Highlight
- Schizophrenia patients exhibit reduced brain iron levels in the substantia nigra and ventral tegmental area (SN-VTA) as measured by quantitative susceptibility mapping MRI.
- Lower SN-VTA magnetic susceptibility, reflecting diminished iron, correlates inversely with elevated striatal dopamine synthesis capacity assessed by [18F]-DOPA PET.
- The relationship persists after accounting for confounding factors such as neuromelanin and myelin content, underscoring iron’s potential role in dopaminergic dysregulation.
- These findings provide novel mechanistic insights into schizophrenia pathophysiology and raise the prospect of targeting brain iron homeostasis in future treatment strategies.
Study Background
Schizophrenia is a chronic and disabling psychiatric disorder characterized by positive symptoms (hallucinations, delusions), negative symptoms, and cognitive impairments. A central neurobiological hypothesis implicates hyperactivity of the dopaminergic system, particularly elevated dopamine synthesis and release in the striatum, as a key factor in symptom expression. However, the upstream mechanisms driving this dopaminergic dysfunction remain incompletely understood.
Recent preclinical research has demonstrated that midbrain iron deficiency can lead to striatal hyperdopaminergia. Iron is a critical cofactor in dopamine metabolism and influences neuronal function. Intriguingly, neuroimaging studies have separately reported low brain iron and elevated dopamine synthesis in schizophrenia, but the direct relationship between iron content in dopaminergic midbrain regions and striatal dopamine synthesis has not been examined concurrently in humans.
Study Design
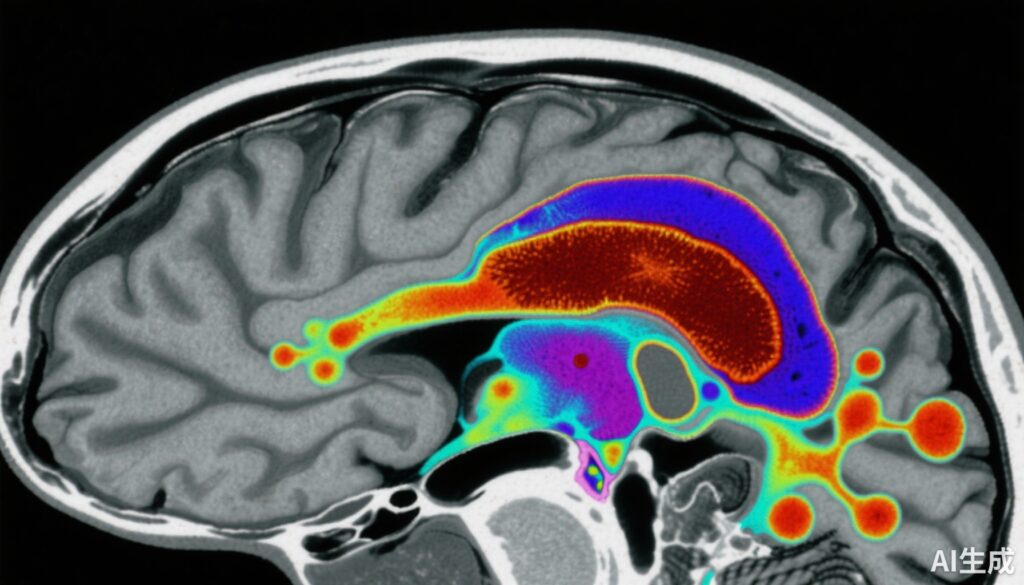
This case-control study involved 159 participants: 80 healthy controls and 79 individuals with early-course schizophrenia (including antipsychotic-naïve or antipsychotic-free patients). Magnetic susceptibility in the SN-VTA was quantitatively measured using quantitative susceptibility mapping (QSM) MRI, which provides a noninvasive marker of tissue iron levels.
To disentangle the possible confounding effects of other paramagnetic substances such as neuromelanin and structural components like myelin on QSM signals, neuromelanin-sensitive MRI (NM-MRI) and diffusion tensor imaging (DTI) were performed in a subset of 99 participants (38 controls, 61 patients).
Finally, in 40 patients with schizophrenia, dopamine synthesis capacity in the striatum was measured via [18F]-DOPA positron emission tomography (PET), enabling correlative analysis between SN-VTA iron content and dopaminergic activity.
Key Findings
The study yielded several important findings:
1. Reduced SN-VTA Magnetic Susceptibility in Schizophrenia: Patients exhibited significantly lower QSM values in the SN-VTA (effect size d = -0.66, 95% CI -0.98 to -0.34) compared to controls. This indicates diminished brain iron levels in this critical dopaminergic region.
2. Independent of Neuromelanin and Myelin Effects: Adjusting for NM-MRI contrast-to-noise ratios (reflecting neuromelanin levels) and mean diffusivity from DTI (reflecting myelin concentration) did not attenuate the observed group differences, supporting the specificity of reduced iron rather than changes in these other tissue components.
3. Inverse Correlation Between SN-VTA Iron and Striatal Dopamine Synthesis Capacity: In schizophrenia patients, lower magnetic susceptibility in SN-VTA was significantly associated with greater striatal dopamine synthesis (Ki cer) (correlation coefficient r = -0.44). This relationship remained significant after controlling for neuromelanin and myelin measures.
4. Regional Specificity: The most pronounced effects were localized to the ventral portion of SN-VTA, a region implicated in modulating striatal dopaminergic tone.
Expert Commentary
These findings elegantly link neurochemical and neuroanatomical abnormalities in schizophrenia, supporting the hypothesis that brain iron deficiency in dopaminergic midbrain nuclei contributes to maladaptive increases in striatal dopamine synthesis. Iron’s role as a cofactor in tyrosine hydroxylase activity and dopamine metabolism provides a biologically plausible mechanism for this association.
The study’s multi-modal imaging approach, controlling for confounding tissue properties, strengthens confidence in the specificity of iron-related findings. Moreover, the inclusion of antipsychotic-naïve or medication-free patients mitigates confounding by treatment effects.
Nonetheless, limitations include the cross-sectional design precluding causal inference and relatively modest sample sizes for some imaging modalities. Longitudinal studies and iron-targeting interventions are needed to clarify whether iron abnormalities are causal contributors to dopamine dysregulation and symptomatology.
These results complement and extend prior work highlighting abnormal brain iron metabolism in schizophrenia and suggest novel therapeutic avenues.
Conclusion
This study provides compelling evidence that individuals with schizophrenia have reduced non-neuromelanin-bound iron in the substantia nigra and ventral tegmental area, associated with elevated striatal dopamine synthesis capacity. These findings implicate aberrant brain iron homeostasis as a mechanistic contributor to the characteristic dopaminergic hyperactivity in schizophrenia.
Future research should explore whether modulating brain iron levels could normalize dopamine function and improve clinical outcomes. Careful evaluation of iron supplementation or chelation strategies, alongside neuroimaging biomarkers, may open innovative paths for treatment beyond dopamine receptor blockade. This work highlights the importance of integrating multimodal imaging and neurochemistry to unravel complex neurobiological underpinnings of psychiatric disorders.
Funding and Clinical Trials
The original study was supported by institutional and governmental research grants. Details on clinical trial registration were not provided in the source publication.
References
Vano LJ, McCutcheon RA, Sedlacik J, et al. Reduced Brain Iron and Striatal Hyperdopaminergia in Schizophrenia: A Quantitative Susceptibility Mapping MRI and PET Study. Am J Psychiatry. 2025 Sep 1;182(9):830-839. doi:10.1176/appi.ajp.20240512. PMID: 40887951; PMCID: PMC7618194.
Additional relevant literature includes:
– Howes OD, Kapur S. The dopamine hypothesis of schizophrenia: version III–the final common pathway. Schizophr Bull. 2009 May;35(3):549-62.
– Aquino D, Bizzi A, Grisoli M, et al. Age-related iron deposition in the basal ganglia: quantitative analysis in healthy subjects. Radiology. 2009 Feb;252(2):165-72.
– Ward RJ, Zucca FA, Duyn JH, et al. The role of iron in brain ageing and neurodegenerative disorders. Lancet Neurol. 2014 Oct;13(10):1045-60.