Introduction
In the rapidly evolving landscape of assisted reproductive technology (ART), frozen embryo transfer (FET) has become a cornerstone of clinical practice. The strategy of freezing all embryos to avoid ovarian hyperstimulation syndrome (OHSS) or to allow for preimplantation genetic testing has shifted the focus toward optimizing endometrial preparation. Historically, clinicians have balanced two primary approaches: the natural ovulation regimen, which relies on the patient’s endogenous hormonal milieu, and the programmed regimen, which uses exogenous estrogen and progesterone to prepare the uterus. While both methods are widely utilized, emerging evidence has suggested that the hormonal environment at the time of implantation may have profound implications for obstetric and neonatal outcomes.
Highlights
- Healthy live birth rates are statistically equivalent between natural ovulation and programmed regimens (41.6% vs 40.6%).
- The natural ovulation regimen significantly reduces the risk of pre-eclampsia (2.9% vs 4.6%) and postpartum hemorrhage (2.0% vs 6.1%).
- The absence of a corpus luteum in programmed cycles is a suspected driver of adverse placental and vascular outcomes.
- Natural cycles carry a higher rate of cycle cancellation (16.2%) compared to programmed cycles (11.5%), primarily due to monitoring challenges.
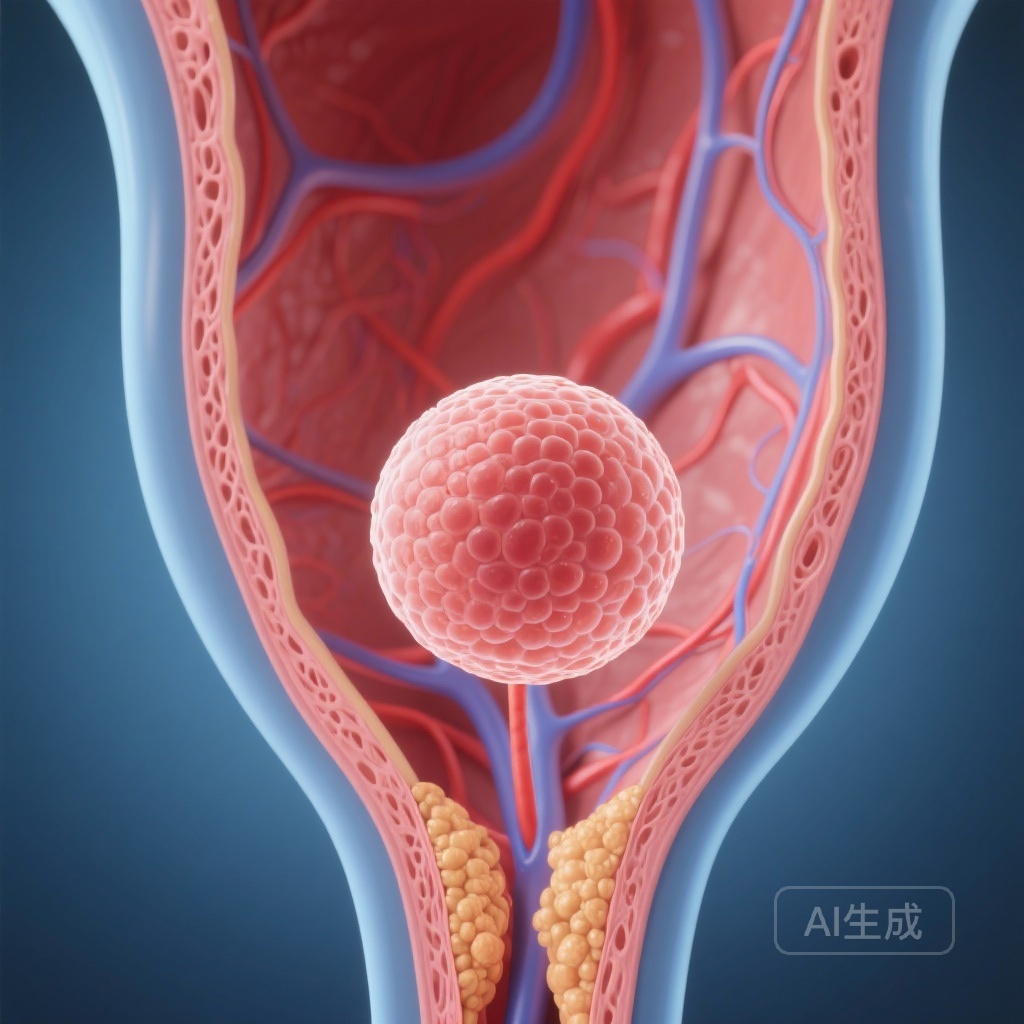
The Corpus Luteum Debate and Disease Burden
The programmed regimen (also known as the artificial cycle) is often preferred for its logistical convenience, as it allows for scheduled transfers and requires less intensive monitoring. However, a critical physiological difference exists: programmed cycles lack a corpus luteum (CL). In a natural cycle, the CL produces not only progesterone and estrogen but also various vasoactive substances, such as relaxin and prostanoids. These factors are believed to play a vital role in maternal circulatory adaptation and early placentation. The growing burden of hypertensive disorders of pregnancy in ART populations has led researchers to question whether the convenience of programmed cycles comes at the cost of maternal vascular health.
Study Design: The PnROVE Trial
The PnROVE study was a multicentre, randomised, parallel-group clinical trial conducted across 24 academic fertility centres in China. The trial enrolled 4,376 ovulatory women, aged 20 to 40 years, who were planning a single frozen blastocyst transfer. Participants were randomised 1:1 to either a natural ovulation regimen or a programmed regimen.
Intervention Protocols
In the natural ovulation group, endometrial preparation was guided by the patient’s natural cycle. Monitoring involved serial transvaginal ultrasounds to track follicle development and serum measurements of luteinising hormone (LH), oestradiol, and progesterone. The timing of the transfer was synchronized with the endogenous LH surge or ovulation. In the programmed regimen group, sequential administration of oral oestradiol followed by vaginal and/or intramuscular progesterone was used to achieve endometrial receptivity, completely bypassing the natural ovulatory process.
Primary and Secondary Endpoints
The study was uniquely powered to evaluate two primary outcomes: the chance of a healthy live birth (defined as a live birth of a singleton at term with normal birth weight and no major congenital anomalies) and the risk of pre-eclampsia or eclampsia. Secondary outcomes included pregnancy loss, placental accreta spectrum, caesarean section rates, and neonatal complications.
Key Findings: Efficacy and Safety Profiles
The results of the intention-to-treat analysis provided a clear picture of the trade-offs between the two regimens. Regarding efficacy, the study found no significant difference in the primary outcome of healthy live birth. Specifically, 41.6% of women in the natural ovulation group and 40.6% in the programmed group achieved a healthy live birth (Relative Ratio [RR] 1.03; 95% CI 0.96 to 1.10; P=0.49). This confirms that both methods are equally effective at achieving the fundamental goal of ART.
Maternal Safety and Obstetric Complications
The safety data, however, favored the natural ovulation regimen. Among patients who achieved clinical pregnancy, the risk of pre-eclampsia was significantly lower in the natural ovulation group (2.9%) compared to the programmed group (4.6%; RR 0.63; 95% CI 0.43 to 0.94; P=0.02). Even more striking were the differences in other maternal complications:
- Postpartum Haemorrhage: 2.0% in the natural group vs. 6.1% in the programmed group (RR 0.32).
- Placental Accreta Spectrum: 1.8% in the natural group vs. 3.6% in the programmed group (RR 0.51).
- Early Pregnancy Loss: 12.1% in the natural group vs. 15.2% in the programmed group (RR 0.80).
- Caesarean Section: 69.5% in the natural group vs. 75.6% in the programmed group (RR 0.92).
Cycle Logistics and Cancellation
While safer for the pregnancy, the natural ovulation regimen was more difficult to manage clinically. The rate of cycle cancellation was significantly higher in the natural group (16.2% vs. 11.5%, P<0.001). This was largely attributed to the failure to detect an LH surge, unexpected ovulation, or suboptimal endometrial thickening in the absence of exogenous stimulation.
Expert Commentary: Mechanistic Insights
The clinical findings of the PnROVE trial align with the “missing corpus luteum” hypothesis. Relaxin, a hormone secreted by the CL, is known to mediate systemic vasodilation and increase renal compliance during early pregnancy. In programmed cycles, the absolute lack of relaxin may lead to a failure of the maternal cardiovascular system to adapt to the increased volume of pregnancy, thereby predisposing the patient to hypertension and pre-eclampsia. Furthermore, the higher incidence of placental accreta and postpartum hemorrhage in the programmed group suggests that the artificial hormonal environment may subtly alter the depth and quality of trophoblast invasion and uterine remodeling.
Clinicians must now weigh the administrative ease of programmed cycles against the clear maternal health benefits of natural cycles. For ovulatory women, the natural cycle should arguably be the first-line recommendation. However, for women with irregular cycles or those who live far from the clinic, the programmed regimen remains a viable, albeit slightly higher-risk, alternative.
Conclusion
The PnROVE trial provides high-level evidence that for ovulatory women undergoing FET, a natural ovulation regimen is as effective as a programmed regimen in terms of live birth rates but offers a superior safety profile for the mother. By reducing the risks of pre-eclampsia, placental complications, and postpartum hemorrhage, the natural cycle aligns more closely with the goal of a healthy mother and a healthy baby. Future research should focus on whether modified natural cycles (using minimal stimulation) can reduce the cancellation rates observed in this study while maintaining the vascular benefits of the corpus luteum.
Funding and Registration
This trial was supported by the National Key Research and Development Program of China and the National Natural Science Foundation of China. It is registered at the Chinese Clinical Trial Registry (ChiCTR2200057990).
References
- Wei D, et al. Natural ovulation versus programmed regimens before frozen embryo transfer in ovulatory women: multicentre, randomised clinical trial. BMJ. 2026;392:e087045.
- von Versen-Höynck F, et al. Increased Risk of Preeclampsia After Frozen-Thawed Embryo Transfer in Programmed Cycles Without a Corpus Luteum. Hypertension. 2019;73(3):641-649.
- Ginström Ernstad E, et al. Neonatal and maternal outcomes after frozen embryo transfer: Increased risks in programmed cycles. American Journal of Obstetrics and Gynecology. 2019;221(2):126.e1-126.e18.