Introduction: The Unmet Need in NAION Management
Nonarteritic anterior ischemic optic neuropathy (NAION) represents the most common cause of acute optic nerve dysfunction in adults over the age of 50. Often described as a “stroke of the optic nerve,” NAION typically presents as sudden, painless unilateral vision loss, often discovered upon awakening. Despite its prevalence and the significant morbidity associated with it, the ophthalmic community has struggled for decades to identify a proven, evidence-based therapy. Current management typically focuses on addressing underlying cardiovascular risk factors, but no pharmacological intervention has successfully demonstrated the ability to restore or reliably preserve vision in the acute phase.
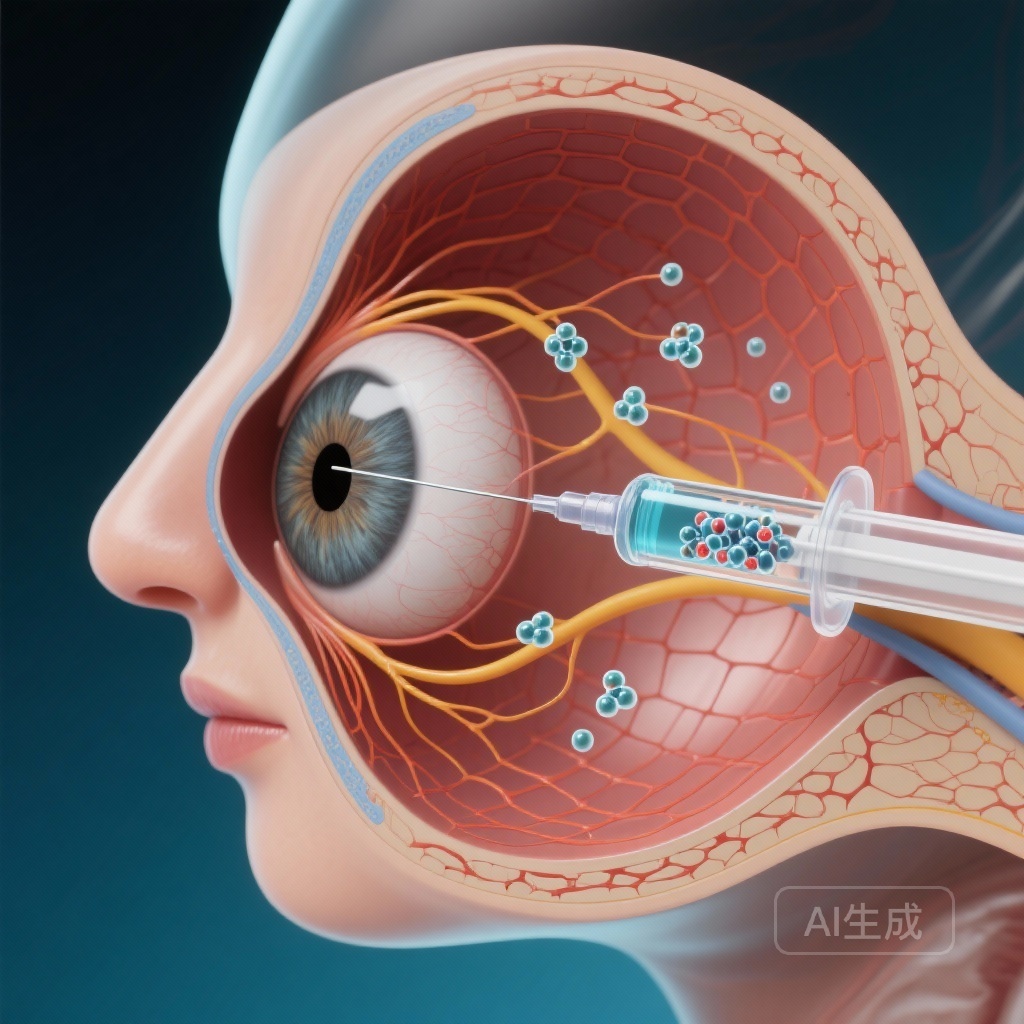
The pathophysiology of NAION involves an ischemic insult to the optic nerve head, leading to a cascade of axonal swelling and subsequent retinal ganglion cell (RGC) death. Research has identified caspase 2, a pro-apoptotic protease, as a key mediator in the death of RGCs following axonal injury. QPI-1007, a synthetic, chemically modified small interfering RNA (siRNA), was designed to inhibit the expression of caspase 2, thereby potentially providing neuroprotection to the optic nerve. This article examines the results of the international, multicenter Phase 2/3 trial investigating the safety and efficacy of QPI-1007 in patients with acute-onset NAION.
Study Design: The QRK207 Trial
The trial was a rigorous, international, multicenter, double-masked, sham-controlled randomized study. It enrolled 725 participants who presented with acute unilateral NAION within 14 days of the onset of visual symptoms. This large sample size reflects the significant global effort to find a solution for this condition.
Intervention and Randomization
Participants were initially randomized in a 1:1:1:1:1 ratio into five distinct treatment groups. Following a preplanned interim analysis, the study focused on three primary groups: single or multiple intravitreal injections of QPI-1007 at doses of 1.5 mg or 3.0 mg, compared against a sham injection. The multidose regimen involved three bimonthly injections. This design allowed researchers to assess both the dose-response relationship and the potential benefit of sustained caspase 2 inhibition during the critical period of RGC vulnerability.
Endpoints and Objectives
The primary efficacy endpoint was the proportion of patients losing at least 15 Early Treatment Diabetic Retinopathy Study (ETDRS) letters of best-corrected visual acuity (BCVA) between day 1 and month 6. Secondary outcomes included the mean change in BCVA and mean change in visual field (VF) sensitivity, measured as mean deviation, over the same period. Safety was monitored through the frequency and severity of adverse events throughout the study duration.
Key Findings: A Complex Clinical Picture
The results of the trial present a nuanced picture of the potential for neuroprotection in NAION. While the study did not meet its primary endpoint across the entire participant population, specific subgroups showed statistically significant benefits.
Primary and Secondary Outcomes in the Total Population
At the 6-month mark, the data showed no significant difference in the proportion of participants who lost 15 letters or more of BCVA between the multidose QPI-1007 groups and the sham-controlled group. This result suggests that for the broad population of NAION patients, including those with relatively mild initial vision loss, the intervention did not provide a clear clinical advantage over the natural history of the disease.
Subgroup Analysis: Insights for Severe Vision Loss
A preplanned subanalysis provided a more encouraging perspective. In participants with a baseline BCVA of 60 letters or fewer (equivalent to Snellen 20/63 or worse), the administration of QPI-1007 showed a significant protective effect. In this subgroup, a significantly lower proportion of patients lost 10 letters of BCVA compared to the sham group. Specifically, the p-values were 0.045 for the 1.5 mg multidose group and 0.0104 for the 3.0 mg multidose group.
Furthermore, visual field sensitivity—a critical measure of functional vision in optic neuropathy—showed significant preservation in this same subgroup. The prevention of a 7-dB loss in visual field mean deviation was statistically significant (P = 0.023) in those with poorer baseline vision. This suggests that while the drug may not be necessary for those with mild ischemia, it may serve as a critical rescue therapy for those at risk of profound visual disability.
Safety Profile and Tolerability
From a safety standpoint, the trial was highly successful. Intravitreal injections of QPI-1007 were well tolerated. The frequency of adverse events was comparable across all groups, with the majority of reported issues being related to the injection procedure itself (such as subconjunctival hemorrhage or transient intraocular pressure elevation) rather than the siRNA molecule. No systemic safety signals were identified, confirming the localized nature of the treatment.
Expert Commentary: Interpreting the Data
The failure to meet the primary endpoint in the total population highlights the inherent challenges of conducting clinical trials for NAION. The natural history of NAION is variable; some patients experience spontaneous improvement, while others stabilize. This variability can dilute the observable effect of a therapeutic agent, particularly when mild cases are included. The “ceiling effect” in patients with high baseline visual acuity makes it difficult to demonstrate significant preservation of vision.
The subgroup findings are, however, clinically meaningful. Patients presenting with BCVA of 20/63 or worse represent a population at higher risk for permanent, lifestyle-altering vision loss. The fact that QPI-1007 showed a dose-dependent and statistically significant benefit in this group provides a path forward for future research. It underscores the importance of patient selection in neuroprotective trials—targeting those with the most to lose and the greatest potential for measurable benefit.
Mechanistically, the inhibition of caspase 2 remains a biologically plausible strategy. By interfering with the programmed cell death pathway, QPI-1007 aims to keep RGCs alive during the acute ischemic phase, providing a window for the optic nerve to recover from the initial metabolic shock. The trial proves that siRNA can be safely delivered to the vitreous and potentially influence the clinical course of an acute optic neuropathy.
Conclusion and Future Directions
The Phase 2/3 trial of QPI-1007 for NAION is a landmark study, representing one of the largest and most rigorous investigations into neuroprotection for this condition. Although the primary outcome for the general population was not met, the significant findings in the subgroup with poorer baseline vision offer a glimmer of hope for a condition that currently has no treatment.
The study highlights two critical takeaways for the medical community: first, that intravitreal siRNA is a safe and viable delivery platform for ocular neuroprotection; and second, that future trials should likely focus on patients with more severe baseline visual impairment to maximize the signal of efficacy. While QPI-1007 may not be a universal cure for NAION, it represents a significant step forward in our understanding of how to manage acute ischemic insults to the optic nerve.
References
Levin LA, Bhatti MT, Klier S, Morgenstern R, Szanto D, Miller NR, Kupersmith MJ; Quark NAION Study Group. A Randomized Sham-Controlled Phase 2/3 Trial of QPI-1007 for Acute Nonarteritic Anterior Ischemic Optic Neuropathy. Ophthalmology. 2026 Jan;133(1):62-74. doi: 10.1016/j.ophtha.2025.07.039. Epub 2025 Aug 14. PMID: 40816607.