Highlight
- Prophylactic permanent pacemakers (PPI) are implanted in about 24% of TAVR patients requiring pacing.
- Primary indication is persistent left bundle branch block with marked PR/QRS prolongation.
- 30-day pacing burden is significantly lower in prophylactic PPI patients compared to non-prophylactic PPI recipients.
- Findings challenge the rationale for routine prophylactic PPI post-TAVR.
Background
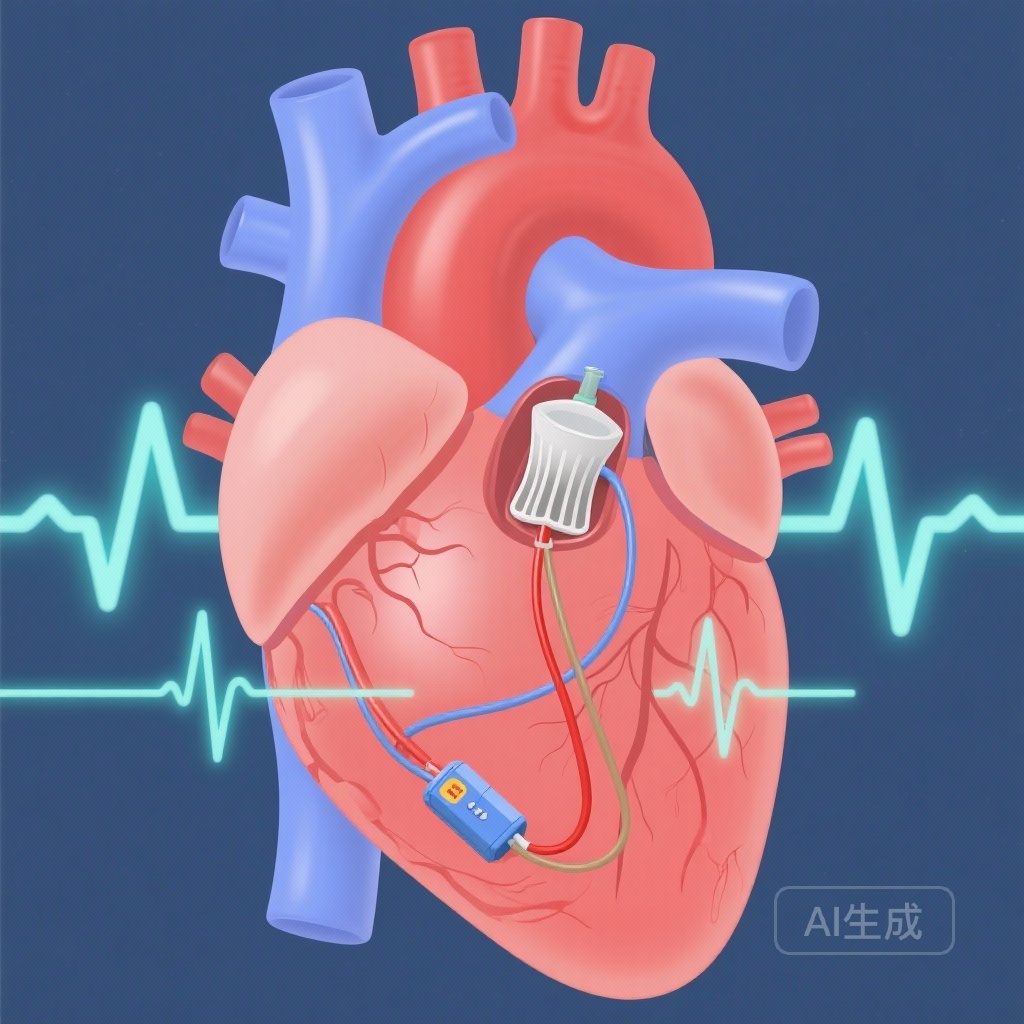
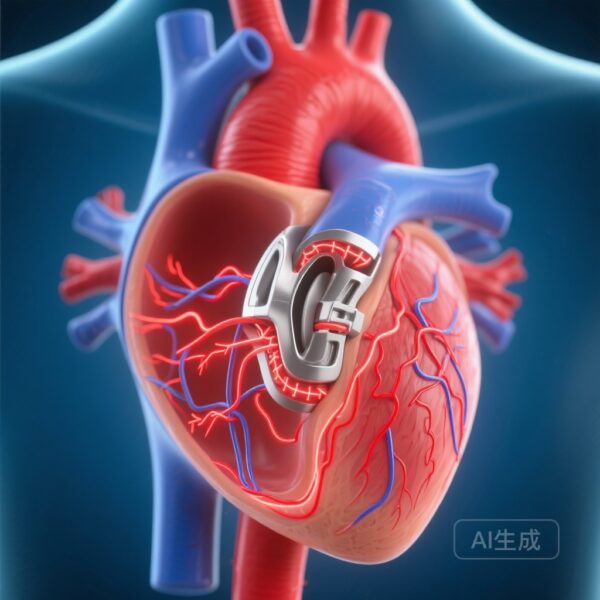
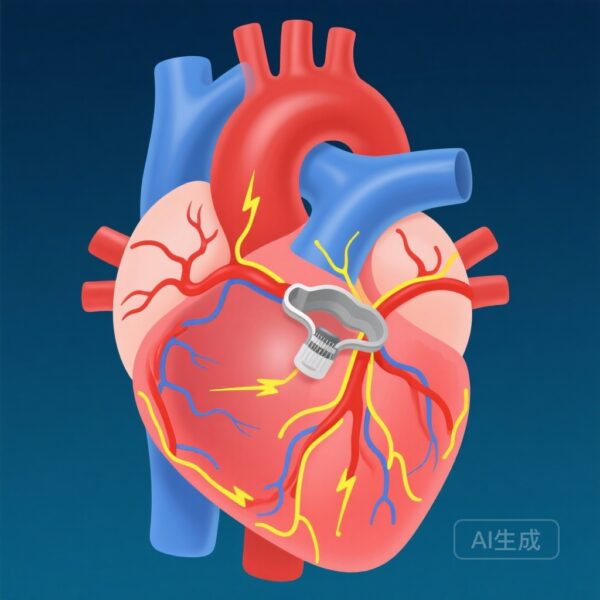
Transcatheter aortic valve replacement (TAVR) has revolutionized the management of severe aortic stenosis, particularly in elderly and high-risk surgical patients. However, its proximity to the cardiac conduction system poses a well-described risk of conduction disturbances, such as left bundle branch block (LBBB) and complete heart block, potentially necessitating permanent pacemaker implantation (PPI). Clinical decision-making regarding immediate versus delayed PPI remains contested, with prophylactic implantation often performed to mitigate adverse outcomes, despite concerns about unnecessary device dependency and associated risks.
Study Design
The PROMOTE trial subanalysis evaluated 2,110 consecutive TAVR patients without prior pacemaker implants across multiple centers. Prophylactic PPI was considered when patients developed marked conduction changes—specifically, daily PR or QRS interval prolongation of ≥20 ms over two consecutive days, or new-onset persistent conduction abnormalities (QRS >150 ms or PR >240 ms). Clinical outcomes and device utilization were assessed at 30 days.
Population
Researchers focused on 329 patients receiving post-TAVR PPI, with 80 (24.3%) meeting prophylactic criteria.
Interventions
Prophylactic pacemaker placement without prior high-grade heart block diagnosis, largely for persistent LBBB with prolonged QRS/PR intervals.
Endpoints
Primary outcomes were clinical events and ventricular pacing burden at 30 days. Secondary analyses explored the role of electrophysiologic study (EPS) thresholds (His-Ventricle interval ≥70 ms) in pacing utilization.
Key Findings
Among prophylactic PPI recipients, 90% were indicated due to persistent LBBB with significant QRS (>150 ms) and/or PR (>240 ms) prolongation. At 30 days, clinical outcome measures such as mortality, hospitalization, or cardiovascular events did not significantly differ between prophylactic and non-prophylactic PPI groups.
The striking difference emerged in pacing utilization: prophylactic PPI patients exhibited a median ventricular pacing burden of only 2% compared to 73% in non-prophylactic PPI recipients (P < 0.001). Furthermore, 42.6% of prophylactic PPI patients had a pacing burden of under 1%, versus 14.5% of non-prophylactic peers (P < 0.001).
Electrophysiologic study-guided prophylactic implantation did not substantially alter pacing burden compared with cases without EPS (median 2.0% vs 1.9%, P = 0.585).
Expert Commentary
These results highlight a significant proportion of prophylactic pacemaker recipients after TAVR who remain minimally device-dependent. While current practice often favors prophylactic implantation to preempt late-onset conduction deterioration, the low utilization rates raise concerns of overtreatment and long-term device-related complications, such as lead malfunction, infection, and tricuspid regurgitation. Experts suggest reevaluating guidelines and incorporating extended ECG surveillance post-TAVR to better identify patients truly in need of pacing support. The absence of outcome differences between groups further argues for a more conservative, individualized approach.
Conclusion
Routine prophylactic pacemaker implantation after TAVR may not be justified for all patients exhibiting conduction disturbances, particularly when pacing burden is minimal. The findings from the PROMOTE trial subanalysis call for refined patient selection algorithms, longer observation before permanent device commitment, and targeted EPS utilization. Further longitudinal studies are warranted to explore delayed conduction recovery and long-term implications of conservative versus prophylactic pacing strategies.
Funding and ClinicalTrials.gov
This subanalysis is part of the PROMOTE trial (NCT04139616). Funders and institutional affiliations were reported in the original publication.
References
Fischer Q, Nombela-Franco L, Muntané-Carol G, et al. Prophylactic Permanent Pacemaker Implantation After Transcatheter Aortic Valve Replacement. JACC Clin Electrophysiol. 2025 Nov;11(11):2484-2492. doi:10.1016/j.jacep.2025.07.028. PMID: 40965381.