Introduction: The Urogenital Challenge in SGLT2 Inhibitor Therapy
The therapeutic landscape for Type 2 Diabetes (T2D) has been revolutionized by Sodium-Glucose Cotransporter 2 (SGLT2) inhibitors. By promoting glycosuria, these agents offer potent glycemic control alongside significant cardiovascular and renal protection. However, the increased concentration of glucose in the urinary tract creates a favorable environment for microbial proliferation, leading to a well-documented increase in urogenital infections (UGIs). These minor yet persistent infections often compromise patient compliance and lead to the premature discontinuation of an otherwise life-saving class of medication. Recent clinical observations have suggested that the co-administration of Dipeptidyl Peptidase-4 (DPP-4) inhibitors might mitigate this risk. A pivotal study by Calvigioni et al., published in 2026, provides the first mechanistic insight into this phenomenon by examining the impact of these therapies on the resident urinary microbiota.
The Emerging Importance of the Urinary Microbiome
Historically, urine was considered sterile in the absence of infection. Modern sequencing techniques have debunked this myth, revealing a complex ‘urobiome’ that plays a critical role in maintaining mucosal integrity and preventing the colonization of pathogens. In patients with T2D, metabolic derangements and chronic hyperglycemia are known to alter various body microbiotas, but the specific characteristics of the T2D urobiome and its response to pharmacological intervention have remained poorly understood until now.
Study Design and Methodology
The study conducted by Calvigioni and colleagues was an open-label, randomized clinical trial involving 30 individuals with T2D. The participants were monitored over a 12-week period to compare the effects of two different treatment arms: Empagliflozin monotherapy (an SGLT2 inhibitor) and a combination therapy of Empagliflozin and Linagliptin (a DPP-4 inhibitor). To establish a baseline for comparison, 15 healthy individuals were included as controls.
Analytical Approaches
The researchers employed a dual-methodological approach to characterize the urinary microbiota. Real-Time quantitative PCR (qPCR) was used to determine the total bacterial load, while 16S rRNA gene sequencing allowed for high-resolution profiling of the bacterial population composition. Clinical parameters, including Body Mass Index (BMI), fasting plasma glucose, and HbA1c, were also tracked to correlate microbial changes with metabolic outcomes.
Key Findings: Urinary Dysbiosis in Type 2 Diabetes
The study first established that T2D is characterized by a distinct urinary dysbiosis. At baseline, individuals with T2D exhibited a significantly higher total bacterial load compared to healthy controls. Specifically, there was a marked abundance of the phylum Bacillota (formerly Firmicutes). The prevalence and proportion of various bacterial species differed profoundly between the two groups, suggesting that the diabetic state itself predisposes the urinary tract to an imbalanced microbial environment even before the introduction of SGLT2 inhibitors.
Differential Effects of Monotherapy vs. Combination Therapy
The most striking results of the study emerged from the comparison of the two treatment groups over 12 weeks.
Empagliflozin Monotherapy: A Shift Toward Pathogenesis
In the group receiving only Empagliflozin, the researchers observed an increase in the total bacterial load. More concerning was the specific increase in the abundance of Bacillota and Aerococcus. Aerococcus species are increasingly recognized as opportunistic uropathogens that can cause urinary tract infections, particularly in immunocompromised or diabetic populations. This finding provides a biological basis for the increased UGI risk associated with SGLT2 inhibitor use, as the drug-induced glycosuria appears to selectively favor the growth of potential pathogens.
Combination Therapy: Restoring the Microbiological Balance
Conversely, the combination of Empagliflozin and Linagliptin demonstrated a ‘restorative’ effect. Instead of further driving dysbiosis, the combination therapy moved the urinary microbial community toward a composition similar to that observed in healthy controls. Furthermore, the combination therapy significantly reduced the prevalence of potential urinary pathogens that were elevated in both the T2D baseline and the SGLT2 monotherapy group.
Clinical and Metabolic Outcomes
While both treatment arms successfully reduced BMI, the combination therapy was significantly more effective in improving glycemic markers. Fasting glucose levels and HbA1c showed significant improvement only in the group receiving both Empagliflozin and Linagliptin. This suggests that the combination not only manages the urobiome more effectively but also provides superior metabolic control.
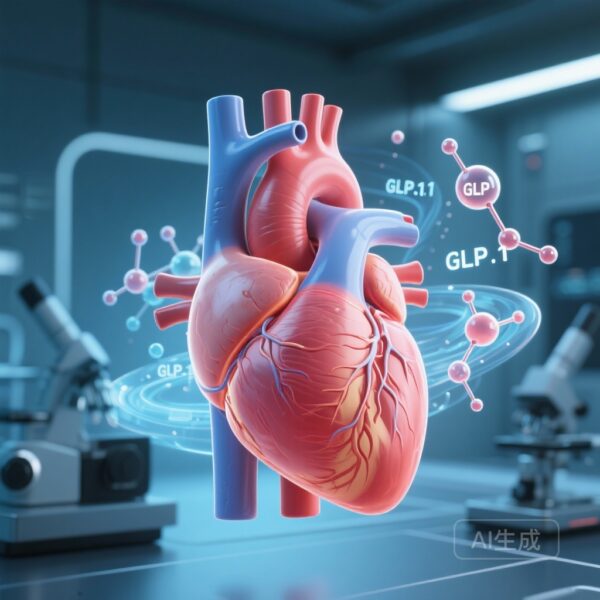
Expert Commentary and Mechanistic Insights
The finding that a DPP-4 inhibitor can ‘buffer’ the microbiological impact of an SGLT2 inhibitor is clinically significant. While the exact mechanism remains to be fully elucidated, several hypotheses exist. DPP-4 inhibitors may influence the local immune response within the urinary tract or alter the chemical composition of the urine beyond just glucose levels. Additionally, the improved systemic glycemic control seen with combination therapy may reduce the overall inflammatory state, indirectly supporting a healthier microbial environment.
Addressing Study Limitations
As with any pilot study, the sample size of 30 individuals is relatively small. The 12-week duration provides a snapshot of short-term changes, but longer-term studies are required to determine if these microbial shifts translate directly into a sustained reduction in clinical UGI episodes. Furthermore, while 16S rRNA sequencing is powerful, it does not distinguish between live and dead bacteria; future functional studies (metabolomics or transcriptomics) could provide deeper insights into the metabolic activity of the urobiome under these treatments.
Conclusion: Implications for Clinical Practice
The study by Calvigioni et al. marks a significant step forward in personalized medicine for Type 2 Diabetes. It suggests that for patients at high risk of urogenital infections—or for those who have previously struggled with SGLT2 inhibitor persistence due to side effects—the initial use of a combination therapy with a DPP-4 inhibitor may be the preferred strategy. By restoring a ‘normal’ urinary microbiota, clinicians can potentially improve therapy adherence, ensuring that patients continue to receive the long-term cardio-renal benefits of SGLT2 inhibition. This research underscores the importance of considering the human microbiome not just in the gut, but as a dynamic participant in the pharmacological response across various organ systems.
References
Calvigioni M, Biancalana E, Rossi C, Mazzantini D, Celandroni F, Ghelardi E, Solini A. Effect of SGLT2 Inhibitors + DPP-4 Inhibitors on Urine Microbiota in Type 2 Diabetes. Diabetes Metab Res Rev. 2026 Jan;42(1):e70127. doi: 10.1002/dmrr.70127. PMID: 41566786.