Highlights
– The CALIPSO randomized clinical trial showed OCT-guided PCI produced a larger final minimal stent area (MSA) than angiography-guided PCI in patients with moderate-to-severe coronary calcification (median MSA 6.5 mm2 vs 5.0 mm2; P <.001).
– OCT guidance prompted more frequent use of intravascular lithotripsy (IVL) and algorithm-driven lesion preparation (46% vs 12%), suggesting enhanced lesion characterization led to more appropriate plaque modification.
– No increase in periprocedural myocardial infarction, radiation dose, contrast volume, or procedure duration was observed with OCT guidance, but the trial was not powered for long-term clinical outcomes.
Background
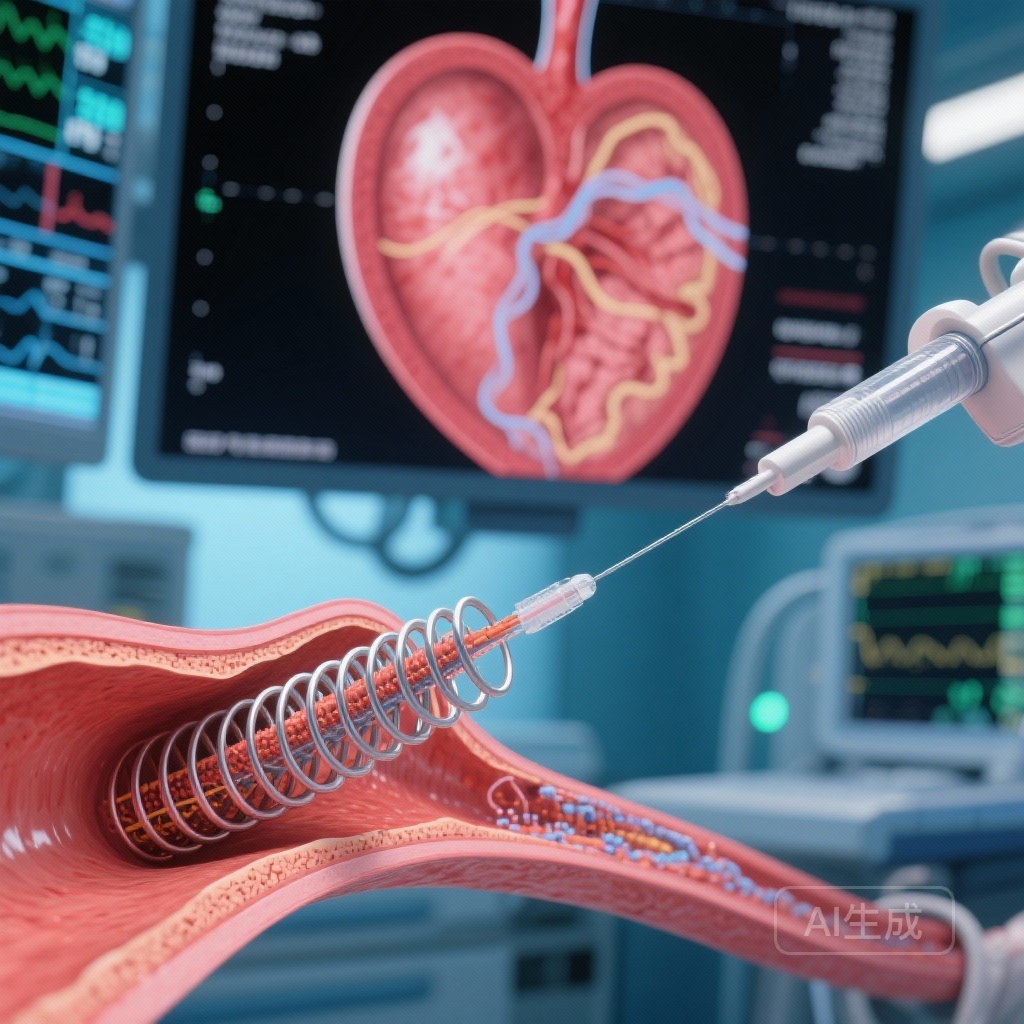
Coronary artery calcification is increasingly common in aging populations and complicates percutaneous coronary intervention (PCI) by promoting stent underexpansion, malapposition, and impaired drug delivery. Poor stent expansion is strongly associated with higher rates of restenosis and stent thrombosis. Angiography alone frequently underestimates the extent, depth, and circumferential distribution of calcium. Intravascular imaging—principally intravascular ultrasound (IVUS) and optical coherence tomography (OCT)—provides direct visualization and quantification of calcified plaque and can guide lesion preparation and device selection.
OCT offers higher axial resolution than IVUS and can detect superficial calcium arcs and thickness, features that may influence decisions about atherectomy, scoring balloons, or intravascular lithotripsy (IVL). Despite guideline interest and observational data suggesting benefits of intravascular imaging for complex PCI, randomized data specifically evaluating OCT-guided strategies for calcified lesions have been lacking.
Study design
CALIPSO (Calcified Lesion Intervention Planning Steered by OCT) was a prospective, multicenter, open-label randomized clinical trial conducted at 12 sites in France between December 2021 and June 2023. Patients with stable coronary disease and angiographically identified moderate-to-severe calcified lesions scheduled for PCI were eligible. After diagnostic angiography, patients were randomized 1:1 to OCT-guided PCI or angiography-guided PCI. The OCT arm used predefined, standardized management algorithms based on OCT measurements to guide lesion preparation and device selection.
Importantly, both arms underwent post-PCI OCT imaging for objective measurement of the primary end point: minimal stent area (MSA) as assessed by OCT. Key secondary safety end points included periprocedural myocardial infarction, radiation dose, contrast medium volume, and total procedure duration. Trial registration: NCT05301218.
Key findings
Population and flow: 143 patients were randomized; 134 patients were included in the final analysis (65 in the OCT-guided arm and 69 in the angiography-guided arm). Median patient age was 73.0 years (IQR 66.0–78.0), and 18.7% were female. Baseline clinical characteristics were balanced between arms.
Primary end point
The final post-PCI median MSA measured by OCT was significantly larger in the OCT-guided group compared with the angiography-guided group: 6.5 mm2 (IQR 5.5–8.1) versus 5.0 mm2 (IQR 4.1–6.1), P <.001. This represented a clinically meaningful improvement in stent expansion for calcified lesions when management was directed by OCT-derived lesion assessment and a prespecified algorithm.
Procedural strategies and mechanisms
Procedural behaviors differed between arms. Use of intravascular lithotripsy was substantially more frequent in the OCT-guided arm (30 patients, 46%) than in the angiography-guided arm (8 patients, 12%), P <.001. This likely reflects OCT’s ability to reveal calcium arc, thickness, and focal distribution that prompts operators to select IVL or other plaque-modification tools. The algorithmic approach in the OCT arm standardized responses to imaging features (for example, selection of IVL for concentric or thick calcium), whereas angiography-based decisions may underrecognize such patterns.
Safety and secondary outcomes
There were no significant differences between groups in short-term procedural safety measures: periprocedural myocardial infarction rates were similar, and there were no increases in radiation exposure, contrast volume, or overall procedure duration in the OCT arm. The trial was designed primarily to detect differences in the imaging-derived MSA and was not powered to detect differences in long-term clinical events such as target lesion failure, myocardial infarction beyond the periprocedural period, or mortality.
Interpretation of effect size
MSA is an established surrogate for stent optimization. Larger MSA after PCI correlates with lower rates of restenosis and adverse events in observational series and some randomized studies of imaging-guided stent optimization. The absolute difference observed (median ~1.5 mm2) is meaningful in the context of calcified lesions, where even modest increases in expansion can translate to improved luminal gain and potentially fewer ischemic complications. However, translating improved MSA into proven reductions in hard clinical events requires adequately powered, longer-term outcome trials.
Expert commentary and contextualization
The CALIPSO trial delivers pragmatic randomized evidence that OCT-guided, algorithm-driven management of calcified coronary lesions improves immediate stent expansion compared with angiography-guided PCI. Several mechanistic points are notable: first, OCT provides high-resolution insights into calcium distribution, which appears to change operator behavior—specifically, more frequent and targeted use of IVL. Second, standardized algorithms reduce variability in decision-making and may amplify the benefit of imaging by ensuring consistent responses to imaging findings.
Strengths of the trial include multicenter randomized design, objective imaging-based primary end point assessed in both arms, and predefined algorithms. Limitations include the open-label design (operator awareness of allocation can influence decisions), the surrogate nature of the primary outcome (MSA rather than clinical events), modest sample size, and a study population limited to centers with OCT experience. The higher rate of IVL use in the OCT arm introduces a mechanistic mediator: improved MSA may reflect better lesion preparation driven by imaging rather than imaging per se. Whether routine OCT should be adopted universally will depend on cost-effectiveness, operator experience, device availability, and evidence of improved patient-level outcomes in larger trials.
Current international practice guidelines already encourage intravascular imaging to optimize stent implantation in selected complex lesions and to guide decision-making in cases of stent failure. The CALIPSO results reinforce guideline rationale by demonstrating an immediate mechanical advantage in the specific and high-risk setting of coronary calcification.
Clinical implications and practical takeaways
- OCT-guided PCI with predefined lesion-preparation algorithms increased final MSA in calcified lesions without adding procedural risk, suggesting imaging-based planning may improve technical success.
- OCT frequently identified calcific features that led operators to escalate plaque modification (notably, IVL), indicating the benefit is mediated through targeted therapy.
- Institutions considering routine OCT for calcified lesions should ensure access to a range of plaque-modification tools (scoring balloons, rotational/orbital atherectomy, IVL) and operator training in image interpretation and algorithmic decision-making.
- Before broad adoption, larger trials with clinical end points, cost-effectiveness analyses, and follow-up beyond the index procedure are desirable to confirm that improved MSA translates into fewer adverse clinical events.
Conclusion
In patients undergoing PCI for moderate-to-severe coronary calcification, OCT-guided, algorithmic lesion assessment and preparation produced greater stent expansion than angiography-guided PCI in the CALIPSO randomized trial, driven in part by more appropriate use of intravascular lithotripsy. The approach did not increase short-term procedural risk but was evaluated using a surrogate imaging endpoint. These results support the value of intravascular imaging for optimizing mechanical outcomes in calcified lesions and motivate larger outcome trials to determine whether imaging-driven strategies improve long-term clinical outcomes and are cost-effective in routine practice.
Funding and trial registration
Trial registration: ClinicalTrials.gov Identifier NCT05301218. Funding and detailed disclosures are reported in the primary publication: Amabile N, Rangé G, Landolff Q, et al. JAMA Cardiol. 2025;10(7):666-675.
References
1. Amabile N, Rangé G, Landolff Q, et al. OCT vs Angiography for Guidance of Percutaneous Coronary Intervention of Calcified Lesions: The CALIPSO Randomized Clinical Trial. JAMA Cardiol. 2025 Jul 1;10(7):666-675. doi: 10.1001/jamacardio.2025.0741. PMID: 40305015; PMCID: PMC12044539.
2. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87-165. (Guideline document discussing role of intravascular imaging in complex PCI.)
AI thumbnail prompt (for image generation)
A clinical cardiac catheterization lab scene: close-up of an OCT cross-sectional coronary image displayed on a high-resolution monitor showing crescentic calcium and stent struts; in the foreground a cardiologist reviews the image with a colleague beside an angiography monitor; cool clinical lighting, realistic medical devices, professional and focused mood.