Highlights
- Higher adherence to the Planetary Health Diet (PHD) is associated with a substantially lower risk of myocardial infarction (63% reduction) among women with a history of gestational diabetes (GD).
- Elevated PHD adherence correlates with reduced incidence of overall cardiovascular disease (CVD) and type 2 diabetes (T2D), with body mass index (BMI) playing a significant mediating role.
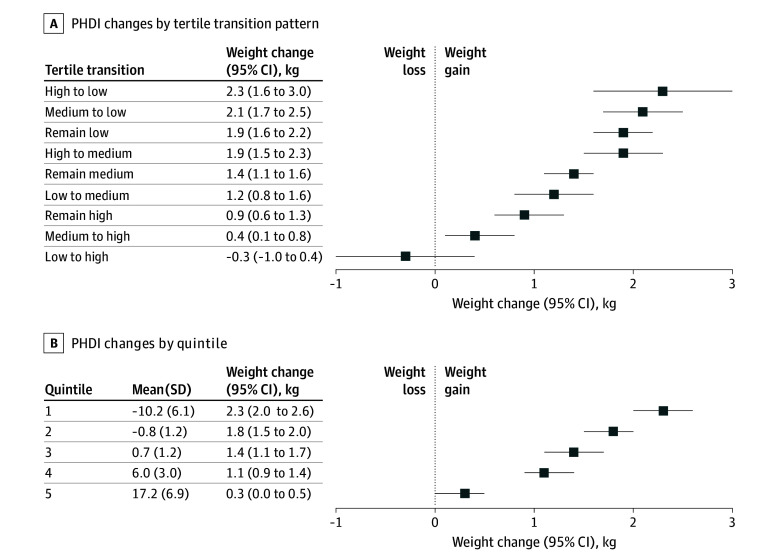
- Change in diet quality, measured by the Planetary Health Diet Index (PHDI), significantly affects concurrent weight changes; decreases in PHDI align with greater weight gain during follow-up.
- Findings emphasize the critical window postpartum for dietary interventions to mitigate long-term cardiometabolic risks in women with GD history.
Background
Gestational diabetes mellitus (GDM) affects a significant proportion of pregnant women worldwide and confers increased long-term risks of type 2 diabetes (T2D) and cardiovascular disease (CVD). The postpartum period is a crucial time for intervention to reduce these risks. However, sustainable dietary patterns that simultaneously support health and the environment are underexamined in this high-risk population.
The Planetary Health Diet (PHD), formulated by the EAT-Lancet Commission, integrates nutritional adequacy with environmental sustainability, emphasizing plant-based foods, limited red meat and processed foods, and moderate dairy and seafood intakes. While the PHD has gained attention for reducing population-level chronic disease risks and environmental impact, its specific role among women with a history of GDM remains understudied.
Key Content
Cohort Evidence on PHD and Cardiometabolic Outcomes in Women with Prior GDM
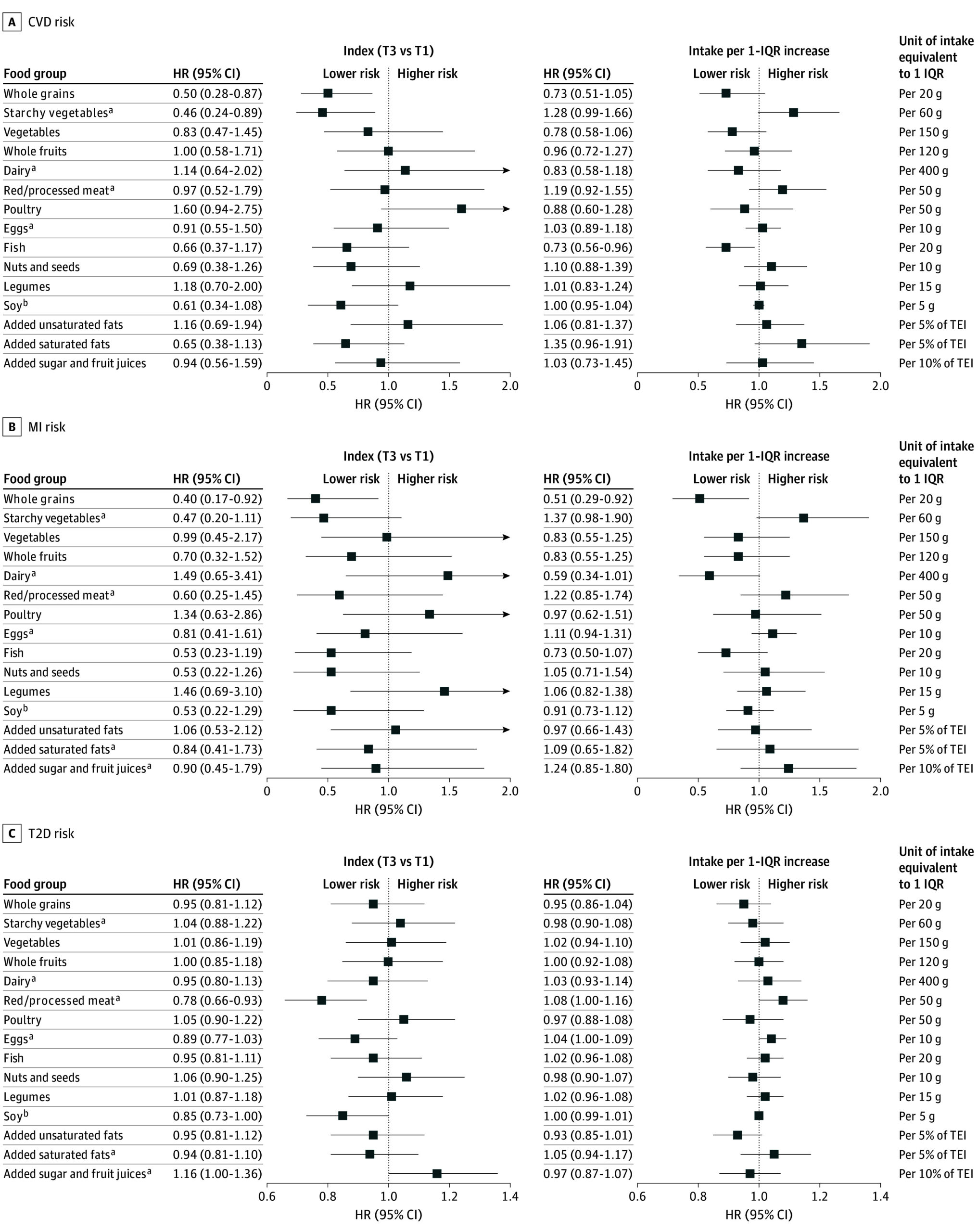
The landmark study by Yin et al. (2025), analyzing 4,633 women with prior GDM from the Nurses’ Health Study II over nearly 30 years (1991–2021), demonstrated that adherence to the PHD—quantified via the Planetary Health Diet Index (PHDI)—was inversely associated with T2D, myocardial infarction (MI), stroke, and overall CVD incidence. During 120,465 person-years, 1,053 new T2D cases and 90 CVD events occurred.
Women in the highest PHDI tertile had a 63% lower hazard for MI (HR 0.37; 95% CI: 0.16–0.86; P for trend=.01). Overall CVD and T2D risks similarly decreased with higher adherence, although BMI accounted for most of the association with T2D (approximately 80%) and a smaller but significant proportion for CVD (~15%). These results held after adjustment for confounders, including lifestyle and demographic factors, underscoring diet quality’s independent benefit.
Figure 1. Hazard Ratios (HRs) for Each Food Component of the Planetary Health Diet Index for Cardiovascular Disease (CVD), Myocardial Infarction (MI), and Type 2 Diabetes (T2D) Risk Among Women With a History of Gestational Diabetes.
Figure 2. Association Between 4-Year Change in Planetary Health Diet Index (PHDI) and Least Squares Means of Weight Change Among Women With a History of Gestational Diabetes.
Mechanistic Insights and BMI Mediation
The pronounced mediation by BMI suggests that weight management is a key pathway through which PHD adherence mitigates T2D risk. The dietary components of the PHD—high in fiber, unsaturated fats, and micronutrients from plants—are known to improve insulin sensitivity and reduce systemic inflammation. Additionally, adherence promotes healthier energy balance, reflected in lower weight gain.
Multivariable marginal models showed that decreasing PHDI over 4-year intervals corresponded to significant weight gain (P for trend < .001), where women with the largest PHDI decline gained on average 2.3 kg within 4 years. This weight gain may exacerbate insulin resistance and cardiovascular risk.
Integration with Broader Literature
Although few studies specifically assess PHD in women with prior GDM, broader evidence supports plant-forward dietary patterns to reduce cardiometabolic risk:
- Plant-Based and Mediterranean Diets: Meta-analyses indicate plant-based and Mediterranean diets decrease T2D incidence, improve glycemic control, and lower cardiovascular events (Ley et al., 2014; Satija et al., 2016).
- Postpartum Intervention Trials: Dietary counseling emphasizing whole grains, fruits, vegetables, and low red meat intake leads to improved weight retention and metabolic profiles in GDM survivors (Catalano et al., 2015; Mapprasert et al., 2021).
- Sustainability and Health Synergy: The PHD uniquely combines sustainability goals with cardiometabolic health, thus representing a dual-benefit strategy aligning with global health priorities (Willett et al., 2019).
Methodological Strengths and Limitations
The extended follow-up and repeated diet assessments in the Nurses’ Health Study II cohort provide robust longitudinal evidence. Use of validated FFQs and the composite PHDI allow comprehensive dietary pattern analysis. Mediation modeling delineates BMI’s role.
Limitations include the observational design precluding definitive causal inference and potential residual confounding. The cohort primarily consists of US nurses, possibly limiting generalizability to more diverse populations. Also, diet FFQs administered every 4 years may miss short-term dietary changes.
Expert Commentary
The findings from Yin et al. corroborate the emerging recognition of the PHD as an effective dietary strategy to manage cardiometabolic risk post-GDM. Managing BMI is pivotal, as weight gain correlates strongly with progression to T2D and CVD.
While clinical guidelines acknowledge lifestyle modifications post-GDM, current recommendations often emphasize individualized nutrition rather than holistic dietary patterns. Incorporation of PHD concepts may provide a standardized, evidence-backed framework that also aligns with planetary sustainability.
Mechanistically, the PHD’s emphasis on plant-based foods, reduced red meat, and limited processed food intake targets metabolic pathways linked to insulin resistance, dyslipidemia, and vascular inflammation. The demonstrated protective effect against MI is particularly noteworthy, given the elevated cardiovascular risk in this population.
Future interventional studies are warranted to confirm causality and evaluate the feasibility and acceptability of PHD implementation in diverse postpartum populations with GDM. Moreover, cost-effectiveness analyses could support policy-level endorsement integrating environmental and health benefits.
Conclusion
Adherence to the Planetary Health Diet among women with a history of gestational diabetes is associated with significantly lower risk of myocardial infarction and type 2 diabetes, largely mediated by effects on body weight. Longitudinal data underscore diet quality and weight management as critical targets to mitigate the progression from GDM to chronic cardiometabolic diseases.
The integration of health-promoting dietary patterns with sustainability goals positions the PHD as a promising model for postpartum dietary management. Clinical adoption and public health strategies should focus on supporting sustainable, high-quality diets to improve long-term outcomes for women with prior gestational diabetes.
References
- Yin X, Yang J, Wang DD, Hu FB, Willett WC, Zhang C. Planetary Health Diet and Risk of Cardiometabolic Diseases Among Women With Gestational Diabetes. JAMA Netw Open. 2025 Nov 3;8(11):e2540170. doi: 10.1001/jamanetworkopen.2025.40170 IF: 9.7 Q1 . PMID: 41201804 IF: 9.7 Q1 ; PMCID: PMC12595533 IF: 9.7 Q1 .
- Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447-492. doi:10.1016/S0140-6736(18)31788-4 IF: 88.5 Q1
- Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383(9933):1999-2007. doi:10.1016/S0140-6736(14)60613-9 IF: 88.5 Q1
- Satija A, Bhupathiraju SN, Spiegelman D, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. 2017;70(4):411-422. doi:10.1016/j.jacc.2017.05.047 IF: 22.3 Q1
- Catalano PM, McIntyre HD, Cruickshank JK, et al. The Hyperglycemia and Adverse Pregnancy Outcome Study: associations with pregnancy outcomes and potential evaluation in future trials. Diabetes Care. 2015;38(3):487-494. doi:10.2337/dc14-1326
- Mapprasert T, Pouyarot S, Weerapakorn W. Effectiveness of nutritional intervention in postpartum women with a history of gestational diabetes mellitus: a systematic review and meta-analysis. Nutrients. 2021;13(12):4301. doi:10.3390/nu13124301 IF: 5.0 Q1