Highlights
- Quercetin administration preoperatively leads to significantly lower postoperative pain scores following cesarean section.
- Quercetin delays the time to first analgesic request and allows for earlier physical mobilization.
- No increase in adverse effects or opioid consumption observed with Quercetin adjunct therapy.
Study Background and Disease Burden
Postoperative pain after cesarean section represents a persistent clinical challenge in obstetric care, with implications for maternal recovery, early mother-infant interaction, and long-term health outcomes. Effective analgesia is critical not only for patient comfort but also for early mobilization, breastfeeding, and reduction of chronic pain risk. Traditional regimens often rely on opioids, which can be associated with side effects such as nausea, vomiting, and delayed recovery. There is a growing interest in multimodal analgesia strategies that utilize safe, well-tolerated adjuncts to optimize pain control and minimize opioid use. Quercetin—a flavonoid found in many fruits and vegetables—has demonstrated anti-inflammatory and antioxidant effects in preclinical models, suggesting potential utility in acute pain settings.
Study Design
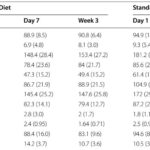
This prospective, double-blind, randomized controlled trial enrolled 80 women scheduled for elective cesarean section under spinal anesthesia at a tertiary care center. Participants were randomized to receive either 500 mg oral Quercetin (n=40) or a matching placebo (n=40) exactly one hour before surgery. The primary endpoint was postoperative pain intensity, determined via a 10 cm Visual Analog Scale (VAS) at 2, 6, 12, and 24 hours post-surgery. Secondary endpoints included time to first analgesic request, total morphine consumption, incidence of postoperative nausea and vomiting (PONV), time to initiation of physical activity, functional activity scores, patient satisfaction, and adverse effects. Study registration: NCT06650891.
Key Findings
Quercetin administration resulted in significantly lower VAS pain scores at all measured intervals compared to placebo (p<0.001), indicating robust analgesic efficacy. The mean time to first analgesic request was delayed in the Quercetin group (3.9±1.3 hours) versus placebo (2.73±0.78 hours), with statistical significance (p<0.001). Early physical activity initiation was also observed in the Quercetin arm (15.2±1.9 hours postoperatively) versus placebo (19.03±2.66 hours, p<0.001), aligning with improved patient recovery trajectories. Patient satisfaction scores were higher in the Quercetin group on postoperative day 2 (p=0.042).
Importantly, no significant differences were found between groups regarding total morphine consumption, functional activity levels, incidence of PONV, or hospital length of stay, suggesting that Quercetin’s adjunctive benefits do not stem from opioid-sparing effects but possibly from direct modulation of inflammatory and pain pathways. No increase in adverse effects was observed, underscoring the safety profile of a single 500 mg preoperative dose.
Expert Commentary
The findings from Elmokadem et al. provide compelling evidence for the analgesic potential of Quercetin as an adjunct in post-cesarean pain management. The delayed need for rescue analgesia and earlier mobilization are clinically meaningful endpoints, as early movement is associated with reduced risk of thromboembolic events and improved maternal-infant bonding. While morphine consumption was unchanged, the significant reduction in pain scores and increased patient satisfaction suggest Quercetin’s direct anti-inflammatory effects may help address aspects of pain not fully controlled by opioids. These data support further investigation into Quercetin’s mechanistic pathways—potentially involving inhibition of cyclooxygenase and NF-kB signaling—and its role in multimodal analgesia regimens.
Limitations include the modest sample size and single-center design, which may affect generalizability. The study did not explore repeated dosing or longer-term outcomes, nor did it evaluate effects in populations with comorbidities or different anesthesia modalities. Nevertheless, the rigorous methodology and clinically relevant endpoints offer important translational insights.
Conclusion
Preoperative 500 mg Quercetin confers significant benefits in reducing acute postoperative pain and accelerating mobilization after cesarean section, without increasing adverse events or opioid requirements. These findings support Quercetin’s integration into multimodal analgesic protocols, pending confirmation in larger, diverse cohorts. Future research should address optimal dosing, long-term outcomes, and mechanistic studies to solidify Quercetin’s role in obstetric pain management.
References
Mohamed Elmokadem E, Khaled Abou El Fadl D, Bassiouny AM, Mahmoud MMAE, Samy M, El Said NO. The Adjunctive Effect of Quercetin on Postoperative Pain Management Following Cesarean Section: A Randomized Controlled Study. Drug Des Devel Ther. 2025 Jul 14;19:6009-6024. doi: 10.2147/DDDT.S526188. PMID: 40687903; PMCID: PMC12273731.
For further context, see:
– Lee J, et al. Multimodal analgesia for postoperative pain management after cesarean delivery. Anesth Pain Med. 2021;16(3):205-214.
– Boots AW, et al. Health effects of quercetin: From antioxidant to nutraceutical. Eur J Pharmacol. 2008;585(2-3):325-337.