Highlights
The PARTHENOPE trial provides landmark evidence for the clinical superiority of individualized dual antiplatelet therapy (DAPT) strategies. The key findings include:
- Personalizing DAPT duration between 3 and 24 months based on validated risk scores significantly reduced the primary endpoint of Net Adverse Clinical Events (NACE) at 24 months compared to a fixed 12-month regimen.
- The benefit was primarily driven by a significant reduction in ischemic complications, specifically myocardial infarction (MI) and urgent target vessel revascularization (TVR).
- Importantly, the personalized approach did not lead to a statistically significant increase in major bleeding events (BARC type 2, 3, or 5) compared to the standard 12-month therapy.
- These results challenge the conventional 12-month ‘one-size-fits-all’ DAPT standard, suggesting that a precision-medicine approach to antithrombotic duration optimizes the balance between ischemic and hemorrhagic risks.
Background: The Challenge of DAPT Duration
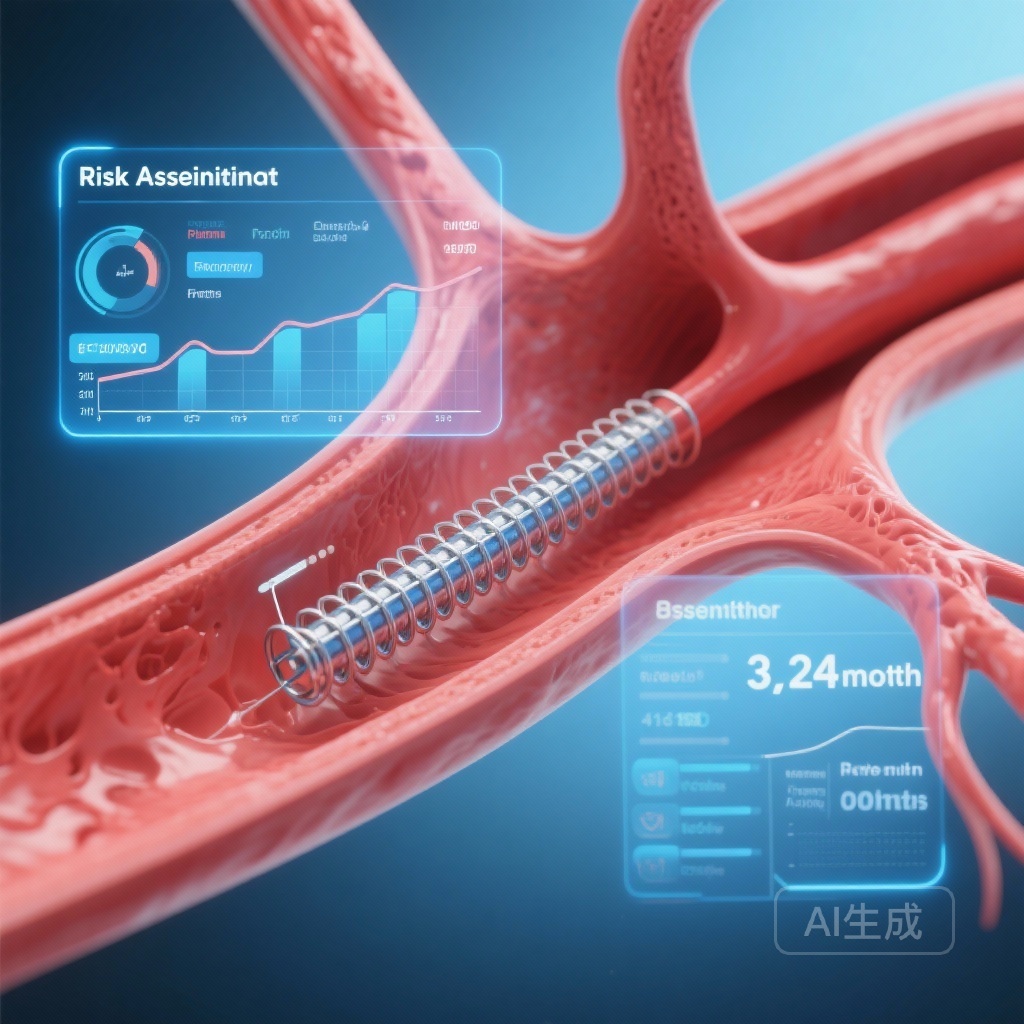
For decades, dual antiplatelet therapy (DAPT)—the combination of aspirin and a P2Y12 inhibitor—has been the cornerstone of pharmacological management following percutaneous coronary intervention (PCI) with stent implantation. While DAPT is essential to prevent stent thrombosis and recurrent ischemic events, it inherently increases the risk of bleeding, which is itself associated with increased morbidity and mortality.
Current clinical guidelines have traditionally recommended a standard 12-month DAPT duration for patients with acute coronary syndromes (ACS) and 6 months for those with chronic coronary syndromes (CCS). However, the optimal duration remains a subject of intense debate. Recent trials have explored both ultra-short DAPT (1–3 months) followed by P2Y12 inhibitor monotherapy and extended DAPT (beyond 12 months). The clinical dilemma lies in the fact that a patient’s risk for ischemia and their risk for bleeding are often dynamic and discordant. A ‘standard’ duration may over-treat those at high bleeding risk or under-treat those at high ischemic risk. The PARTHENOPE trial sought to determine if a risk-score-based, personalized duration could resolve this therapeutic tension.
Study Design and Methodology
The PARTHENOPE trial (NCT04135989) was a multicenter, randomized controlled trial that employed a pragmatic approach to evaluate DAPT strategies in a ‘real-world’ PCI population. The study enrolled 2,107 patients undergoing PCI at various clinical centers.
Patient Population and Randomization
Patients were randomized in a 1:1 ratio to either a personalized DAPT strategy or a standard DAPT strategy. Inclusion criteria were broad, encompassing patients with both ACS and CCS, reflecting the diversity of daily clinical practice. A secondary randomization also compared polymer-free versus biodegradable-polymer drug-eluting stents (DES), though the primary focus remained the antithrombotic duration.
Intervention: Personalized vs. Standard
In the standard group, patients received DAPT for a fixed duration of 12 months, followed by aspirin monotherapy. In the personalized group, the duration was determined at the time of PCI based on a clinical risk score assessment (integrating factors such as age, prior MI, renal function, and bleeding history). Based on this risk stratification, patients in the personalized arm were assigned to one of three durations:
- 3 months: For patients at high bleeding risk.
- 6 months: For patients at intermediate risk.
- 24 months: For patients at high ischemic risk and low bleeding risk.
Endpoints
The primary endpoint was a Net Adverse Clinical Event (NACE) at 24 months. NACE was defined as a composite of all-cause death, myocardial infarction, stroke, urgent target vessel revascularization (TVR), or major bleeding (defined by Bleeding Academic Research Consortium [BARC] criteria types 2, 3, or 5).
Key Findings and Results
The results of the PARTHENOPE trial indicate a clear advantage for the personalized approach over the traditional 12-month standard.
Primary Endpoint: NACE
At the 24-month follow-up, the primary endpoint of NACE occurred in 18.6% (196 of 1,055) of patients in the personalized DAPT group, compared to 22.2% (232 of 1,052) in the standard DAPT group. This represents an absolute risk reduction of 3.54 percentage points (95% CI: -6.99 to -0.99; P = 0.040). The Number Needed to Treat (NNT) to prevent one NACE was approximately 28, indicating a clinically meaningful benefit.
Ischemic Outcomes
The reduction in NACE was largely attributable to a decrease in ischemic events. Myocardial infarction rates were significantly lower in the personalized group (difference of -2.29 percentage points; 95% CI: -4.43 to -0.14). Similarly, urgent target vessel revascularization was reduced in the personalized group (difference of -1.30 percentage points; 95% CI: -2.55 to -0.05). These data suggest that extending DAPT to 24 months in high-ischemic-risk patients successfully mitigated late thrombotic events without being offset by failures in the short-duration subgroups.
Safety Outcomes: Bleeding
Critically, the personalized approach did not result in an excess of bleeding. The rate of BARC type 2, 3, or 5 bleeding was similar between the two groups (difference of -0.41 percentage points; 95% CI: -2.92 to 2.10). This finding is particularly important because it suggests that shortening DAPT to 3 or 6 months in high-bleeding-risk patients effectively protected them, while the longer 24-month duration in the low-bleeding-risk subgroup did not lead to a prohibitive increase in hemorrhages.
Clinical Implications and Expert Commentary
The PARTHENOPE trial represents a significant step forward in the movement toward precision cardiology. For years, clinicians have utilized risk scores like PRECISE-DAPT or the DAPT score to guide decisions, but prospective randomized data validating a score-based strategy have been limited.
Mechanistic Insights
The superiority of the personalized strategy likely stems from its ability to align the intensity of antithrombotic therapy with the patient’s biological risk profile. In high-ischemic-risk patients, the prolonged 24-month DAPT likely provided protection against ‘non-stent’ related events (e.g., plaque rupture at non-target sites), which are common in polyvascular disease or advanced diabetes. Conversely, in patients where the risk of a life-threatening bleed outweighs the marginal benefit of preventing a small MI, the 3-month duration minimized exposure to harm.
Study Limitations and Considerations
While the results are compelling, some limitations warrant discussion. The trial was an open-label design, which is common in DAPT duration studies but can introduce bias in the reporting of subjective endpoints. Additionally, the specific risk score utilized and the choice of 3, 6, or 24 months as the ‘personalized’ tiers may not be the only viable configurations. Further research is needed to determine if even more granular durations or the use of newer P2Y12 monotherapy strategies would yield even better results.
Impact on Guidelines
Experts suggest that these results will likely influence future iterations of the ESC and ACC/AHA guidelines. The trial provides a ‘proof of concept’ that a structured, score-based approach is superior to a temporal default. It encourages clinicians to perform a formal risk assessment at the time of PCI rather than defaulting to a 12-month prescription.
Conclusion
The PARTHENOPE randomized trial demonstrates that a personalized DAPT duration ranging from 3 to 24 months, tailored to individual patient risk, is superior to a standard 12-month regimen. By reducing the incidence of NACE through lower rates of myocardial infarction and urgent revascularization without increasing bleeding, this strategy offers a more balanced and effective approach to post-PCI care. The era of the ‘standard 12 months’ appears to be giving way to a more nuanced, patient-centric model of care.
Funding and clinicaltrials.gov
The PARTHENOPE trial was supported by various academic and research grants. ClinicalTrials.gov Identifier: NCT04135989.
References
Piccolo R, Calabrò P, Carrara G, et al. Personalized or Standard Duration of Dual Antiplatelet Therapy After Percutaneous Coronary Intervention: The PARTHENOPE Randomized Trial. J Am Coll Cardiol. 2025 Dec 9;86(23):2352-2367. doi: 10.1016/j.jacc.2025.08.040. Epub 2025 Aug 30. PMID: 40892607.