Highlights
Research published in JAMA indicates that Rapid recovery with extended ultraoxygenated preservation (REUP) is a viable method for Donation after Circulatory Death (DCD) heart transplants without the need for normothermic regional perfusion or ex-situ machine reanimation.
The study reported a 96% 30-day survival rate among 24 recipients, even with donor ages exceeding 40 years and total ischemic times reaching up to 8 hours.
Only 4% of patients experienced severe primary graft dysfunction (PGD), suggesting that ultraoxygenated cold storage may effectively mitigate ischemia-reperfusion injury.
REUP offers a potential solution to the high cost, technical complexity, and ethical dilemmas associated with current DCD procurement strategies.
Introduction: The Evolving Landscape of DCD Heart Transplantation
For decades, heart transplantation relied almost exclusively on Donation after Brain Death (DBD). However, the persistent shortage of donor organs has necessitated the expansion of the donor pool to include Donation after Circulatory Death (DCD). While DCD has significantly increased the number of available hearts, the procurement process is inherently more complex due to the period of warm ischemia that occurs between the withdrawal of life-sustaining therapy and the initiation of cold flush.
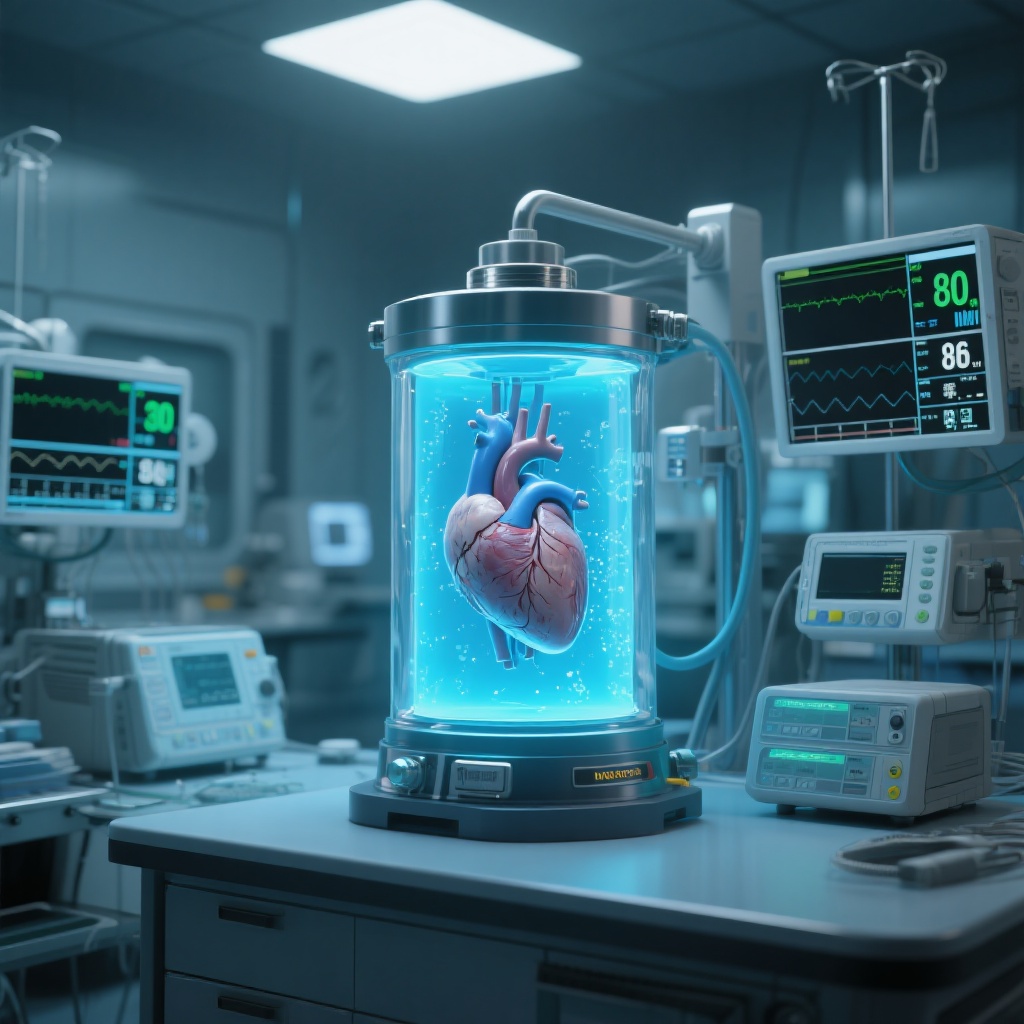
To address the injury sustained during warm ischemia, two primary strategies have dominated the field: Thoracoabdominal Normothermic Regional Perfusion (TA-NRP), which reanimates the heart within the donor’s body, and ex-situ machine perfusion (such as the Organ Care System), which keeps the heart beating and perfused with warm blood during transport. While effective, both methods have drawbacks. TA-NRP faces ongoing ethical scrutiny regarding the definition of death and the restoration of circulation, while ex-situ perfusion is notoriously expensive and logistically demanding. This study explores a third way: Rapid Ultraoxygenated Recovery (REUP), a technique that simplifies the process by bypassing the need for preimplant reanimation entirely.
Study Design and Methodology
The study, led by Williams et al. and published in JAMA (2026), was a prospective case series conducted at a high-volume heart transplant center in the United States. Between November 2024 and July 2025, researchers enrolled 24 adult patients to undergo DCD heart transplantation using the REUP technique. The objective was to assess the feasibility and safety of REUP across a broad spectrum of donor and recipient profiles, specifically removing previous restrictions on donor age or anticipated ischemic time.
The REUP Protocol
Unlike traditional methods that require the heart to be restarted before implantation, REUP focuses on optimized preservation. The procedure involves a rapid recovery phase following the declaration of circulatory death, followed by extended storage in a specialized ultraoxygenated environment. This method aims to stabilize the metabolic state of the myocardium and provide sufficient oxygen to prevent the progression of cellular injury during transport, without the mechanical complexity of a beating-heart system.
Patient and Donor Characteristics
The study population was notably diverse. The mean donor age was 32 years, but significantly, 38% of the donors were older than 40—a group often excluded from DCD protocols. The recipient pool was also high-risk, with 50% of patients having undergone a prior sternotomy, which typically complicates transplant surgery and increases the risk of adverse outcomes.
Key Findings: Survival and Graft Function
The primary outcomes of the study provide a compelling case for the efficacy of REUP. Despite the inclusion of high-risk donors and long transport times, the clinical results were excellent and comparable to, if not better than, outcomes seen with more expensive reanimation technologies.
Survival and Graft Integrity
The 30-day survival rate was 96%. This is a landmark figure for a technique that eschews the traditional reanimation phase. Perhaps even more impressive was the low incidence of severe primary graft dysfunction (PGD), which was observed in only one patient (4%). Secondary graft dysfunction was also limited to a single case. These figures suggest that the ultraoxygenated preservation successfully protected the heart from the metabolic insults of the DCD process.
Ischemic Time Thresholds
One of the most significant barriers in heart transplantation is the “ischemic clock.” Traditionally, ischemic times longer than 4 hours are associated with exponentially higher risks of graft failure. In this series, however, 60% of the donor hearts had a total ischemic time exceeding 4 hours. One heart was successfully transplanted after an 8-hour ischemic window, representing a potential paradigm shift in how far donor organs can be transported using simplified preservation methods.
Rejection and Biopsy Results
Long-term success depends on the absence of acute rejection. On the first endomyocardial biopsy, only one patient (4%) showed signs of acute cellular rejection (Grade 2R). Crucially, there were no observed cases of antibody-mediated rejection (AMR). This indicates that the REUP technique does not induce a heightened inflammatory or immunological response compared to standard procurement methods.
Mechanistic Insights: Why Ultraoxygenation Works
The success of REUP challenges the assumption that a DCD heart must be “tested” via reanimation before it can be safely transplanted. The biological plausibility of REUP lies in the mitigation of the “oxygen debt” accumulated during the warm ischemic period. By providing a super-saturated oxygen environment during cold storage, the technique may allow for the restoration of mitochondrial function and ATP stores, which are depleted when the heart stops beating.
Furthermore, by avoiding the re-initiation of blood flow in the donor (as in NRP) or the use of warm blood perfusion during transport, REUP may actually reduce the production of reactive oxygen species (ROS) that contribute to reperfusion injury. This “quiet” recovery and preservation strategy may be more protective for the delicate myocardial tissue than the more invasive reanimation protocols.
Expert Commentary and Clinical Implications
The implications of this study for the field of cardiothoracic surgery are profound. If preimplant reanimation is not strictly necessary, the barriers to DCD heart transplantation could be significantly lowered.
Cost-Effectiveness and Accessibility
Current machine perfusion systems can cost tens of thousands of dollars per use, excluding the costs of specialized personnel to manage the equipment. REUP, by utilizing optimized cold storage, could democratize DCD heart transplantation, making it accessible to smaller centers that lack the budget or technical infrastructure for ex-situ perfusion.
Ethical Considerations
The use of TA-NRP has sparked intense debate within the medical community and the public regarding whether restarting a heart in a donor violates the “dead donor rule.” REUP bypasses this controversy entirely, as the heart remains in a state of preserved arrest until it is implanted into the recipient. This could simplify the consent process and reduce the ethical burden on procurement teams.
Limitations and Future Directions
While the results are promising, the study is a single-center case series with a relatively small sample size (n=24). Larger, multicenter randomized controlled trials are needed to confirm these findings and to see if the results are reproducible across different surgical teams. Additionally, long-term follow-up beyond 30 days will be essential to determine if REUP-preserved hearts perform as well as DBD or NRP-recovered hearts over many years.
Conclusion
The study by Williams et al. demonstrates that Rapid Ultraoxygenated Recovery (REUP) is a safe, feasible, and highly effective method for DCD heart recovery. By achieving excellent 30-day survival and low rates of graft dysfunction without the need for donor heart reanimation, this technique challenges current standards of care. REUP not only accommodates older donors and extended ischemic times but also offers a simplified, cost-effective, and ethically straightforward path toward expanding the heart donor pool. As the transplant community continues to seek ways to reduce waitlist mortality, REUP stands out as a promising innovation that could redefine the future of cardiac procurement.
References
Williams AM, Trahanas J, Bommareddi S, et al. Donation After Circulatory Death Heart Transplant Without Preimplant Reanimation Using Rapid Ultraoxygenated Recovery. JAMA. 2026;335(4):e2525169. doi:10.1001/jama.2025.25169