Introduction: The Persistent Challenge of Residual Risk
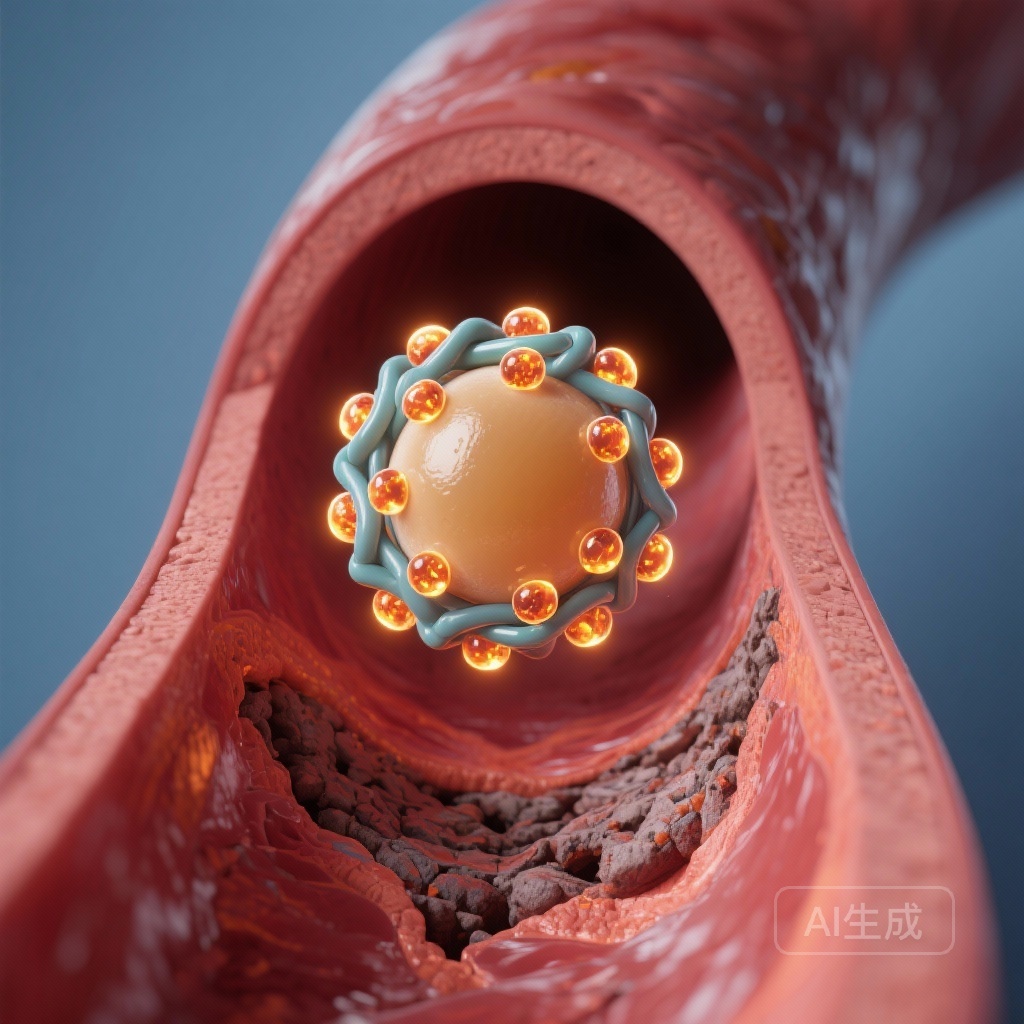
Despite the successful implementation of intensive LDL-cholesterol lowering and antiplatelet therapies, a substantial residual risk for major adverse cardiovascular events (MACE) remains in patients with established coronary artery disease (CAD). Recent scientific focus has shifted toward Lipoprotein(a) [Lp(a)] and its proinflammatory cargo, specifically oxidized phospholipids (OxPL). While Lp(a) is recognized as a genetically determined, independent risk factor for CAD, the precise mechanisms by which it exerts its deleterious effects—whether through pro-atherogenic, pro-inflammatory, or pro-thrombotic pathways—remain a subject of intense clinical investigation.
Oxidized phospholipids on apolipoprotein B-100 (OxPL-apoB) represent a key biomarker of the pro-inflammatory potential of the apoB-containing lipoproteins, with the majority of OxPL being carried on Lp(a). Experimental models have previously suggested that OxPL might enhance platelet activation and contribute to a hypercoagulable state. However, clinical evidence linking OxPL-apoB levels to actual platelet reactivity in patients undergoing coronary interventions has been sparse. This article interprets the findings of a major study utilizing data from the EXCELSIOR trial to clarify these relationships.
Highlighting the Core Findings
1. Decoupling OxPL-apoB from Platelet Activation
Contrary to some experimental hypotheses, the study found no significant association between OxPL-apoB levels and either intrinsic or on-clopidogrel platelet reactivity. This suggests that the cardiovascular risk conferred by OxPL-apoB is not primarily mediated through the ADP or collagen-induced platelet activation pathways.
2. Long-Term Prognostic Value
Both OxPL-apoB and Lp(a) were confirmed as significant independent predictors of myocardial infarction-free survival and all-cause mortality over a median follow-up of seven years. Patients with OxPL-apoB levels above 8 nmol/L faced a 39% higher risk of adverse outcomes.
3. The Synergy of OxPL and Lp(a)
When analyzed together in multivariable models, the independent significance of each marker was attenuated, reinforcing the biological reality that OxPL-apoB and Lp(a) are inextricably linked, with OxPL likely serving as the primary driver of Lp(a)-associated vascular injury.
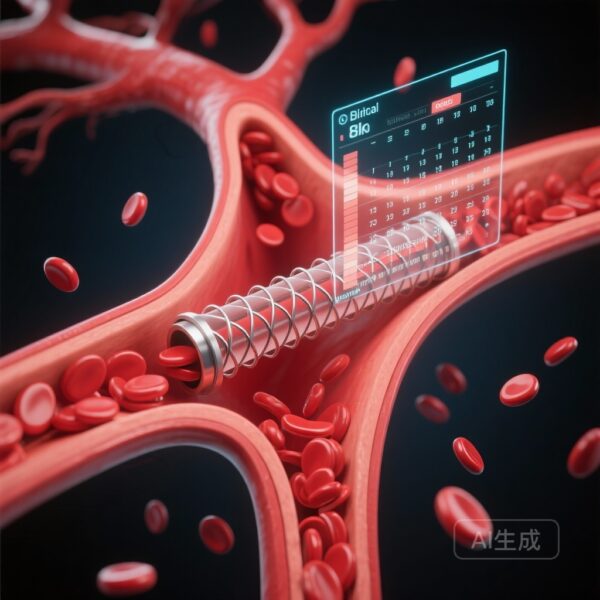
Study Design and Methodology
The research utilized a robust observational cohort from the EXCELSIOR trial (Impact of Extent of Clopidogrel-Induced Platelet Inhibition During Elective Stent Implantation on Clinical Event Rate). The study population included 2,040 patients undergoing coronary angiography, with or without percutaneous coronary intervention (PCI). This provided a high-risk clinical setting to evaluate both acute platelet dynamics and long-term outcomes.
Researchers measured OxPL-apoB levels and Lp(a) concentrations at baseline. Platelet function was rigorously assessed using multiple parameters: the expression of surface markers such as CD62P (P-selectin), CD41, and PAC-1 (activated GPIIb/IIIa receptor), and platelet aggregation responses to collagen and ADP, both intrinsically and under the influence of the P2Y12 inhibitor clopidogrel. The primary clinical endpoint was myocardial infarction-free survival and all-cause mortality over a 7-year horizon.
Detailed Analysis of Results
Clinical Characteristics and Correlation with CAD Severity
Elevated OxPL-apoB levels were not merely biochemical markers but correlated strongly with the clinical burden of disease. Higher levels were observed in patients with more severe coronary obstruction and those with a history of prior myocardial infarction, PCI, or coronary artery bypass graft (CABG) surgery. This aligns with the understanding of OxPL as a marker of cumulative atherosclerotic burden.
Platelet Reactivity: The Negative Finding
One of the most significant aspects of this study was the lack of correlation between OxPL-apoB and platelet function. Whether assessing the baseline activation state (PAC-1 or CD62P expression) or the response to agonists (ADP and collagen), OxPL-apoB levels did not differentiate high-reactivity patients from low-reactivity patients. Furthermore, OxPL-apoB did not influence the efficacy of clopidogrel-induced platelet inhibition. This finding is crucial as it suggests that the “pro-thrombotic” reputation of Lp(a) might not be driven by classical platelet aggregation pathways but perhaps by other mechanisms like impaired fibrinolysis or localized plaque instability.
Predicting Long-Term Outcomes
In univariate and separate multivariable Cox regression models, the data was clear:
– OxPL-apoB: Hazard Ratio (HR) 1.022 per unit increase (P=0.010).
– Lp(a): HR 1.002 per unit increase (P=0.032).
The researchers identified optimal cut-off points for clinical risk stratification. For OxPL-apoB, a threshold of 8 nmol/L was associated with an HR of 1.391 (95% CI, 1.086-1.780; P=0.009). For Lp(a), the traditional threshold of 30 mg/dL yielded an HR of 1.261 (95% CI, 1.012-1.570; P=0.038). However, when both OxPL-apoB and Lp(a) were included in the same multivariable model, neither remained a statistically significant independent predictor. This statistical “washout” occurs due to the high collinearity between the two—because OxPL is primarily carried on Lp(a), they essentially represent the same pathological axis.
Expert Commentary: Mechanistic Insights and Clinical Implications
From a physiological standpoint, these findings suggest that the clinical risk associated with Lp(a) and its oxidized phospholipid content is predominantly driven by chronic atherogenesis and perhaps late-stage plaque vulnerability rather than acute platelet-mediated thrombosis.
OxPL are known to be sequestered within the arterial wall, where they promote the recruitment of monocytes, induce the death of vascular smooth muscle cells, and contribute to the formation of a necrotic core. The fact that circulating OxPL-apoB levels do not correlate with systemic platelet reactivity suggests that their role in “thrombosis” might be confined to the local environment of a ruptured plaque—where OxPL could potentially interact with the coagulation cascade or local inflammatory cells—rather than causing a systemic “hyper-reactive” platelet phenotype.
For the clinician, this study reinforces the importance of measuring Lp(a) or OxPL-apoB as part of a comprehensive risk assessment. While we currently lack widely available therapies specifically targeting OxPL, the emergence of antisense oligonucleotides and siRNA therapies designed to lower Lp(a) (such as pelacarsen and olpasiran) offers a promising future. By lowering Lp(a), these therapies will inherently reduce the burden of OxPL-apoB, potentially addressing the residual risk identified in the EXCELSIOR cohort.
Conclusion
The analysis of the EXCELSIOR trial confirms that OxPL-apoB and Lp(a) are potent longitudinal predictors of cardiovascular mortality and myocardial infarction. Importantly, the study clarifies that this risk does not stem from increased platelet reactivity or resistance to P2Y12 inhibition. Instead, the accumulation of OxPL on the Lp(a) moiety likely promotes cardiovascular events through progressive atheroinflammation. As we move toward an era of personalized lipid management, identifying patients with elevated OxPL-apoB remains a critical step in identifying those who may benefit most from aggressive secondary prevention and future Lp(a)-targeted therapies.
Funding and Registration
The EXCELSIOR trial was supported by institutional funding and specific grants related to cardiovascular research. ClinicalTrials.gov Identifier: NCT00457236.
Reference:
Tsimikas S, Kille A, Kaier K, Nührenberg T, Franke K, Valina CM, Yang X, Leibundgut G, Neumann FJ, Westermann D, Hochholzer W. Oxidized Phospholipids on ApoB-100, Platelet Activation and Reactivity, and Long-Term Cardiovascular Outcomes. Arterioscler Thromb Vasc Biol. 2025 Oct;45(10):1935-1944. doi: 10.1161/ATVBAHA.125.322347 . Epub 2025 Aug 14. PMID: 40808656 ; PMCID: PMC12421647 .