hyperplasia at the distal end of the stent graft could still occur. Future research should focus on the impact of branch angulation on long-term patency and whether specific patient populations (e.g., those with connective tissue disorders) require different bridging strategies.
Conclusion
The use of the BeGraft Peripheral Plus as a dedicated bridging stent in BEVAR procedures is associated with excellent technical success and very high short-term patency. With a target vessel instability rate under 3% and a two-year primary patency exceeding 95%, the BGP+ represents a significant advancement in the endovascular treatment of complex aortic aneurysms. While longer-term follow-up is necessary to confirm these results over the lifespan of the patient, the current data provides high confidence for clinicians incorporating this device into their BEVAR practice.
References
1. Caputo S, Jakimowicz T, Abisi S, et al. Short Term Outcomes of a Dedicated Balloon Expandable Bridging Stent in Branched Endovascular Aortic Aneurysm Repair. Eur J Vasc Endovasc Surg. 2025;S1078-5884(25)01318-8. doi:10.1016/j.ejvs.2025.12.049.
2. Haulon S, Greenberg RK, et al. Branching out: The evolution of endovascular aortic repair for thoracoabdominal aneurysms. J Vasc Surg. 2021.
3. Mastracci TM, Eagleton MJ. The Achilles heel of branched endovascular repair: The bridging stent graft. Seminars in Vascular Surgery. 2016;29(3):122-129.