Introduction
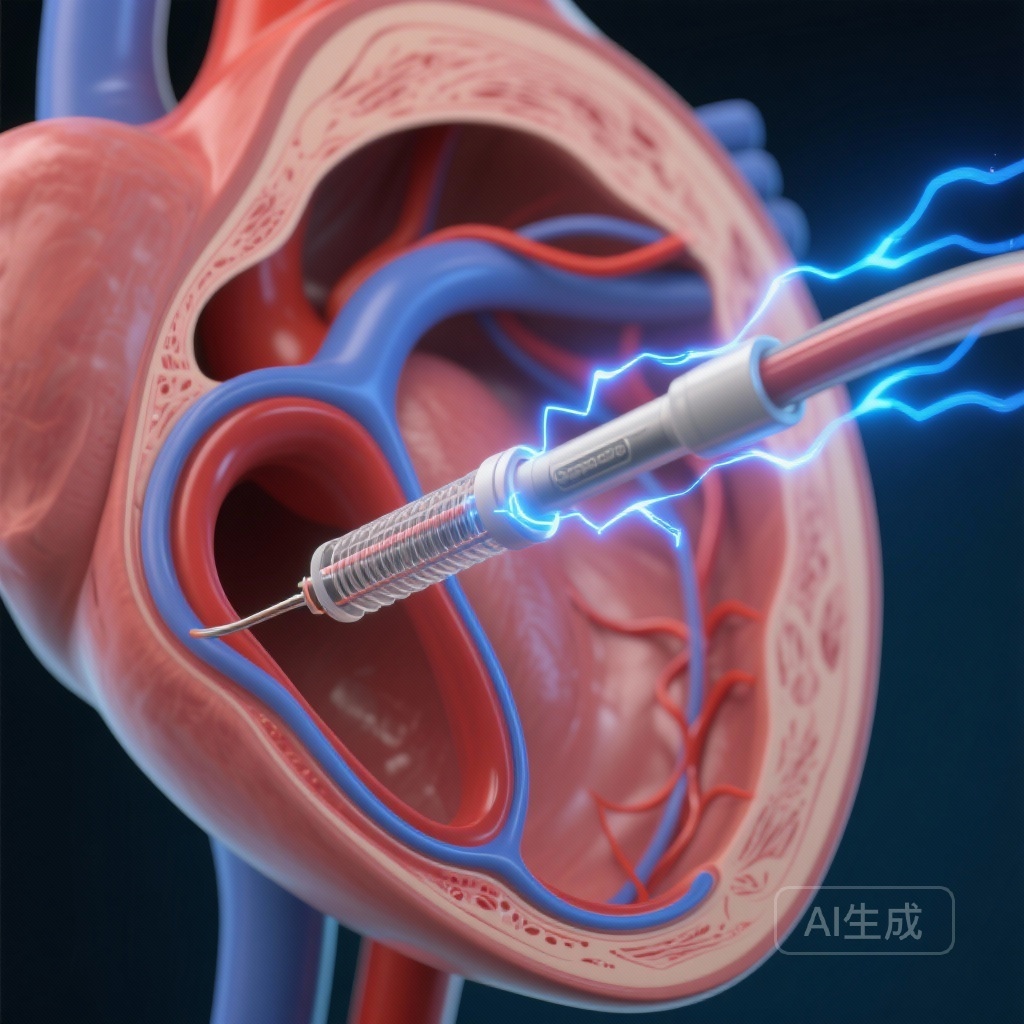
The landscape of catheter ablation for atrial fibrillation (AF) is undergoing a paradigm shift. For decades, thermal energy—primarily radiofrequency ablation (RFA) and cryoballoon ablation—has been the cornerstone of pulmonary vein isolation (PVI). However, thermal modalities carry inherent risks of collateral tissue damage, including esophageal injury, phrenic nerve palsy, and pulmonary vein stenosis, due to their non-selective nature. Pulsed field ablation (PFA), a non-thermal modality utilizing high-voltage, ultra-short electrical pulses to induce irreversible electroporation, has emerged as a promising alternative with high myocardial selectivity. The InsightPFA trial evaluates a next-generation iteration of this technology: nanosecond pulsed field ablation (nsPFA). By utilizing pulses in the nanosecond range rather than the microsecond range, this novel system aims to further refine the precision and efficiency of PVI.
Highlights
The InsightPFA trial provides several critical insights into the future of arrhythmia management:
Noninferior Efficacy
The primary efficacy endpoint of freedom from atrial tachyarrhythmia at 12 months was achieved in 65.5% of the nsPFA group compared to 64.1% in the AI-guided RFA group, successfully meeting the criteria for noninferiority.
Superior Efficiency
The nsPFA group demonstrated significantly shorter total procedure times, left atrial dwell times, and ablation times, highlighting the technology’s potential to increase laboratory throughput.
Safety and Sedation
The trial confirmed a comparable safety profile between nsPFA and RFA. Notably, over 89% of nsPFA procedures were performed under conscious sedation, proving the feasibility of this approach without requiring general anesthesia.
Background and Clinical Context
Catheter ablation is the preferred treatment for symptomatic paroxysmal AF refractory to antiarrhythmic drugs (AADs). While RFA guided by the Ablation Index (AI) has improved the durability of PVI, the procedure remains time-intensive and requires meticulous point-by-point application. The emergence of PFA has been heralded as a ‘safety-first’ revolution because the electrical threshold for cardiomyocyte death is lower than that of surrounding structures like the esophagus or phrenic nerve. The InsightPFA trial specifically investigated a novel biphasic nsPFA system (Insight Medtech), which uses ultra-short pulses to potentially minimize skeletal muscle contraction and improve the focus of the electric field.
Study Design and Methodology
The InsightPFA trial was a prospective, multicenter, randomized controlled trial conducted across 13 high-volume centers in China. A total of 287 patients with symptomatic paroxysmal AF were randomized in a 1:1 ratio to receive either nsPFA or AI-guided RFA.
Patient Population
Eligible participants were adults with documented paroxysmal AF who had failed at least one Class I or III antiarrhythmic drug. The mean age was approximately 60 years, with a standard distribution of comorbidities such as hypertension and mild structural heart disease.
Interventions
The nsPFA group utilized the LotosPFA catheter, a circular biphasic catheter designed for PVI. The RFA group utilized standard-of-care AI-guided catheters with contact force sensing. A notable feature of the study was the high utilization of conscious sedation (89.4% in nsPFA vs. 92.4% in RFA), reflecting real-world practice patterns in many regions.
Endpoints
The primary efficacy endpoint was freedom from documented atrial tachyarrhythmia (AF, atrial flutter, or atrial tachycardia) lasting longer than 30 seconds after a 3-month blanking period, without the use of Class I/III AADs. Safety endpoints included a composite of major adverse events such as death, stroke, TIA, atrioesophageal fistula, and phrenic nerve injury.
Key Findings and Results
The trial results underscore the maturity of nsPFA technology as a viable clinical tool.
Efficacy Outcomes
In the full analysis set, the primary efficacy endpoint was reached by 65.5% (93/141) of the nsPFA group and 64.1% (93/142) of the AI-guided RFA group. The adjusted rate difference of 2.0% (95% CI: -8.7% to 12.8%) met the predefined noninferiority margin (P = 0.0019). Kaplan-Meier estimates at 12 months showed success rates of 66.7% and 67.4%, respectively, with a hazard ratio of 0.99.
Procedural Efficiency
The most striking differences were observed in procedural metrics. The nsPFA group had significantly:
These findings suggest that nsPFA can substantially reduce the physiological stress on the patient and the physical demand on the operator.
Safety and Complications
Both groups achieved 100% acute procedural success (all pulmonary veins isolated). There were no significant differences in procedure-related adverse events. Importantly, no atrioesophageal fistulas or permanent phrenic nerve palsies were reported in either cohort.
The Fluoroscopy Paradox
Despite shorter procedure times, the nsPFA group experienced longer fluoroscopy times and higher radiation exposure compared to the RFA group. This is likely attributed to the circular nature of the PFA catheter, which may require more fluoroscopic guidance for positioning compared to the highly integrated 3D mapping used in point-by-point RFA.
Expert Commentary
The InsightPFA trial is a landmark study for several reasons. First, it validates the use of nanosecond pulses, which some researchers believe offer a cleaner electroporation profile with even less thermal byproduct than microsecond pulses. The high rate of conscious sedation is also a significant finding; many early PFA trials were criticized for requiring general anesthesia to manage the skeletal muscle contractions associated with high-voltage delivery. The Insight Medtech system appears to have mitigated this issue effectively.However, clinicians must consider the ‘fluoroscopy gap.’ As electrophysiology moves toward ‘zero-fluoro’ workflows using advanced 3D mapping, the reliance on fluoroscopy for PFA catheter positioning is a hurdle that must be addressed through better integration with electroanatomical mapping systems. Furthermore, the 12-month success rate of roughly 66% in both groups reminds us that while PFA is faster and safer, it has not yet drastically surpassed RFA in terms of long-term rhythm control for paroxysmal AF.
Conclusion
The InsightPFA trial successfully demonstrates that nanosecond pulsed field ablation is a safe, efficient, and noninferior alternative to traditional thermal radiofrequency ablation for patients with paroxysmal atrial fibrillation. Its ability to be performed under conscious sedation while significantly reducing procedure time makes it an attractive option for high-volume electrophysiology centers. Future iterations of the technology focusing on better 3D mapping integration will likely further enhance its clinical utility and reduce radiation exposure.
References
1. Lin W, Chu H, Wang C, et al. Pulsed Field Ablation Using a Novel Biphasic Catheter vs Thermal Ablation for Paroxysmal Atrial Fibrillation: InsightPFA Trial. J Am Coll Cardiol. 2025;86(23):2314-2326.
2. Reddy VY, Neuzil P, Koruth JS, et al. Pulsed Field Ablation for Pulmonary Vein Isolation in Atrial Fibrillation. J Am Coll Cardiol. 2019;74(3):315-326.
3. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the EACTS. Eur Heart J. 2021;42(5):373-498.