Highlight
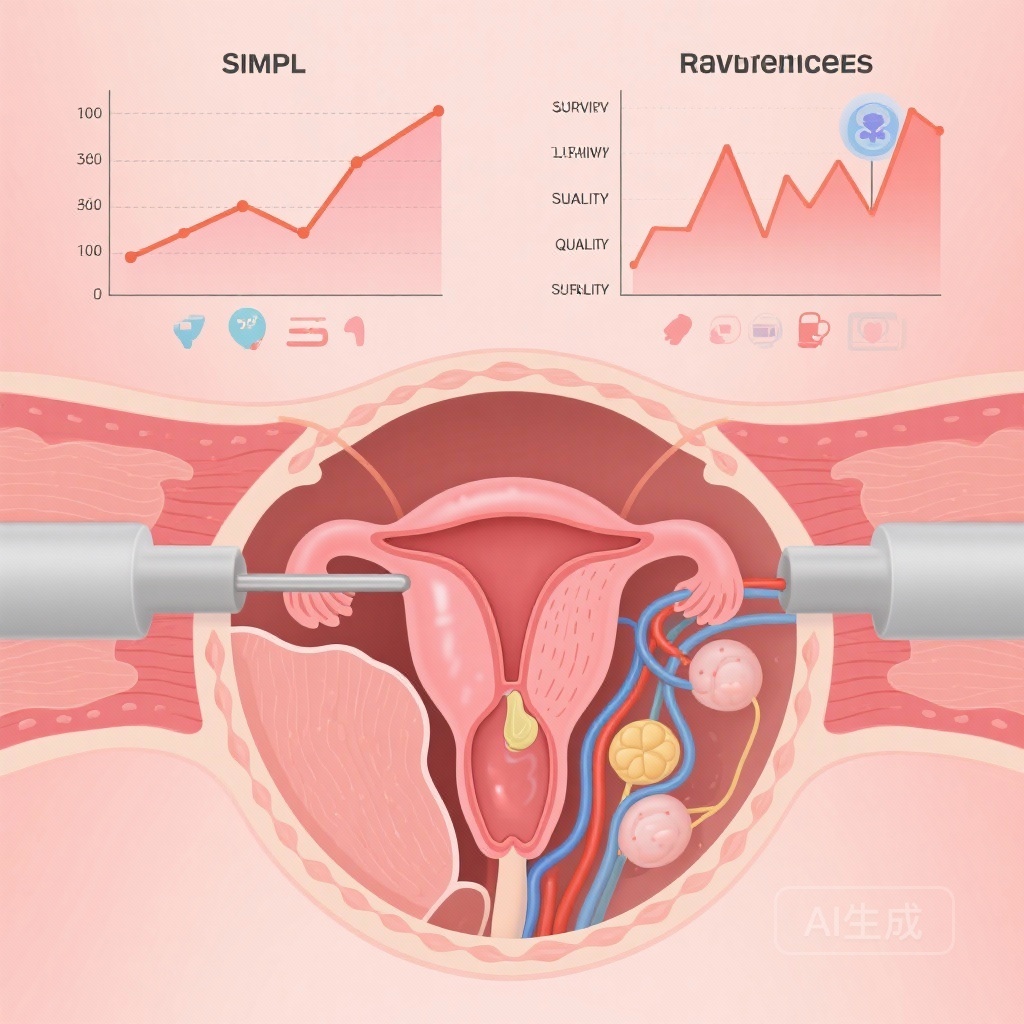
- Randomised trials show little or no difference in survival between simple and radical hysterectomy with pelvic lymphadenectomy for stage IA2–IB1 cervical cancer.
- Simple hysterectomy likely results in fewer perioperative adverse events.
- Short-term sexual function and quality of life appear better with simple hysterectomy.
- Simple hysterectomy may be cost-effective for selected patients, but evidence certainty is low to moderate.
Background
Cervical cancer remains a significant global health concern, especially in low- and middle-income countries. While radical hysterectomy has long been the surgical standard for early-stage disease, its extensive tissue removal—including parametria and part of the vagina—can lead to substantial morbidity. For carefully selected women with early-stage disease (FIGO 2019 stage IA2–IB1), where the risk of parametrial involvement is low, a less extensive approach such as simple hysterectomy with pelvic lymphadenectomy may minimise harm while maintaining oncologic safety.
Study Design
This Cochrane systematic review evaluated randomised controlled trials comparing simple hysterectomy with pelvic lymphadenectomy versus radical hysterectomy with pelvic lymphadenectomy in women with stage IA2–IB1 cervical cancer. Literature searches covered CENTRAL, MEDLINE, Embase, Web of Science, PubMed, and trial registries, with the last search conducted on 19 March 2025. Inclusion criteria focused solely on randomised trials with appropriate staging definitions. Outcomes of interest included all-cause mortality, overall survival (OS), disease-free survival (DFS), cancer-related mortality, recurrence rates, adverse events, sexual dysfunction, cost-effectiveness, and quality of life.
The review included two trials with a combined population of 740 participants. One was a small single-centre study in Brazil (40 participants), while the other was a large multicentre trial involving Western Europe, South Korea, and Canada (700 participants). Demographically, 75% of the larger trial participants were white.
Key Findings
Survival Outcomes
Low-certainty evidence suggested no significant difference between simple and radical hysterectomy in all-cause mortality (RR 1.12, 95% CI 0.44–2.89), overall survival (HR 1.26, 95% CI 0.48–3.28), or disease-free survival (HR 1.01, 95% CI 0.48–2.11). Cancer-related mortality data were highly uncertain (RR 3.64, 95% CI 0.61–21.92).
Recurrence
Rates of recurrence showed no meaningful difference (RR 1.56, 95% CI 0.73–3.35; low-certainty evidence).
Safety and Morbidity
Moderate-certainty evidence indicated that adverse events were less frequent in the simple hysterectomy group (RR 0.82, 95% CI 0.70–0.97), suggesting tangible benefits in perioperative safety.
Quality of Life and Sexual Function
At certain follow-up points, women undergoing simple hysterectomy reported better sexual function and quality-of-life scores compared to those undergoing radical hysterectomy. These outcomes, however, were inconsistently measured and subject to variability.
Cost-effectiveness
Simple hysterectomy emerged as the dominant cost-effective strategy in economic analyses provided by the included studies.
Expert Commentary
These findings support a growing interest in de-escalation of surgical treatment for selected early-stage cervical cancer patients. The potential to maintain equivalent oncologic control while reducing surgical morbidity aligns well with principles of personalised care. However, low to moderate evidence certainty warrants caution, especially given the limited geographical and ethnic diversity of the study populations. Current clinical guidelines may evolve to incorporate simple hysterectomy as an option for select patients, but broad adoption should be preceded by further trials with diverse cohorts and robust QoL assessments.
Conclusion
For women with FIGO stage IA2–IB1 cervical cancer and low parametrial involvement risk, simple hysterectomy with pelvic lymphadenectomy may offer similar survival and recurrence outcomes compared to radical hysterectomy, while potentially reducing adverse events and improving short-term quality of life. The available evidence supports cautious consideration of simple hysterectomy in multidisciplinary treatment planning, with attention to patient selection and informed consent.
Funding and Registration
No specific funding was received for the review. Cochrane protocol registration DOI: 10.1002/14651858.CD012335.
References
Kietpeerakool C, Rattanakanokchai S, Shawky M, Morrison J. Simple hysterectomy with pelvic lymphadenectomy versus radical hysterectomy with pelvic lymphadenectomy for women with stage IA2-IB1 cervical cancer. Cochrane Database Syst Rev. 2025 Oct 15;10(10):CD012335. doi: 10.1002/14651858.CD012335.pub2. PMID: 41090469; PMCID: PMC12522187.