Introduction: The Evolution of Neuromodulation in Stroke Recovery
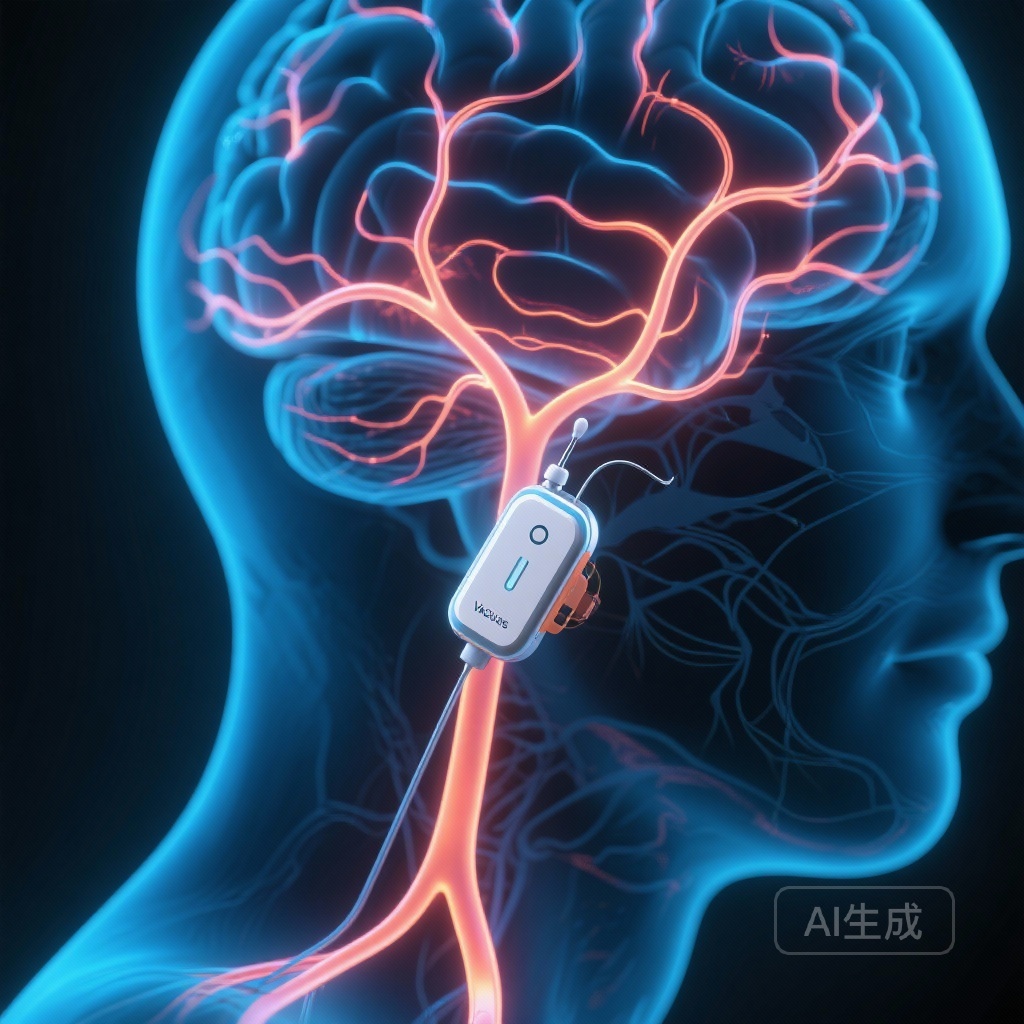
For decades, the management of chronic stroke has been primarily compensatory, focusing on adapting to permanent neurological deficits rather than reversing them. However, the emergence of neuromodulation, specifically vagus nerve stimulation (VNS), has shifted the paradigm toward active neurorehabilitation and the promotion of neuroplasticity. While the US Food and Drug Administration (FDA) recently approved the combination of task-oriented training and VNS for upper limb recovery, the hardware used in these interventions has remained largely unchanged for over a quarter of a century.
A recent study published in Stroke (2026) by Hays et al. introduces a significant technological leap: a miniaturized, closed-loop vagus nerve stimulation (CLV) system designed specifically for the needs of stroke survivors. This system not only simplifies the surgical approach but also enables a more personalized, data-driven rehabilitation experience. The results of their randomized, sham-controlled trial suggest that this next-generation device could be the key to unlocking lasting recovery in individuals living with the long-term effects of ischemic stroke.
Background: Addressing the Limitations of Conventional VNS
Conventional VNS systems, originally developed for epilepsy and depression, are relatively bulky and require complex implantation procedures. These legacy devices were not optimized for the ‘closed-loop’ requirements of stroke rehabilitation, where stimulation must be precisely timed to coincide with specific physical movements to reinforce neural circuits—a principle known as Hebbian plasticity.
The unmet medical need in this field was clear: a device that is smaller, easier to implant, and capable of seamless integration with rehabilitation sensors. The miniaturized system evaluated in this study is approximately 50-fold smaller than traditional pulse generators. This reduction in size is not merely an aesthetic improvement; it reduces the surgical footprint and potentially lowers the risk of site-related complications, making the therapy more accessible to a broader patient population.
Study Design: Precision Engineering Meets Clinical Rigor
The study was a randomized, sham-controlled trial conducted in Dallas, TX, involving 19 participants who had experienced an ischemic stroke at least one year prior to enrollment. All participants had residual upper limb deficits, a common and debilitating consequence of stroke that often limits independence and quality of life.
The trial was divided into two distinct phases. In the first phase, participants were randomized to receive 18 sessions of individualized, progressive rehabilitation paired with either active CLV or sham stimulation. This double-blinded phase was designed to isolate the effect of the stimulation from the effect of the physical therapy itself. Following this, all participants entered an open-label phase where they received an additional 18 sessions of active CLV therapy. To assess the long-term potential of the device, a subset of participants then transitioned to an exploratory extension involving up to 100 self-paced CLV sessions performed in the comfort of their own homes.
Key Findings: Safety and Functional Efficacy
Safety and Tolerability
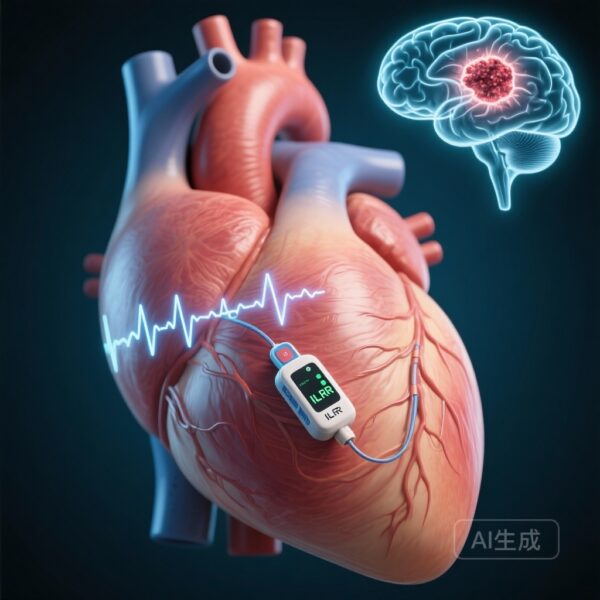
The primary outcome of the study focused on the safety and feasibility of the miniaturized system. The investigators reported that the nature and rate of adverse events were similar to or lower than those observed with conventional, larger VNS devices. Crucially, the closed-loop stimulation did not adversely affect autonomic functions such as heart rate or blood pressure, addressing a major concern in the use of autonomic neuromodulation. The simplified implantation process was successful across the cohort, proving the feasibility of the miniaturized hardware.
Functional Outcomes and the Fugl-Meyer Assessment
The secondary functional outcomes provided compelling evidence of the system’s effectiveness. The Fugl-Meyer Assessment for Upper Extremity (FMA-UE), a gold-standard metric for stroke recovery, was used to quantify improvements.
During the randomized controlled phase, participants receiving active CLV exhibited a significant improvement of 5.3±0.7 points over their baseline scores (P<0.001). In the context of chronic stroke, where functional plateaus are common, a 5-point gain is clinically meaningful and often translates to improved performance in activities of daily living.
Long-term Benefits in the Exploratory Home Extension
Perhaps the most striking finding came from the exploratory extension phase. Participants who engaged in additional self-paced CLV therapy at home saw their FMA-UE scores improve by an average of 10.9±1.3 points (P<0.001) compared to baseline. This suggests a dose-response relationship, where continued stimulation paired with repetitive movement leads to cumulative neurological gains. The ability to deliver this therapy in a home setting represents a major advancement in making intensive rehabilitation sustainable for patients.
Mechanistic Insights: Why CLV Works
The success of closed-loop VNS lies in its ability to trigger the release of neuromodulators, such as acetylcholine and norepinephrine, exactly when the brain is engaged in a motor task. By stimulating the vagus nerve during successful or attempted movements, the device reinforces the specific neural pathways associated with those movements. This ‘paired plasticity’ approach encourages the brain to reorganize itself, bypassing damaged areas and strengthening the remaining functional connections. The miniaturized system’s ability to interface with sensors ensures that the timing of this stimulation is precise, which is essential for maximizing the therapeutic effect.
Expert Commentary: A Shift Toward Patient-Centric Rehabilitation
Clinical experts in neurology and physical medicine view these results as a vital step toward ‘Rehabilitation 2.0.’ The transition from bulky, hospital-bound equipment to miniaturized, home-use technology addresses many of the barriers that currently prevent stroke survivors from receiving adequate therapy.
While the results are promising, it is important to note the study’s limitations, including the small sample size and the exploratory nature of the home-based extension. Further research is needed to determine the optimal ‘dose’ of stimulation and to identify which patient phenotypes are most likely to respond to CLV. However, the safety profile and significant functional gains observed here provide a strong foundation for larger, multicenter phase III trials.
Conclusion: The Path Toward Large-Scale Implementation
The miniaturized CLV system represents a paradigm shift in the treatment of chronic stroke. By combining cutting-edge biomedical engineering with established principles of neuroplasticity, this system offers a safe, feasible, and highly effective means of restoring upper limb function. The findings by Hays et al. underscore the potential for lasting recovery, even years after the initial stroke event. As the medical community moves toward more personalized and accessible healthcare solutions, miniaturized neuromodulation stands out as a beacon of hope for stroke survivors worldwide.
Funding and Clinical Trials
This research was supported by various grants and the clinical trial is registered at ClinicalTrials.gov under the unique identifier NCT04534556. The primary study was conducted between September 2021 and January 2024.
References
1. Hays SA, et al. Closed-Loop Vagus Nerve Stimulation Delivered With a Miniaturized System Produces Lasting Recovery in Individuals With Chronic Stroke. Stroke. 2026;57(1):38-49. doi:10.1161/STROKEAHA.125.052937.
2. Dawson J, et al. Vagus nerve stimulation paired with rehabilitation for upper limb function after ischaemic stroke (VNS-REHAB): a randomised, blinded, pivotal, device trial. The Lancet. 2021;397(10284):1545-1553.
3. Engineer ND, et al. Directing plasticity to understand and treat neurological disorders. Neuron. 2011;71(6):960-971.