Highlights
- Nonstenotic carotid disease (less than 50% stenosis) is a significant and often overlooked source of ipsilateral ischemic stroke, appearing in over 60% of the AcT trial cohort.
- High-risk plaque features, including intraluminal thrombi and carotid webs, are strongly associated with stroke risk regardless of the degree of luminal narrowing.
- The presence of an intraluminal thrombus increased the odds of a concordant stroke by over eight-fold (adjusted Odds Ratio [aOR]: 8.11).
- Clinical evaluation of carotid disease should shift focus from simple stenosis percentages to comprehensive plaque characterization.
Background: The Clinical Challenge of the Nonstenotic Carotid Artery
For decades, the management of carotid artery disease has been dictated by the degree of luminal narrowing. Guidelines from the North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST) established the 50% stenosis threshold as the primary benchmark for considering surgical or endovascular intervention. However, this focus on quantity—the percentage of narrowing—has often come at the expense of quality—the stability and composition of the plaque itself.
A significant portion of ischemic strokes are classified as “cryptogenic” or as Embolic Strokes of Undetermined Source (ESUS). Emerging evidence suggests that many of these events may actually be caused by unstable, nonstenotic (<50%) carotid plaques that shed emboli into the cerebral circulation. Despite this, patients with low-grade stenosis are frequently excluded from aggressive secondary prevention strategies beyond medical management. The study by Ignacio et al., a secondary analysis of the AcT (Alteplase Compared to Tenecteplase) trial, provides crucial data to bridge this gap in clinical understanding.
Study Design and Methodology
This cross-sectional secondary analysis utilized data from the AcT randomized controlled trial, which primarily compared two thrombolytic agents in acute ischemic stroke. The researchers evaluated baseline computed tomography angiograms (CTA) from 1,577 enrolled patients. After excluding those with uninterpretable imaging, 1,407 patients were analyzed.
The primary focus was the degree of internal carotid artery (ICA) stenosis and the presence of specific plaque features on the side ipsilateral to the stroke. These features included:
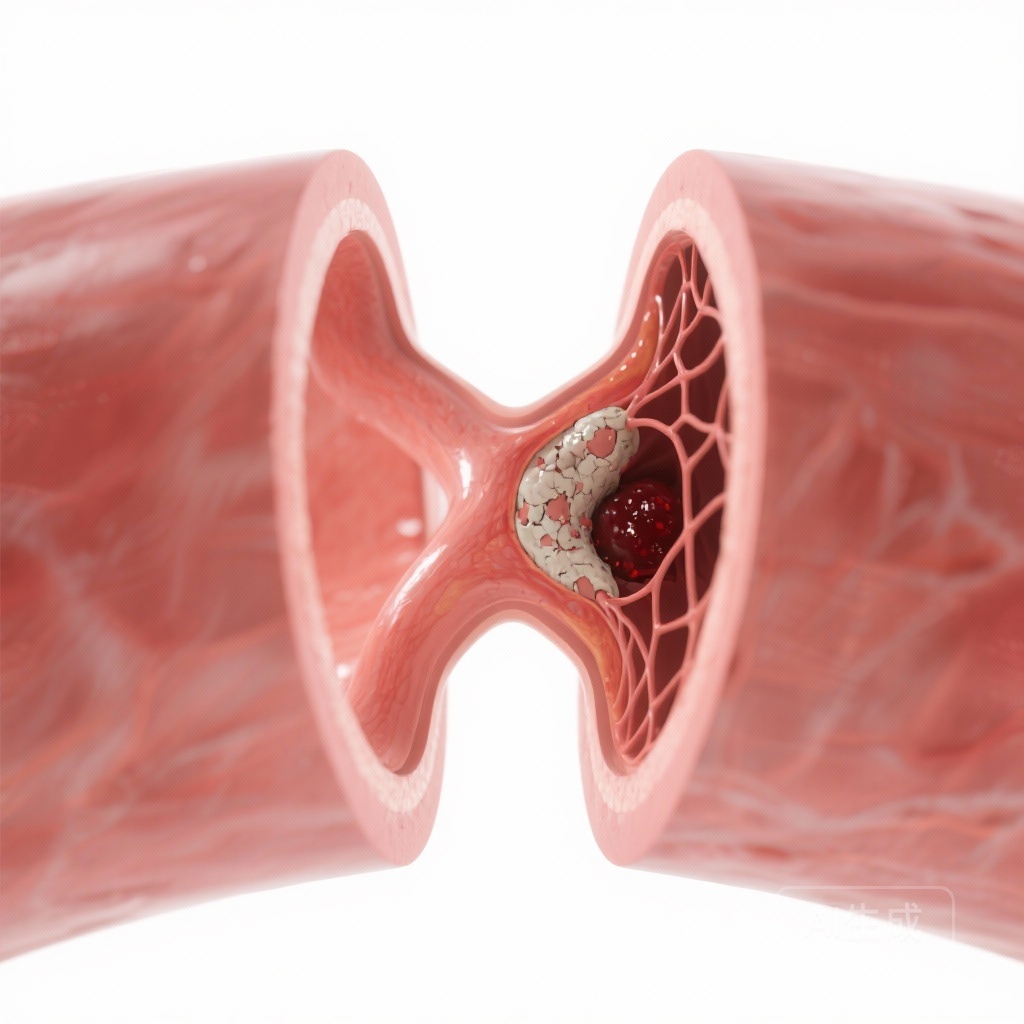
- Intraluminal thrombi (a clot attached to the vessel wall).
- Carotid webs (a thin, shelf-like projection of intimal fibrous tissue).
- Carotid dissection (a tear in the vessel wall).
- The “rim sign” (an adventurous or peripheral enhancement pattern on CTA indicative of high-risk plaque).
The researchers used mixed-effects logistic regression models, adjusting for age and sex, to examine the association between “concordant stroke” (an acute stroke occurring specifically in the territory of the ipsilateral ICA) and these nonstenotic carotid features. Follow-up imaging at 24 hours was used to confirm stroke locations.
Key Findings: Redefining “Mild” Disease
The study cohort (median age 73; 48% female) revealed a high prevalence of nonstenotic carotid disease. Of the 1,407 patients, 61.8% (n=869) had nonstenotic disease in at least one ICA, while only 14.9% had traditional stenotic disease (≥50%).
Among the 2,519 individual internal carotid arteries with nonstenotic disease, 689 (27.4%) were associated with a concordant stroke. The analysis identified several morphological features that were potent predictors of stroke risk, even in the absence of significant narrowing:
Intraluminal Thrombus
The strongest association was observed with intraluminal thrombi. Patients with this feature in a nonstenotic artery were over 8 times more likely to have a concordant stroke (aOR 8.11; 95% CI, 1.60-41.08). This underscores the immediate embolic potential of an active thrombus, regardless of whether the vessel is 10% or 90% blocked.
Carotid Webs
Carotid webs, often dismissed as incidental findings or developmental anomalies, were significantly associated with stroke (aOR 3.58; 95% CI, 1.53-8.35). Webs create local hemodynamic turbulence and blood stasis, providing a nidus for clot formation.
Carotid Dissections and the Rim Sign
Carotid dissections (aOR 6.77) and the carotid rim sign (aOR 3.17) also showed strong correlations with ipsilateral stroke. The rim sign is particularly noteworthy as it reflects underlying plaque inflammation and intraplaque hemorrhage, markers of biological instability rather than physical obstruction.
Pathophysiological Mechanisms: Beyond the Lumen
The finding that stroke risk remains high in nonstenotic vessels challenges the “plumbing model” of stroke. The mechanism is likely embolic rather than hemodynamic. In a stenotic vessel (≥70%), the stroke may be caused by reduced flow (hypoperfusion). In nonstenotic disease, the mechanism is usually “artery-to-artery embolism.”
Vulnerable plaques undergo microscopic ruptures or erosions of the fibrous cap. This exposes the highly thrombogenic core of the plaque to the bloodstream, leading to the formation of a thrombus. If this thrombus detaches, it travels downstream into the smaller arteries of the brain, causing an infarction. The AcT analysis proves that this process does not require a large plaque burden; a small, unstable plaque is just as dangerous as a large one.
Clinical Implications for Stroke Prevention
These results have profound implications for how clinicians approach both acute stroke diagnosis and secondary prevention:
1. Redefining ESUS
Many patients currently labeled with ESUS may have nonstenotic carotid disease with high-risk features. Routine CTA reporting should move beyond stating “no significant stenosis” and specifically look for and report webs, thrombi, and the rim sign.
2. Medical Management and Beyond
While current guidelines suggest statins and antiplatelets for all carotid disease, the intensity of this therapy might need to be escalated in the presence of these high-risk features. Furthermore, the role of carotid endarterectomy (CEA) or carotid artery stenting (CAS) in patients with <50% stenosis but high-risk morphology (especially carotid webs) is an area that requires urgent clinical trial investigation.
3. Imaging Protocols
The study highlights the utility of high-quality CTA in the acute setting. While duplex ultrasound is a common screening tool, it may lack the sensitivity to detect subtle features like carotid webs or the rim sign. CTA or high-resolution MRI (vessel wall imaging) should be considered standard for evaluating stroke etiology when the source is not immediately apparent.
Expert Commentary and Limitations
Experts in the field suggest that these findings represent a shift toward “precision stroke medicine.” Instead of treating a number (stenosis percentage), we are moving toward treating the specific pathology. However, the study has limitations. As a secondary analysis of a trial focused on thrombolysis, there may be selection bias toward patients who were candidates for acute intervention. Additionally, the cross-sectional nature allows for association but not definitive causality, although the biological plausibility is strong.
Further prospective studies are needed to determine if interventional strategies for nonstenotic but “symptomatic” carotid disease (e.g., stenting a carotid web) result in better outcomes than medical therapy alone.
Conclusion
The AcT trial secondary analysis provides a clear mandate for the neurovascular community: the degree of stenosis is an insufficient metric for assessing carotid-related stroke risk. Features such as intraluminal thrombi, carotid webs, and the rim sign identify a high-risk population that is currently underserved by traditional treatment algorithms. By recognizing these nonstenotic but symptomatic phenotypes, clinicians can better tailor secondary prevention and potentially reduce the burden of recurrent stroke.
References
Ignacio KHD, Nagendra S, Bala F, et al. Association Between Ipsilateral Stroke and Nonstenotic (<50%) Carotid Disease: Secondary Analysis From the AcT Trial. J Am Heart Assoc. 2026 Jan 20;15(2):e042821. doi: 10.1161/JAHA.125.042821. Epub 2026 Jan 14. PMID: 41532511.