Highlights
- COVID-19 infection is linked to accelerated vascular aging, measured by increased carotid-femoral pulse wave velocity (PWV), approximating 5 extra years of arterial aging.
- The acceleration in vascular stiffening is most pronounced in women across all severities of COVID-19, including mild cases.
- Vaccination is associated with lower PWV and protective vascular effects in women but not significantly in men.
- Sex differences in immune responses may underlie the observed greater vascular impact in women, with persistent symptoms correlating to higher vascular aging markers.
Background
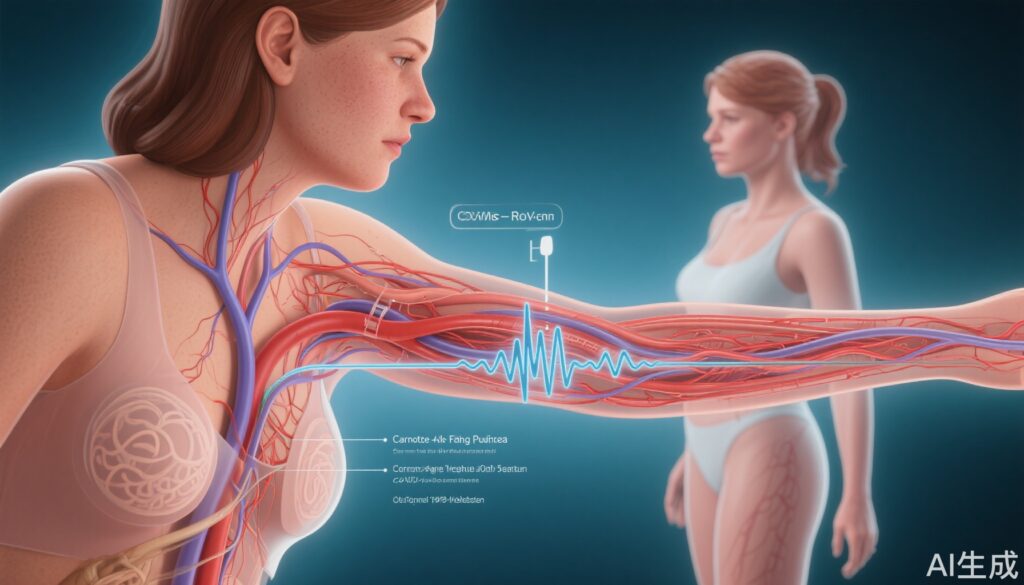
The COVID-19 pandemic has posed unprecedented challenges to global health, with accumulating evidence revealing its systemic impacts beyond acute respiratory illness. Cardiovascular complications and long-term sequelae including endothelial dysfunction, inflammation, and vascular injury have garnered particular attention. Arterial stiffness, an established surrogate of vascular aging and predictor of cardiovascular morbidity and mortality, can be non-invasively assessed by carotid-femoral pulse wave velocity (PWV). Understanding how SARS-CoV-2 infection influences vascular aging is vital for anticipating long-term cardiovascular risk.
Key Content
Study Design and Population
The CARDIOVASCULAR Aging TRansition Study after SARS-CoV-2 Infection (CARTESIAN) enrolled 2,390 participants from 16 countries between 2020 and 2022. Participants were stratified into four groups: never infected controls, COVID-19 positive non-hospitalized, hospitalized, and ICU-admitted groups. Mean age was 50 years, with 49% female. All infected individuals had positive PCR-confirmed COVID-19 diagnosis within 90 days of enrollment.
Measures of Vascular Aging
Vascular stiffness was evaluated using carotid-femoral pulse wave velocity (PWV), measured at 6 and 12 months post-infection. PWV is a validated marker of arterial stiffness, with increases reflecting accelerated vascular aging. Clinical relevance is established with every 0.5 m/s PWV increment corresponding roughly to 5 years of vascular aging.
Main Findings: PWV Changes and Sex Differences
All COVID-19 affected groups exhibited increased PWV compared to controls, indicating accelerated vascular aging. Stratified analysis revealed the following:
- Women showed significant PWV increases at all disease severities: mild cases (+0.55 m/s), hospitalized (+0.60 m/s), and ICU-treated (+1.09 m/s), correlating with 5 to over 10 years of aging.
- Men did not display statistically significant PWV differences by COVID-19 status.
- ICU-admitted COVID-positive women had a doubling of PWV relative to COVID-negative women, underscoring disease severity impact.

Vaccination Effects
Vaccination was protective in women, with vaccinated females showing significantly lower PWV values (adjusted mean 7.35 m/s) compared to unvaccinated women (7.71 m/s). No significant vaccination effect on PWV was observed in men. This suggests a sex-specific vascular benefit of COVID-19 vaccination.
Persistent Symptoms and Vascular Aging
Women experiencing long COVID or persistent symptoms exhibited higher PWV, linking ongoing symptomatology to vascular aging burden. This association was absent in men.
Immunological and Biological Insights
Lead author Dr. Rosa Maria Bruno proposed that the robust and rapid immune responses in women—a double-edged sword—may accelerate vascular damage post-infection despite offering early protection. Sex-specific immune modulation likely contributes to differing vascular outcomes.
Expert Commentary
The CARTESIAN study, published in the European Heart Journal, offers robust multinational, prospective data implicating COVID-19 as a driver of accelerated vascular aging, particularly in women. This demographic susceptibility highlights the necessity for personalized cardiovascular risk assessment post-COVID.
Experts emphasize the need for longitudinal monitoring and research into mechanistic pathways, including endothelial dysfunction, chronic inflammation, and autoimmunity, that could elucidate sex-specific vascular effects. The differential impact of vaccination supports tailored public health messaging.
Limitations include observational design restricting causal inference, potential confounders not fully captured, and uncertainties about long-term trajectories beyond 1 year.
Clinicians should consider cardiovascular follow-up in recovered COVID-19 patients, especially women, integrating vascular aging markers like PWV as part of risk stratification tools.
Conclusion
SARS-CoV-2 infection accelerates vascular aging detectable within 6 to 12 months, with women disproportionately affected. Vaccination offers protective vascular effects in females, underscoring sex-specific immune-vascular interactions. These findings mandate heightened awareness of COVID-19’s vascular legacy, advocating for further research to identify modifiable targets and optimize prevention and management strategies against pandemic-induced vascular aging.
References
- Bruno RM, Badhwar S, Abid L, et al; CARTESIAN Investigators. Accelerated vascular ageing after COVID-19 infection: the CARTESIAN study. Eur Heart J. 2025 Aug 17;ehaf430. doi: 10.1093/eurheartj/ehaf430 IF: 35.6 Q1 . Epub ahead of print. PMID: 40819656 IF: 35.6 Q1 .
- Bukhari S, et al. Editorial: The vascular legacy of COVID-19: sex-specific arterial aging implications. Eur Heart J. 2025.