Highlights
The MANIFEST-US registry represents the largest real-world analysis of pulsed field ablation (PFA) to date, encompassing 41,968 patients across 102 U.S. centers. The study found a remarkably low major adverse event rate of 0.63%, primarily driven by vascular complications and cardiac tamponade. Notably, the study reported zero cases of atrioesophageal fistula, pulmonary vein stenosis, or persistent phrenic nerve paralysis, which are the hallmark complications of traditional thermal ablation. Additionally, the data revealed a rare signal for unexplained sudden death (0.019%), warranting further investigation into post-procedural monitoring.
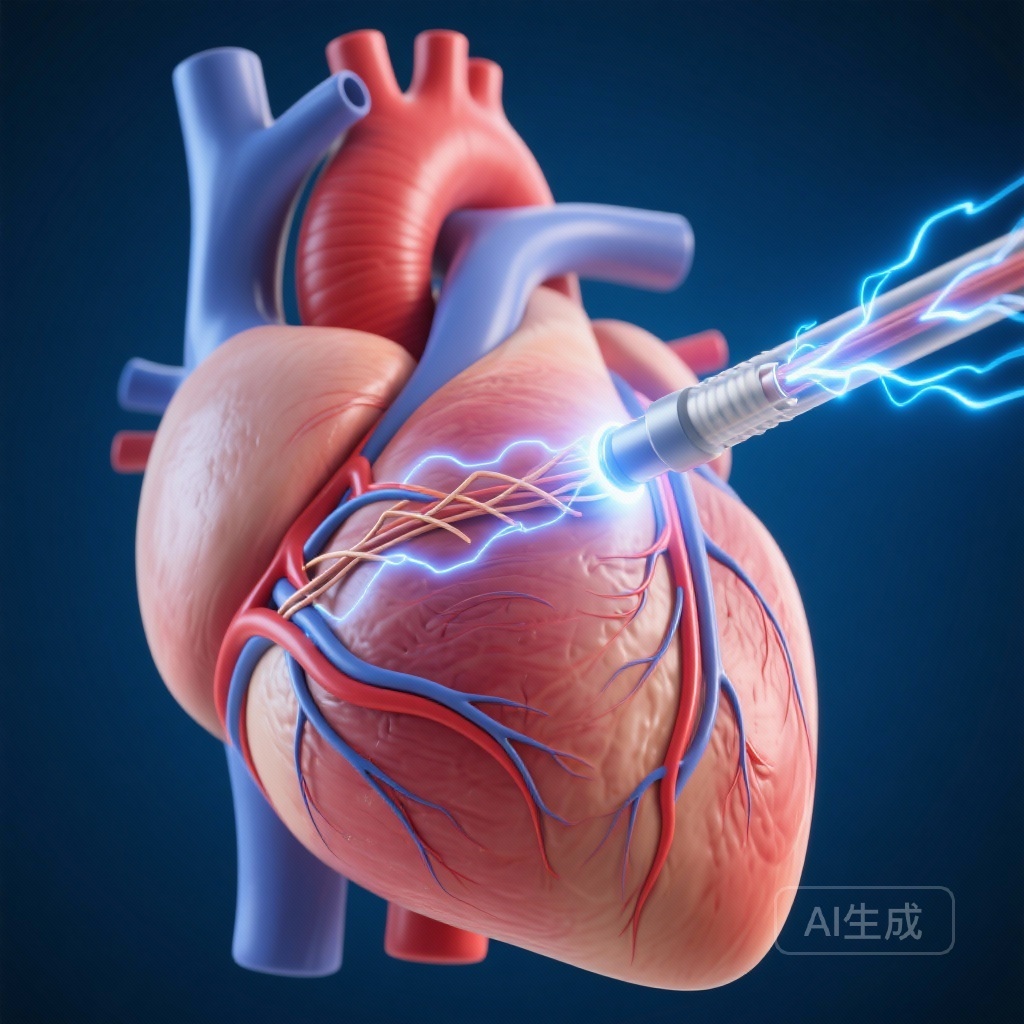
The Shift Toward Non-Thermal Energy in Atrial Fibrillation
The clinical introduction of Pulsed Field Ablation (PFA) represents a paradigm shift in the management of atrial fibrillation (AF). For decades, the standard of care for pulmonary vein isolation (PVI) has relied on thermal energy sources—either radiofrequency (RF) heat or cryoballoon cold. While effective, thermal energy is non-selective, meaning it can damage adjacent structures such as the esophagus, phrenic nerve, and pulmonary vein ostia. This lack of tissue specificity has necessitated complex mitigation strategies, such as esophageal temperature monitoring and phrenic nerve pacing, which add procedural time and do not entirely eliminate risk.
The Mechanism of Tissue Selectivity
PFA utilizes high-voltage, short-duration electrical pulses to induce irreversible electroporation (IRE). This process creates permanent nanopores in the cell membranes of cardiomyocytes, leading to cell death without the collateral damage associated with extreme temperatures. Because cardiac tissue has a lower threshold for electroporation than the esophagus or nerve tissue, PFA offers a theoretical safety advantage that has now been tested in a massive, unselected patient population through the MANIFEST-US study.
Study Design and Methodology
The MANIFEST-US study (Multicenter Study on the Safety of Pulsed Field Ablation in Over 40,000 Patients) was a retrospective analysis designed to evaluate the real-world utilization and safety of the pentaspline PFA catheter in the United States. Between February 2024 and July 2025, invitations were sent to 435 U.S. centers. Ultimately, 102 centers participated, contributing data from 518 operators. The study’s primary objective was to document the incidence of major and minor procedure-related adverse events (AEs) in a diverse patient population that included both paroxysmal and persistent AF cases.
Patient Demographics and Procedural Details
The study cohort included 41,968 patients with a median age of 68 years (ranging from 17 to 99). The population was 56% male. A significant majority of patients (73%) were undergoing their first-time ablation procedure. In terms of AF phenotype, 54% had paroxysmal AF, while 37% had persistent AF. The procedural data showed that while pulmonary vein isolation (PVI) was performed in nearly all patients (93%), many operators utilized the PFA catheter for extravenous lesions. These included the posterior wall (57%), cavotricuspid isthmus (31%), and mitral isthmus (14%), reflecting the versatility of the pentaspline design in addressing complex substrates.
Safety Outcomes: A New Benchmark for Electrophysiology
The most significant finding of MANIFEST-US is the overall major complication rate of 0.63%. In the context of cardiac electrophysiology, where thermal ablation major complication rates historically hover between 2% and 4% in large registries, these results suggest a substantial improvement in the safety margin.
Major Adverse Events
The primary major complications observed were cardiac tamponade (0.16%), vascular injuries requiring intervention (0.18%), and stroke (0.10%). The low rate of stroke (approximately 1 in 1,000) is particularly encouraging, as it suggests that the PFA energy delivery does not significantly increase the risk of thromboembolism or gaseous emboli when compared to thermal methods.
Absence of Collateral Damage
Perhaps most importantly, the study reported zero cases of atrioesophageal fistula, pulmonary vein (PV) stenosis, or persistent phrenic nerve paralysis. The absence of esophageal fistulas is a landmark result, as this complication, though rare in RF ablation (0.02% to 0.1%), is often fatal. Similarly, the lack of PV stenosis confirms the tissue-selective nature of PFA, as it avoids the collagen shrinkage and fibrotic scarring of the vein ostia typically seen with thermal injury.
Rare and Emerging Signals
While the safety profile was excellent, the study identified rare events that require clinical vigilance. The 30-day mortality rate was 0.04%, with a specific signal for unexplained sudden death or cardiac arrest in 0.019% of patients (approximately 1 in 5,000). Other rare events included coronary artery spasm (0.10%) and acute renal failure requiring dialysis (0.02%). The coronary spasm cases underscore the importance of avoiding direct PFA application in close proximity to the coronary arteries, particularly during mitral isthmus or cavotricuspid isthmus ablation.
Expert Commentary and Clinical Implications
The MANIFEST-US data provide strong evidence that PFA has moved from a promising technology to a safe clinical standard. The lack of esophageal injury simplifies the procedure, potentially removing the need for routine esophageal temperature monitoring and allowing for more efficient workflows. However, the study also highlights that vascular access remains the most frequent source of complications. This suggests that while the energy source has become safer, the mechanical aspects of large-bore catheterization still require meticulous technique, potentially benefiting from wider adoption of ultrasound-guided access.
The Learning Curve and Real-World Application
Given that the study included over 500 operators, the low complication rate suggests that PFA has a relatively flat learning curve. Unlike RF ablation, which requires precise contact force and stable catheter-tissue interface over time, PFA delivery is rapid and less dependent on prolonged stability. This may explain why the safety results remained consistent even as the technology was rolled out to hundreds of centers with varying levels of experience.
Study Limitations
Despite its scale, MANIFEST-US is a retrospective registry, which may lead to underreporting of minor adverse events. The study also focused exclusively on the pentaspline PFA catheter; therefore, the results may not be directly generalizable to other PFA platforms (such as circular or lattice catheters) that utilize different waveforms or pulse configurations. Furthermore, the signal for unexplained sudden death, while extremely rare, lacks detailed mechanistic data in this registry and necessitates prospective studies with continuous rhythm monitoring.
Conclusion
The MANIFEST-US registry confirms that pulsed field ablation using the pentaspline catheter is a highly safe modality for the treatment of atrial fibrillation in a real-world, unselected U.S. population. With a major complication rate of 0.63% and the effective elimination of thermal-related injuries like esophageal fistulas and PV stenosis, PFA establishes a new safety benchmark in cardiac electrophysiology. As the technology continues to evolve, further research will be needed to optimize lesion durability and investigate the mechanisms behind rare adverse events, but the initial large-scale implementation has been an unequivocal success.
References
Turagam MK, Aryana A, Day JD, et al. Multicenter Study on the Safety of Pulsed Field Ablation in Over 40,000 Patients: MANIFEST-US. J Am Coll Cardiol. 2025 Nov 10. doi: 10.1016/j.jacc.2025.10.051.