Introduction: Addressing the Progressive Challenge of MacTel Type 2
Macular telangiectasia type 2 (MacTel) is a progressive, bilateral neurodegenerative disease of the central retina that typically manifests in middle age. Characterized by the loss of Müller cells and subsequent degeneration of photoreceptors, MacTel leads to significant visual impairment, particularly affecting reading and fine-detail tasks. Unlike many other retinal diseases, MacTel does not primarily stem from vascular leakage or neovascularization in its early stages, making traditional anti-VEGF therapies largely ineffective for the non-proliferative form of the disease.
The quest for a neuroprotective agent that can stabilize the retina and prevent the loss of photoreceptors has led to the development of NT-501 (Revakinagene taroretcel). This innovative therapy utilizes encapsulated cell technology to provide a continuous, intraocular supply of ciliary neurotrophic factor (CNTF). Following promising results in Phase 2 clinical trials, two identical Phase 3 trials—NTMT-03-A and NTMT-03-B—were conducted to evaluate the efficacy and safety of NT-501 in slowing the progression of MacTel.
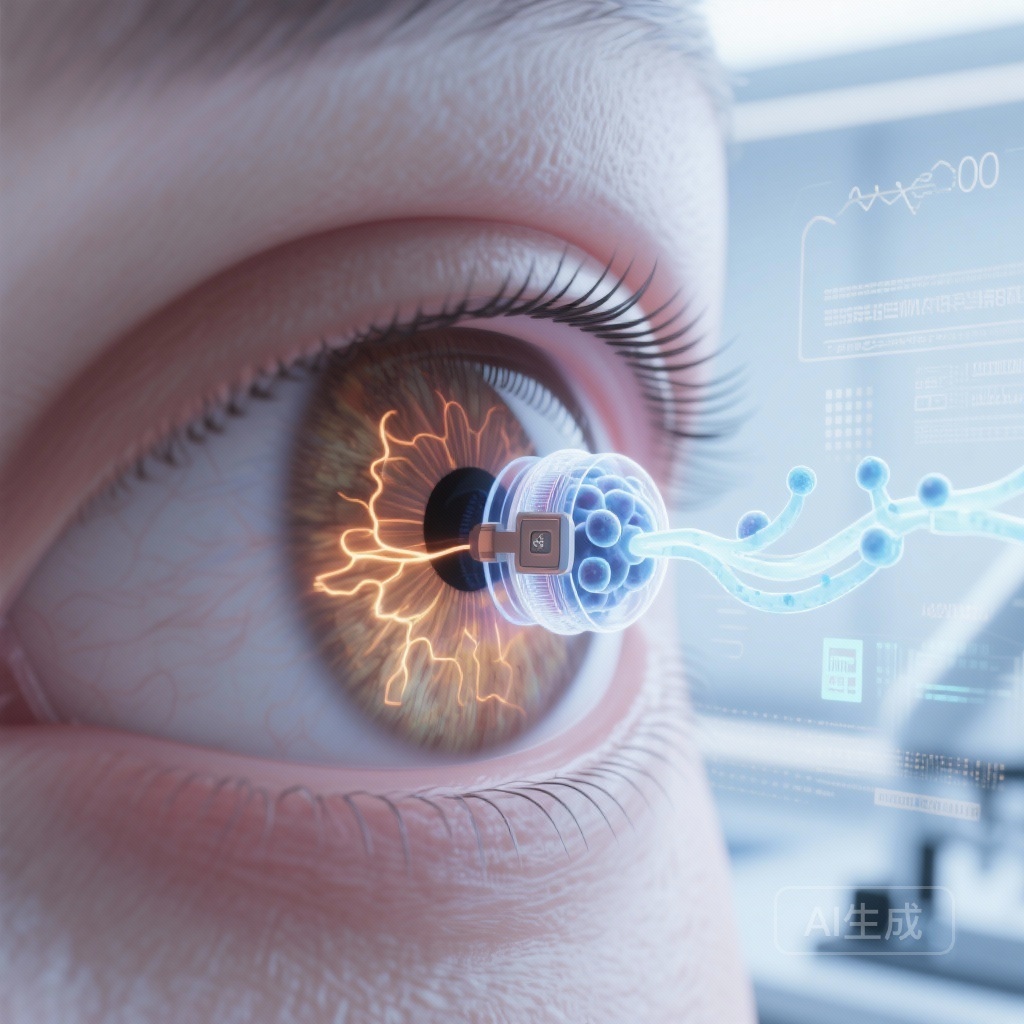
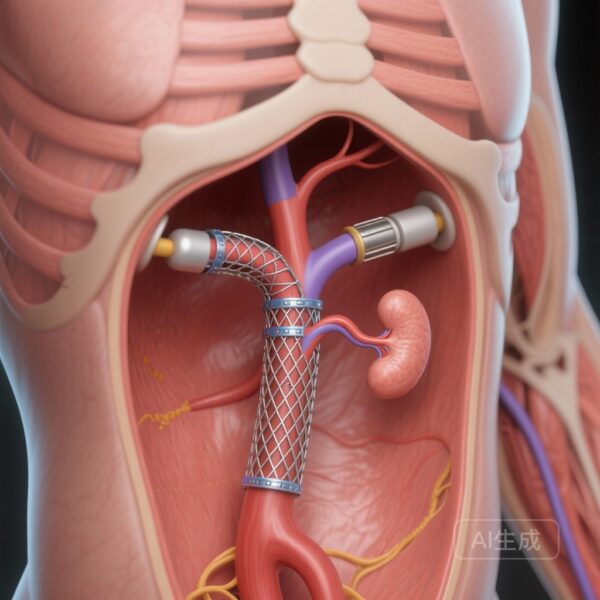
The Mechanism: Encapsulated Cell Therapy and CNTF
NT-501 represents a paradigm shift in ocular drug delivery. It consists of a semi-permeable polymer capsule containing human cells (NTC-200 cell line) genetically engineered to secrete CNTF. This device is surgically implanted into the vitreous cavity. The capsule’s membrane allows nutrients to enter and CNTF to exit, while shielding the producer cells from the host’s immune system. This ensures a long-term, sustained release of the therapeutic protein directly to the site of degeneration.
CNTF is a potent neurotrophic factor known for its ability to promote the survival of various neuronal populations, including photoreceptors. In the context of MacTel, CNTF is hypothesized to protect the remaining retinal cells from metabolic stress and apoptosis, thereby slowing the expansion of the ellipsoid zone (EZ) area loss—a key structural biomarker for photoreceptor integrity in this disease.
Study Design: The NTMT-03 Phase 3 Program
The NTMT-03 program comprised two multicenter, randomized, sham-controlled Phase 3 trials. A total of 115 participants were enrolled in NTMT-03-A and 113 in NTMT-03-B. Participants were randomized to receive either the NT-501 implant or a sham procedure. To ensure rigorous evaluation, the trials utilized high-resolution spectral-domain optical coherence tomography (SD-OCT) to measure the primary endpoint.
Primary and Secondary Endpoints
The primary efficacy endpoint was the rate of change in ellipsoid zone area (EZA) loss over a 24-month period, measured in square millimeters (mm2). Secondary outcomes focused on functional metrics, including changes in retinal sensitivity (measured via microperimetry), reading speed, and patient-reported outcomes using the National Eye Institute Visual Function Questionnaire 25 (NEI VFQ-25).
Safety monitoring was extensive, tracking treatment-emergent serious adverse events (SAEs), changes in best-corrected visual acuity (BCVA), and specific physiological responses to CNTF, such as miosis (pupillary constriction) and delayed dark adaptation.
Key Findings: Significant Deceleration of Photoreceptor Loss
The results from both Phase 3 trials demonstrated a statistically significant reduction in the rate of EZA loss in eyes treated with NT-501 compared to those receiving the sham procedure.
Structural Efficacy
In NTMT-03-A, the adjusted rate of change of EZA loss was 0.075 mm2/24 months in the NT-501 group versus 0.166 mm2/24 months in the sham group. This represents a difference of -0.091 mm2/24 months (95% CI, -0.125 to -0.056; P<0.001), indicating a substantial slowing of retinal degeneration.
The NTMT-03-B trial mirrored these findings, albeit with a slightly different magnitude. The rate of EZA loss was 0.111 mm2/24 months for the NT-501 group and 0.160 mm2/24 months for the sham group, resulting in a difference of -0.049 mm2/24 months (95% CI, -0.089 to -0.008; P=0.02). The consistency across two independent trials reinforces the structural neuroprotective effect of the therapy.
Functional Outcomes
Despite the clear structural benefits, the functional outcomes were less definitive. Changes in retinal sensitivity and reading speed were inconsistent between the two trials. Furthermore, no significant differences were observed between treatment groups in NEI VFQ-25 scores or BCVA loss. This discrepancy suggests that while NT-501 preserves the physical integrity of the photoreceptors, the translation of this structural preservation into measurable functional improvements may require longer observation periods or more sensitive functional assessments.
Safety and Tolerability
The safety profile of NT-501 was generally favorable, with no significant differences in the proportion of participants experiencing serious adverse events compared to the sham group. However, specific physiological effects related to CNTF exposure were noted.
Miosis and Dark Adaptation
Miosis was observed in 17% and 14% of the NT-501 groups in NTMT-03-A and NTMT-03-B, respectively, compared to none in the sham groups. Similarly, delayed dark adaptation occurred in 17% and 24% of the NT-501 groups. These are known pharmacological effects of CNTF on the iris dilator muscle and the visual cycle, respectively. While these effects are manageable, they represent important clinical considerations for patients undergoing treatment.
Expert Commentary and Clinical Implications
The success of the NTMT-03 trials marks a milestone in the management of MacTel Type 2. For years, clinicians have lacked an intervention that targets the underlying neurodegenerative process. The ability of NT-501 to reduce the rate of EZA loss by approximately 30% to 50% offers hope for preserving long-term visual function in patients who would otherwise face steady decline.
The inconsistency in functional metrics highlights a common challenge in neuroprotection trials: structural changes often precede functional decline, and current functional tests may not be sensitive enough to capture the benefits of slowing a slowly progressive disease over a 24-month window. However, in the ophthalmological community, EZA loss is increasingly accepted as a robust surrogate marker for disease progression in MacTel.
Future research should focus on the long-term sustainability of the NT-501 implant and whether repeated implantations are necessary or safe. Additionally, investigating the treatment’s efficacy in different stages of the disease may help refine patient selection criteria.
Conclusion
In conclusion, the Phase 3 trials NTMT-03-A and NTMT-03-B provide high-level evidence that NT-501 encapsulated cell therapy is effective in slowing the progression of retinal degeneration in Macular Telangiectasia Type 2. By significantly reducing the rate of ellipsoid zone area loss, this therapy addresses a critical unmet need in ocular neuroprotection. While functional benefits were not uniformly demonstrated within the 24-month study period, the structural preservation achieved suggests that NT-501 could significantly alter the clinical trajectory of MacTel Type 2.
Funding and Clinical Trial Information
These studies were funded by Neurotech Pharmaceuticals. ClinicalTrials.gov identifiers: NCT03316300 (NTMT-03-A) and NCT03319849 (NTMT-03-B).
References
Chew EY, Gillies M, Jaffe GJ, et al. Cell-Based Ciliary Neurotrophic Factor Therapy for Macular Telangiectasia Type 2. NEJM Evid. 2025 Aug;4(8):EVIDoa2400481. doi: 10.1056/EVIDoa2400481. Epub 2025 Jul 22. PMID: 40693847.