Highlights
Predictive Value of Trial Criteria
Patients with ST-elevation myocardial infarction-related cardiogenic shock (STEMI-CS) who meet the DanGer Shock (DGS) trial eligibility criteria (DGS-like) exhibit significantly lower mortality at 180 days when treated with a microaxial flow pump (mAFP) compared to those who do not (62.5% vs. 72.0%).
Early Survival Benefits
The survival advantage of the DGS-like profile is evident as early as 30 days, with an all-cause mortality rate of 48.4% compared to 70.2% in the DGS-unlike cohort.
Clinical Selection Matters
After multivariable adjustment, the DGS-like profile remained a robust independent predictor of survival, suggesting that the trial’s strict inclusion/exclusion criteria successfully identify a subset of patients most likely to benefit from invasive mechanical circulatory support.
Background: The Evolution of Cardiogenic Shock Management
Cardiogenic shock (CS) remains the leading cause of death in patients hospitalized with acute myocardial infarction, with historical mortality rates hovering around 40% to 50% despite advances in percutaneous coronary intervention (PCI). For decades, the search for effective mechanical circulatory support (MCS) was marked by neutral results in major randomized controlled trials (RCTs), such as the IABP-SHOCK II trial, which led to the downgrading of intra-aortic balloon pumps in international guidelines.
The landscape shifted significantly with the publication of the DanGer Shock (DGS) trial. This landmark study demonstrated that the routine use of a microaxial flow pump (mAFP), specifically the Impella CP, in addition to standard care for STEMI-CS, reduced the risk of all-cause death at 180 days. However, the DGS trial utilized highly specific inclusion and exclusion criteria, focusing on a high-risk but salvageable population while excluding patients with prolonged cardiac arrest or mechanical complications. In clinical practice, clinicians often face an ‘all-comers’ population that is more heterogeneous than trial cohorts. Understanding how well these trial-derived criteria predict outcomes in a real-world setting is crucial for optimizing patient selection and resource allocation.
Study Design and Methodology
To investigate the external validity and predictive power of the DGS criteria, researchers conducted a prospective analysis of a single-centre mAFP registry. The study included 478 patients treated with a microaxial flow pump for cardiogenic shock, of whom 225 presented with STEMI-related CS (STEMI-CS). The primary objective was to compare the outcomes of patients who fit the DGS trial profile (‘DGS-like’) against those who did not (‘DGS-unlike’).
Defining the DGS-like Profile
Patients were categorized as DGS-like if they met the following criteria derived from the original trial:
- Confirmed STEMI-related cardiogenic shock.
- Serum lactate levels ≥2.5 mmol/L.
- Left ventricular ejection fraction (LVEF) < 45%.
- Absence of mechanical complications (e.g., ventricular septal rupture).
- No comatose state following out-of-hospital cardiac arrest (OHCA). However, the study included patients with in-hospital cardiac arrest (IHCA) with a maximum of 10 minutes to return of spontaneous circulation (ROSC) as a surrogate for medically witnessed arrest.
The ‘DGS-unlike’ cohort consisted of STEMI-CS patients who failed to meet one or more of these criteria. The primary endpoint for comparison was all-cause mortality at 180 days, with secondary endpoints including 30-day mortality and procedural characteristics.
Key Findings: Survival Disparities in Real-World Application
Among the 225 patients with STEMI-CS treated with an mAFP, only 64 (28.4%) met the strict DGS-like criteria. This relatively low percentage highlights the high degree of clinical complexity found in real-world registries compared to controlled trial environments.
Baseline Characteristics and Treatment
The DGS-like cohort was generally younger than the DGS-unlike group. Notably, DGS-like patients were significantly less likely to have received cardiopulmonary resuscitation (CPR) prior to mAFP implantation. Furthermore, the duration of mAFP support was significantly longer in the DGS-like group, suggesting a more stable recovery trajectory or a more proactive management strategy in this subset. Interestingly, baseline lactate levels, comorbidities, and the severity of coronary artery disease did not differ significantly between the two groups, nor did the need for inotropes or vasopressors.
Table 1. Baseline characteristics.
| Alln = 225 | DGS‐like STEMI‐CSn = 64 | DGS‐unlike STEMI‐CSn = 161 | P value | |
|---|---|---|---|---|
| Age, years | 69 (58, 82) | 67 (57, 74) | 69 (58, 80) | 0.018 |
| Female sex, n (%) | 55/255 (24.4) | 15/64 (23.4) | 40/161 (24.8) | 0.825 |
| Body mass index, kg/m2 | 26.7 (24.6, 29.4) | 26.7 (24.2, 29.9) | 26.6 (24.7, 29.0) | 0.993 |
| Arterial hypertension, n (%) | 149/221 (67.4) | 45/63 (71.4) | 104/158 (65.8) | 0.422 |
| Atrial fibrillation, n (%) | 49/225 (21.8) | 19/64 (29.7) | 30/161 (18.6) | 0.070 |
| Diabetes mellitus, n (%) | 69/224 (30.8) | 17/64 (26.6) | 52/160 (32.5) | 0.385 |
| CKD stage ≥3, n (%) | 58/223 (26.0) | 16/64 (25.0) | 42/159 (26.4) | 0.828 |
| PAD, n (%) | 18/224 (8.0) | 4/64 (6.3) | 14/160 (8.8) | 0.534 |
| COPD, n (%) | 10/224 (4.5) | 2/64 (3.1) | 8/160 (5.0) | 0.728 |
| Dyslipidaemia, n (%) | 125/220 (56.8) | 41/64 (64.1) | 84/156 (53.8) | 0.165 |
| Previous AMI, n (%) | 39/225 (17.3) | 8/64 (12.5) | 31/161 (19.3) | 0.227 |
| Previous CABG, n (%) | 8/225 (3.6) | 3/64 (4.7) | 5/161 (3.1) | 0.691 |
| Previous PCI, n (%) | 45/225 (20.0) | 8/64 (12.5) | 37/161 (23.0) | 0.076 |
| Previous stroke, n (%) | 22/225 (9.8) | 7/64 (10.9) | 15/161 (9.3) | 0.712 |
| Mean blood pressure, mmHg | 74 (60, 89) | 74 (66, 84) | 73 (60, 90) | 0.642 |
| Heart rate, min−1 | 95 (75, 115) | 100 (80, 116) | 92 (74, 110) | 0.122 |
| Arterial lactate, mmol/L | 5.6 (3.2, 11.6) | 4.9 (3.7, 8.8) | 6.3 (2.7, 12.0) | 0.496 |
| Arterial lactate ≥2.5 mmol/L, n (%) | 180/217 (82.9) | 64/64 (100) | 116/153 (75.8) | <0.001 |
| LVEF, % | 30 (20, 40) | 30 (20, 40) | 25 (20, 40) | 0.104 |
| Resuscitation before mAFP, n (%) | 122/225 (54.2) | 21/64 (32.8) | 101/161 (62.7) | <0.001 |
| Median time of CPR, min | 20 (10, 53) | 7 (5,10) | 30 (15, 60) | <0.001 |
| Coronary artery disease, n (%) | 0.866 | |||
| None | 1/223 (0.4) | 0/64 (0) | 1/159 (0.6) | |
| 1‐vessel | 49/223 (22.0) | 13/64 (20.3) | 36/159 (22.6) | |
| 2‐vessel | 65/223 (29.1) | 18/64 (28.1) | 47/159 (29.6) | |
| 3‐vessel | 108/223 (48.4) | 33/64 (51.6) | 75/159 (47.2) | |
| Infarct‐related artery LM or LAD, n (%) | 137/219 (62.6) | 41/64 (65.1) | 96/156 (61.5) | 0.624 |
| PCI treatment, n (%) | 217/225 (96.4) | 64/64 (100) | 153/161 (95.0) | 0.109 |
| Median time from symptoms to mAFP, hours | 2 (1.0, 3.8) | 2 (1.0, 4.4) | 2 (1.0, 3.5) | 0.864 |
| Duration of mAFP support, hours | 34.5 (8.0, 72.9) | 46.2 (19.9, 96.9) | 26.7 (4.3, 69.3) | 0.019 |
| Type of mAFP, n (%) | 0.580 | |||
| Impella CP | 221/225 (98.2) | 64/64 (100) | 0/64 (0) | |
| Impella 2.5 | 4/225 (1.8) | 0/64 (0) | 4/161 (2.5) | |
| Additional tMCS, n (%) | 0.571 | |||
| Impella RP | 4/225 (1.8) | 0/64 (0) | 4/161 (2.5) | |
| V‐A ECMO | 10/225 (4.4) | 4/64 (6.3) | 6/161 (3.7) | |
| Ventilation, n (%) | 0.084 | |||
| None | 22/225 (9.8) | 10/64 (15.6) | 12/161 (7.5) | |
| Non‐invasive | 14/225 (6.2) | 4/64 (6.3) | 10/161 (6.2) | |
| Invasive | 146/225 (64.9) | 34/64 (53.1) | 112/161 (69.6) | |
| Both | 43/225 (19.1) | 16/64 (25.0) | 27/161 (16.8) | |
| Any norepinephrine, n (%) | 193/223 (86.5) | 51/63 (81.0) | 142/160 (88.8) | 0.124 |
| Any vasopressin, n (%) | 81/222 (36.5) | 19/63 (30.2) | 62/159 (39.0) | 0.218 |
| Any dobutamine, n (%) | 118/222 (53.2) | 28/63 (44.4) | 90/159 (56.6) | 0.102 |
| Any enoximone, n (%) | 31/222 (14.0) | 11/63 (17.5) | 20/159 (12.6) | 0.344 |
Mortality Outcomes
The study found a striking difference in survival outcomes. The 180-day all-cause mortality was 62.5% in the DGS-like cohort compared to 72.0% in the DGS-unlike cohort (P = 0.014). The difference was even more pronounced at the 30-day mark, where mortality was 48.4% for DGS-like patients versus 70.2% for DGS-unlike patients (P < 0.001).


Multivariable Analysis
To ensure these findings were not merely the result of confounding variables such as age or CPR history, the researchers performed a multivariable analysis. The DGS-like profile remained a potent independent predictor of reduced mortality at both 180 days (Hazard Ratio [HR] 0.57; 95% CI 0.39, 0.83) and 30 days (HR 0.48; 95% CI 0.32, 0.72). These data suggest that the specific constellation of clinical factors used in the DGS trial identifies a phenotype with a markedly better prognosis when supported by microaxial flow pumps.
Table. Primary and secondary outcomes.
| Alln = 225 | DGS‐like STEMI‐CSN = 64 | DGS‐unlike STEMI‐CSN = 161 | Adjusted coefficients (95%CI) | P value | |
|---|---|---|---|---|---|
| Death at 180 days, n (%) | 156/225 (69.3) | 40/64 (62.5) | 116/161 (72.0) | 0.57 (0.39, 0.83) a | 0.014 (log‐rank) |
| Death at 30 days, n (%) | 144/225 (64.0) | 31/64 (48.4) | 113/161 (70.2) | 0.48 (0.32, 0.72) a | <0.001 (log‐rank) |
| CPR after device, n (%) | 119/219 (54.3) | 24/63 (38.1) | 95/161 (60.9) | 0.50 (0.27, 0.95) b | 0.002 |
| Death on device, n (%) | 100/225 (44.4) | 20/64 (31.3) | 80/161 (49.7) | 0.36 (0.19, 0.69) b | 0.012 |
| Weaning success, n (%) | 104/225 (46.2) | 36/64 (56.3) | 68/161 (42.2) | 1.45 (0.68, 3.10) b | 0.057 |
| Days in ICU, days | 5 (1, 15)n = 220 | 6 (3, 16)n = 62 | 4 (1, 15)n = 158 | 0.04 (−2.75, 4.74) c | 0.057 |
Expert Commentary: Interpreting the Data
The results of this registry analysis provide critical insights into the ‘whom to treat’ dilemma in cardiogenic shock. While the DanGer Shock trial proved that mAFPs can save lives, this study by Mangner et al. emphasizes that the benefit is heavily dependent on the patient profile. The significantly higher mortality in the DGS-unlike group (over 70% at 30 days) suggests that in patients with prolonged cardiac arrest, lower lactate levels (possibly indicating less severe shock), or mechanical complications, the use of an mAFP may not be enough to overcome the underlying severity of the insult.
The Challenge of Cardiac Arrest
One of the most important takeaways involves the exclusion of comatose OHCA patients. In the DGS-unlike cohort, many patients were excluded because of prolonged CPR or neurological uncertainty. The poor outcomes in this group reinforce the theory that ‘brain death’ or irreversible systemic inflammatory response syndrome (SIRS) often precedes cardiac recovery in these cases. By selecting patients with shorter ROSC times or witnessed arrests, clinicians can target individuals where hemodynamic support can actually bridge the patient to recovery rather than merely prolonging a futile situation.
Mechanistic Insights
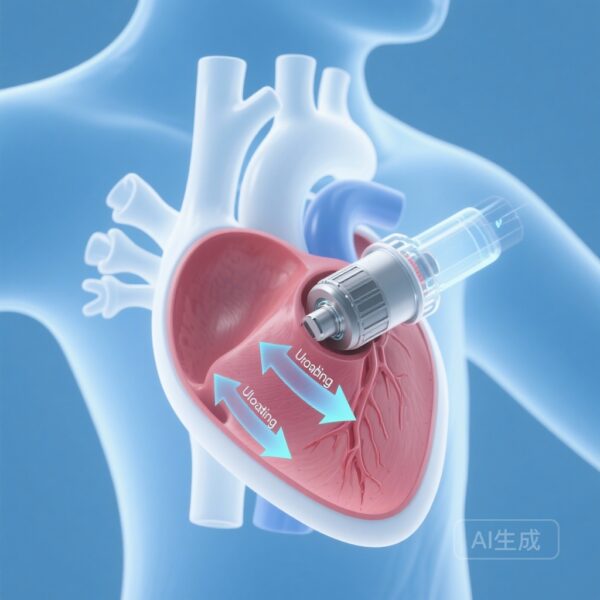
The microaxial flow pump works by actively unloading the left ventricle and increasing systemic mean arterial pressure, thereby reducing myocardial oxygen demand while improving coronary and end-organ perfusion. The DGS-like profile essentially selects for patients with profound ‘pump failure’ (low LVEF, high lactate) who still have a viable chance of neurological and systemic recovery. In contrast, the DGS-unlike group may include patients who are either ‘too well’ (lactate < 2.5) to justify the risks of an invasive device or ‘too sick’ (prolonged arrest) to benefit from hemodynamic stabilization.
Conclusion: Moving Toward Precision MCS
The findings from this registry analysis validate the rigor of the DanGer Shock trial’s design and offer a practical framework for real-world application. By identifying a DGS-like profile, clinicians can more accurately predict which STEMI-CS patients are likely to derive a survival benefit from mAFP therapy. While the overall mortality in cardiogenic shock remains high, the ability to identify a subset with a 20% absolute reduction in 30-day mortality compared to the ‘unlike’ cohort represents a significant step forward in precision critical care.
Future research should focus on whether specific interventions can improve outcomes for the ‘DGS-unlike’ population, or whether alternative strategies—such as earlier escalation to extracorporeal membrane oxygenation (ECMO) or palliative care—are more appropriate for those who do not meet these criteria.
References
1. Mangner N, Mierke J, Baron D, et al. DanGer Shock-like profile predicts the outcome in ST-elevation myocardial infarction-related cardiogenic shock. ESC Heart Fail. 2025;12(4):2759-2768. doi:10.1002/ehf2.15269 IF: 3.7 Q1 .
2. Møller JE, Engstrøm T, Jensen LO, et al. Microaxial Flow Pump or Standard Care in Infarct-Related Cardiogenic Shock. N Engl J Med. 2024;390(15):1389-1400.
3. Thiele H, Zeymer U, Neumann FJ, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med. 2012;367(14):1287-1296.