Highlights
- Intensity-modulated proton therapy (IMPT) achieved non-inferior progression-free survival (PFS) compared to intensity-modulated radiation therapy (IMRT) in patients with stage III/IV oropharyngeal cancer.
- Remarkably, IMPT was associated with a significant improvement in 5-year overall survival (90.9% vs. 81.0%, p=0.045) and a lower rate of deaths from disease progression.
- Proton therapy significantly reduced high-grade toxicities, including severe lymphopenia, dysphagia, and long-term gastrostomy tube dependence.
- These findings suggest that IMPT should be considered a new standard-of-care treatment for oropharyngeal cancer, balancing oncologic efficacy with a superior safety profile.
Background: The Evolution of Radiotherapy in Oropharyngeal Cancer
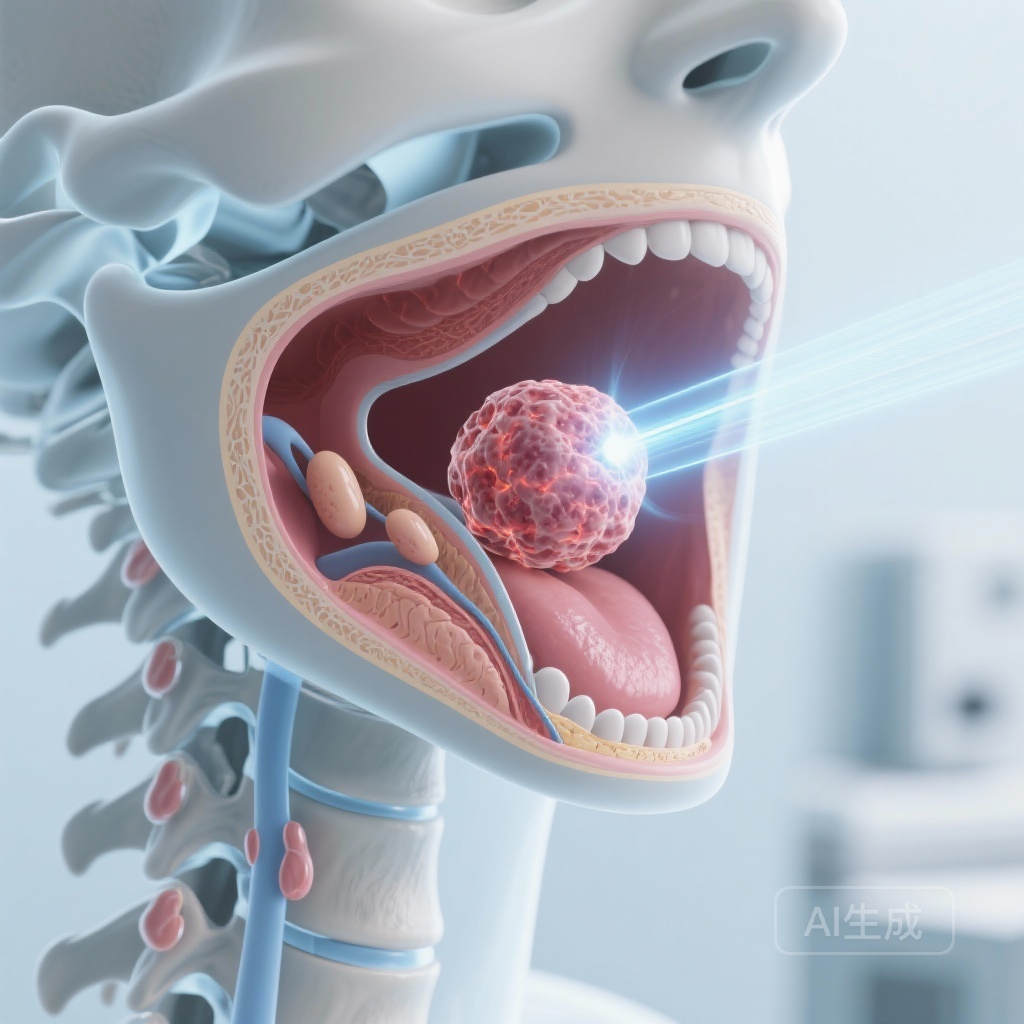
Oropharyngeal cancer (OPC) represents a significant and growing portion of the head and neck cancer burden, particularly driven by the rising incidence of human papillomavirus (HPV)-associated malignancies. While traditionally treated with surgery or radiotherapy, the current standard of care for locally advanced disease often involves concurrent chemoradiotherapy. While this approach is effective in terms of local control, the proximity of the oropharynx to critical structures—such as the salivary glands, swallowing muscles, and the spinal cord—means that photon-based intensity-modulated radiation therapy (IMRT) often results in significant acute and chronic toxicities.
Common side effects of IMRT include xerostomia (dry mouth), severe dysphagia (difficulty swallowing), and malnutrition, frequently necessitating the use of gastrostomy (G-tube) feeding tubes. Furthermore, the exit dose inherent to photon beams can lead to collateral damage to healthy tissues and circulating lymphocytes. Intensity-modulated proton therapy (IMPT) offers a theoretical advantage through the Bragg peak phenomenon, which allows for precise energy deposition within the tumor while virtually eliminating the exit dose. This multicentre, randomized, phase 3 trial sought to determine if these physical advantages translate into tangible clinical benefits for patients with oropharyngeal cancer.
Study Design and Methodology
The trial was conducted across 21 cancer centers and universities in the USA, enrolling 440 patients between 2013 and 2022. Eligible participants were adults (≥18 years) with stage III or IV oropharyngeal cancer and an ECOG performance status of 0-2. Patients were randomized in a 1:1 ratio to receive either IMPT or IMRT. Both groups received a total radiation dose of 70 Gy delivered in 33 fractions to the primary tumor and involved cervical lymph nodes.
Concurrent or induction systemic therapy was administered based on local institutional standards, ensuring the trial reflected real-world multidisciplinary care. The primary endpoint was progression-free survival (PFS) at 3 years, with a non-inferiority margin set at 9 percentage points. Secondary endpoints included overall survival (OS), local and regional recurrence rates, distant metastasis rates, and safety outcomes, specifically focusing on high-grade toxicities and G-tube dependence. PFS was analyzed in the intention-to-treat (ITT) population, while safety was assessed in the per-protocol population.
Results: Non-Inferiority and Superior Survival
Progression-Free and Overall Survival
The study successfully met its primary endpoint, demonstrating that IMPT is non-inferior to IMRT in terms of disease control. At a median follow-up of 3.2 years, the 3-year PFS rate was 82.5% for the IMPT group and 83.0% for the IMRT group. The 5-year PFS rates remained robust at 81.3% for IMPT and 76.2% for IMRT (Hazard Ratio [HR] 0.88; p=0.005 for non-inferiority).
One of the most striking findings was the difference in overall survival. The 5-year OS rate was significantly higher in the IMPT group at 90.9%, compared to 81.0% in the IMRT group (HR 0.58; 95% CI 0.34-0.99; p=0.045). This survival advantage was underpinned by a lower number of deaths related to disease progression (9 in the IMPT group vs. 18 in the IMRT group) and fewer treatment-related deaths (3 vs. 6, respectively). Despite the survival difference, local, regional, and distant control rates were statistically similar between the two groups at 5 years, suggesting that while both modalities control the tumor effectively, proton therapy may offer a survival benefit through reduced systemic toxicity or improved host resilience.
Toxicity and Quality of Life Outcomes
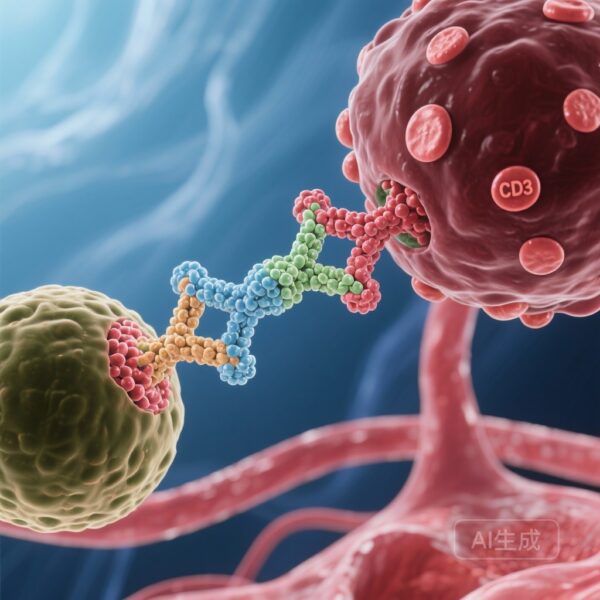
The safety profile of IMPT was markedly superior to IMRT across several key metrics. Severe (Grade 3 or higher) lymphopenia was significantly more prevalent in the photon group (89% vs. 76% in the IMPT group). Lymphopenia is increasingly recognized as a prognostic factor in head and neck cancers, as it may impair the immune system’s ability to clear residual microscopic disease.
Functional outcomes also favored proton therapy. Patients in the IMPT group experienced lower rates of dysphagia (31% vs. 49%) and xerostomia (33% vs. 45%). Most notably, the dependence on gastrostomy tubes—a major determinant of long-term quality of life—was significantly lower in the IMPT cohort at 26.8% compared to 40.2% in the IMRT cohort (p=0.018). These results highlight the ability of proton therapy to spare the constrictor muscles and salivary glands more effectively than even the most advanced photon techniques.
Expert Commentary and Mechanistic Insights
The results of this trial challenge the long-held assumption that proton therapy is merely an expensive equivalent to IMRT. The observed improvement in overall survival, while not the primary endpoint, is a profound finding that warrants deep consideration. Clinicians and researchers suggest that the reduction in “integral dose”—the total energy deposited in the patient—is the likely driver of these benefits. By sparing the circulating blood pool and bone marrow from low-dose radiation bath, IMPT preserves the immune environment, potentially enhancing the efficacy of systemic therapies and the body’s natural anti-tumor response.
Furthermore, the reduction in gastrostomy dependence is a major victory for patient-centered care. Chronic dysphagia is one of the most debilitating consequences of head and neck irradiation, leading to social isolation, depression, and recurrent aspiration pneumonia. The 13.4% absolute reduction in G-tube dependence observed in this trial represents a clinically meaningful improvement in the survivorship experience.
However, implementation of IMPT remains hindered by high capital costs and limited availability. While this trial provides the high-level evidence needed to justify its use, health policy experts must now grapple with the cost-effectiveness of broader adoption. Critics may point to the open-label nature of the trial, but the objective nature of survival and G-tube dependence data mitigates many concerns regarding observer bias.
Conclusion and Clinical Implications
This phase 3 multicentre trial provides definitive evidence that intensity-modulated proton therapy is a highly effective and safer alternative to IMRT for patients with oropharyngeal cancer. By achieving non-inferior progression-free survival while significantly improving overall survival and reducing the burden of treatment-related toxicity, IMPT establishes itself as a new standard-of-care option.
For clinicians, these data support the early referral of OPC patients to proton centers where available. For the broader medical community, this study underscores the importance of physical precision in radiation delivery and its direct impact on systemic outcomes. Future research should focus on identifying which specific subgroups of patients (e.g., those with larger tumors or specific comorbidities) derive the greatest benefit from proton therapy to optimize resource allocation.
Funding and ClinicalTrials.gov
This study was funded by the MD Anderson Cancer Center, Massachusetts General Hospital, the National Institutes of Health (NIH), and Hitachi America. The trial is registered with ClinicalTrials.gov under the identifier NCT01893307.
Reference
Frank SJ, Busse PM, Lee JJ, et al. Proton versus photon radiotherapy for patients with oropharyngeal cancer in the USA: a multicentre, randomised, open-label, non-inferiority phase 3 trial. Lancet. 2026 Jan 10;407(10524):174-184. doi: 10.1016/S0140-6736(25)01962-2.