Highlight
– In a randomized phase II trial (LUNAR, NCT05496959), neoadjuvant 177Lu-PNT2002 followed by SBRT significantly improved progression-free survival (PFS) versus SBRT alone for oligorecurrent hormone-sensitive prostate cancer (orHSPC): median PFS 17.6 vs 7.4 months (HR 0.37; P < .0001).
– Two cycles of 177Lu-PNT2002 (6.8 GBq per cycle, 2 weeks apart) given before SBRT did not produce a meaningful increase in grade ≥3 toxicity; grade 3 lymphopenia was the only reported higher-grade adverse event in small numbers.
– The study was single-center and phase II; findings are hypothesis-generating but suggest a potentially practice-altering combined local + targeted radioligand strategy for selected patients with PSMA-PET–defined oligorecurrence.
Background
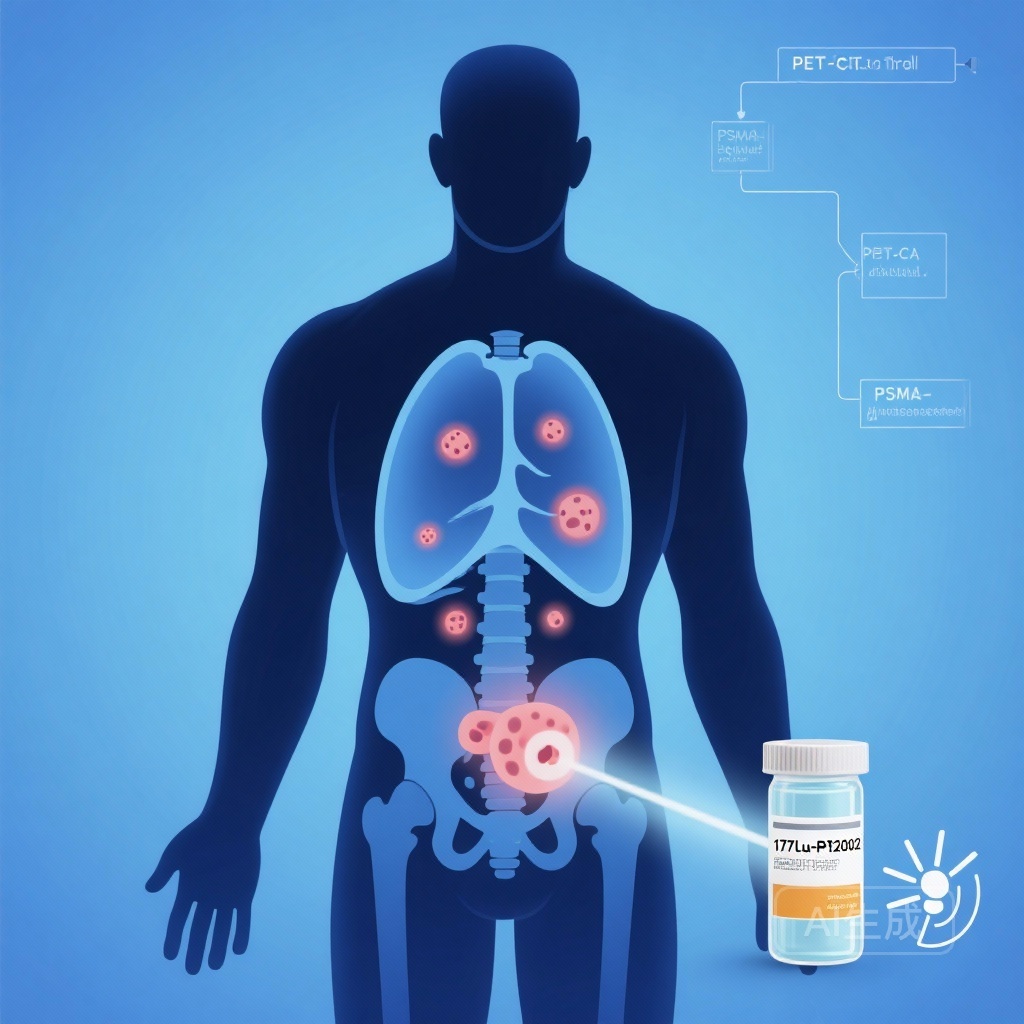
Oligorecurrent hormone-sensitive prostate cancer (orHSPC) — typically defined as recurrence with a limited number (commonly 1–5) of metastatic lesions — has become an increasingly recognized clinical state thanks to the widespread use of PSMA-targeted positron emission tomography/computed tomography (PSMA PET/CT). Metastasis-directed therapy (MDT), most commonly stereotactic body radiotherapy (SBRT), can delay systemic hormonal therapy and has shown benefit in selected patients. However, progression after MDT remains common, prompting investigation of combinatorial approaches that target both macroscopic and microscopic disease reservoirs.
Prostate-specific membrane antigen (PSMA)–targeted lutetium-177 (177Lu) radioligand therapy (RLT) delivers beta-emitting radiation selectively to PSMA-expressing cells and has shown meaningful clinical activity in later-line metastatic castration-resistant prostate cancer (mCRPC). Relying on PSMA PET to select patients, investigators have explored RLT in earlier disease states or in combination with local therapies to improve control of both visible and occult disease foci.
Study design
The LUNAR trial (Lutetium-Neoadjuvant to Stereotactic Ablative Radiotherapy) is a single-center, randomized, open-label, controlled phase II study conducted at UCLA (ClinicalTrials.gov NCT05496959). Key eligibility criteria were hormone-sensitive prostate cancer with oligorecurrence defined by 1–5 PSMA PET/CT–avid lesions. Patients were stratified by stage (N1/M1a vs M1b) and by lesion count (1 vs 2–3 vs 4–5) and randomized 1:1 to one of two arms:
- SBRT alone to all PSMA PET–identified lesions (control arm).
- Neoadjuvant 177Lu-PNT2002 (6.8 GBq per cycle, two cycles given 2 weeks apart) followed by SBRT to all lesions (experimental arm).
The primary endpoint was progression-free survival (PFS), defined as progression detected on PSMA PET/CT, initiation of salvage hormonal therapy, or death. PSMA PET/CT was obtained at prostate-specific antigen (PSA) progression and/or at 12 months after SBRT as part of systematic imaging follow-up. Analyses were performed in the intention-to-treat population.
Key findings
Between September 2, 2022, and November 9, 2023, 92 patients were randomized (47 to SBRT alone; 45 to 177Lu + SBRT). Eighty-seven patients were evaluable for analysis (42 in the SBRT arm; 45 in the combination arm). Median follow-up was 22 months.
Primary outcome: The addition of neoadjuvant 177Lu-PNT2002 to SBRT produced a statistically and clinically significant improvement in PFS. Median PFS was 17.6 months (95% CI, 15 months to not reached) in the 177Lu + SBRT arm versus 7.4 months (95% CI, 6.0 to 13.5 months) in the SBRT-alone arm. The hazard ratio (HR) for progression or death was 0.37 (95% CI, 0.22 to 0.61), P < .0001. This corresponds to a 63% relative reduction in the risk of progression or death over the observed follow-up.
Secondary and exploratory outcomes: The report notes identification of prognostic biomarkers for PFS; details were mentioned as exploratory and will require confirmatory analyses when the full dataset and biomarker methods are published. No data on overall survival (OS) mature in the initial report.
Safety: Toxicity was acceptable and comparable between arms. The only grade 3 adverse events reported were lymphopenia: two patients (4.8%) in the SBRT arm and three patients (6.7%) in the 177Lu + SBRT arm. No unexpected toxicities or treatment-related deaths were reported. Importantly, the addition of two cycles of 177Lu-PNT2002 did not translate into a clinically meaningful excess of high-grade adverse events in this cohort.
Clinical interpretation of effect size
A median PFS extension from 7.4 to 17.6 months is substantive in the orHSPC setting where the goal of MDT is often to postpone systemic therapy and prolong disease control with limited morbidity. The HR of 0.37 is large for a randomized phase II study and suggests a robust treatment effect. Because the primary endpoint incorporated PSMA PET/CT progression as well as biochemical progression and initiation of hormonal therapy, the finding reflects both radiographic and management-driven events.
Expert commentary and mechanistic rationale
Combining local ablative therapy with a systemic, lesion-targeted radiopharmaceutical has a compelling biological rationale. SBRT ablates macroscopic lesions with high-dose local radiation, addressing visible disease. Neoadjuvant 177Lu-PSMA RLT can deliver systemic targeted radiation to PSMA-expressing micrometastases and to the margins of known lesions, potentially sterilizing occult disease that would otherwise seed progression after focal therapy.
The LUNAR results resonate with the evolving paradigm in oligometastatic prostate cancer: blending precise imaging, focal ablative therapy, and systemic modalities tailored by molecular phenotype. The magnitude of PFS benefit observed here, if reproducible in larger, multicenter trials, could shift practice by offering a time-limited, targeted systemic therapy that augments the durability of MDT without the morbidity of continuous androgen deprivation.
Limitations and considerations
Several limitations temper immediate adoption into widespread practice:
- Single-center, open-label phase II design: potential for selection bias and center-specific expertise in PSMA PET interpretation and SBRT planning.
- Primary endpoint relied in part on PSMA PET imaging, which is highly sensitive; the clinical significance of small PSMA-avid foci detected after treatment requires contextualization with PSA kinetics and patient-centered outcomes.
- Follow-up is relatively short for evaluating late toxicities and overall survival; OS data are not yet available.
- Details of the prognostic biomarker analyses were not provided in the preliminary report; validation is required.
- Generalizability to centers without robust PSMA PET/CT infrastructure or experience with PSMA-targeted RLT may be limited.
Finally, the regimen used two cycles of 6.8 GBq 177Lu-PNT2002 given two weeks apart; whether different dosing schedules, additional cycles, or concurrent rather than neoadjuvant sequencing would alter efficacy or toxicity remains unanswered.
Implications for practice and future research
The LUNAR trial provides encouraging evidence that a short course of PSMA-targeted RLT administered before SBRT can double median PFS in selected patients with PSMA PET–defined oligorecurrent HSPC. Before changing standard practice, the findings should be confirmed in multicenter phase III studies with longer follow-up and prespecified patient-reported outcomes and overall survival endpoints.
Key questions for future trials include:
- Can the PFS benefit be replicated in a broader, multicenter population?
- Does neoadjuvant 177Lu-PSMA ultimately improve overall survival or quality of life versus SBRT alone or SBRT plus conventional systemic therapy?
- Which patients derive the most benefit — e.g., by lesion count, location (nodal vs bone), PSA kinetics, or molecular biomarkers?
- What is the optimal sequencing and number of 177Lu cycles when combined with MDT?
Given the favorable toxicity profile in LUNAR, future comparative trials could also assess patient-reported outcomes and time to initiation of long-term androgen deprivation therapy, outcomes highly relevant to patients weighing short-term combination therapy versus delayed systemic treatment.
Conclusion
The phase II LUNAR trial demonstrates that neoadjuvant 177Lu-PNT2002 followed by SBRT significantly prolonged progression-free survival compared with SBRT alone in patients with PSMA PET–defined oligorecurrent hormone-sensitive prostate cancer, without a meaningful increase in high-grade toxicity. The results are hypothesis-generating and merit confirmation in larger, multicenter randomized trials with longer follow-up and prespecified analyses of overall survival, quality of life, and biomarker-defined subgroups. If validated, this combined modality approach could change the therapeutic landscape for selected patients with oligorecurrent prostate cancer by offering more durable disease control while preserving quality of life.
Funding and clinicaltrials.gov
The LUNAR study was conducted at the University of California, Los Angeles. The trial is registered with ClinicalTrials.gov (identifier: NCT05496959). Funding sources were reported in the original publication; readers should consult the full JCO article for detailed funding and conflict-of-interest disclosures.
References
1. Kishan AU, Valle LF, Wilhalme H, et al. 177Lu-Prostate-Specific Membrane Antigen Neoadjuvant to Stereotactic Ablative Radiotherapy for Oligorecurrent Prostate Cancer (LUNAR): An Open-Label, Randomized, Controlled, Phase II Study. J Clin Oncol. 2025 Nov 12:JCO2501553. doi:10.1200/JCO-25-01553. Epub ahead of print. PMID: 41223345.
2. Sartor O, de Bono J, Chi KN, et al. Lutetium-177–PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med. 2021;385:1091–1103. doi:10.1056/NEJMoa2107322.
AI image prompt for thumbnail
A high-resolution medical-illustration: frontal view of a middle-aged man’s pelvis silhouette overlaid with a PET/CT image showing multiple bright PSMA-avid spots; a labeled vial reading ‘177Lu-PNT2002’ in the foreground and a stylized SBRT beam icon targeting lesions; clinical trial flow diagram faintly in the background; color palette in clinical blues and soft grays; clear, informative, and focused on targeted radiotherapy and advanced imaging.