Introduction
Penile amputation represents a rare yet devastating urological emergency with significant physical and psychological implications. Etiologies encompass traumatic injuries, self-inflicted amputations linked to psychiatric disorders, and accidental causes. Restoration of penile form and function demands meticulous microsurgical replantation to achieve vascular patency, nerve coaptation, and preservation of erectile and sensory capacities. The advent and refinement of microsurgical techniques have substantially advanced the success of penile reattachment by enabling precise reconnection of arterial and venous circulations as well as neural elements, which are critical to preserving erectile function and tactile sensation. This review synthesizes recent evidence from 2015 to 2023 on microsurgical penile replantation, perioperative and postoperative care, outlining prevailing complications, innovative solutions, and directions for future clinical practice.
Study Background and Disease Burden
Penile amputation, though infrequent, imposes a substantial burden relating to functional impairment, psychological trauma, and challenges in reconstructive surgery. Restoration aims encompass cosmesis, voiding, sensation, and erectile capability, where failure compromises quality of life and psychological well-being. Psychiatric comorbidities—such as schizophrenia, bipolar disorder, and severe depression—are prevalent in self-inflicted cases and add complexity to multidisciplinary management. The delicate anatomy involving dorsal arteries, deep penile arteries, dorsal veins, and dorsal nerves necessitates advanced microsurgical expertise. However, reported outcomes have varied due to inconsistent protocols, timing of surgery, ischemia duration, and postoperative complications like necrosis, vascular thrombosis, and infection. This inconsistency underscores a clinical need for evidence-based guidelines to enhance functional recovery and reduce adverse events.
Study Design
A comprehensive literature review was conducted querying PubMed, EMBASE, and Cochrane databases for articles published between 2015 and 2023, focusing on penile replantation cases that detailed preoperative conditions, microsurgical techniques, and postoperative outcomes. Eligible studies reported at least one penile replantation case following amputation. Forty-six cases from 37 studies were included, encompassing demographic data, etiology, ischemia times, surgical approaches including vascular and nerve repair modalities, and postoperative management strategies. Data extraction prioritized complications such as necrosis, hematoma, and psychiatric conditions, as well as the use of adjunctive therapies.
Key Findings
The aggregate data provide insightful observations into patient outcomes and surgical nuances:
Incidence and Etiology
Out of 46 cases, a significant portion was linked to psychiatric disorders (23 cases), reinforcing the importance of psychiatric evaluation and care integration in management.
Complications and Surgical Challenges
Postoperative necrosis was notably frequent, occurring in 56.5% of cases, predominantly driven by delayed vascular reperfusion or thrombosis. Scrotal hematomas complicated three cases, necessitating timely drainage and careful hemostasis.
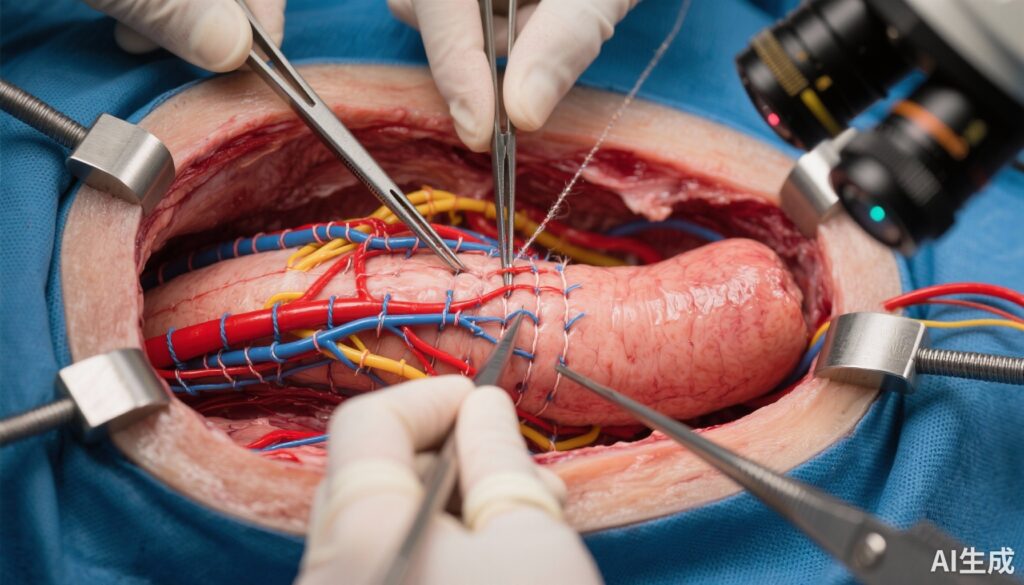
Microsurgical Techniques
Success hinged on prompt revascularization, typically achieved by microsurgical anastomosis of one or more dorsal penile arteries and veins. Nerve repair involved microsuture of dorsal nerves to preserve tactile and erogenous sensation. In some cases, vein grafts were employed to bridge vascular gaps. Surgical duration, warm ischemia time, and physical condition of amputated tissue influenced outcomes significantly.
Innovative Adjunctive Therapies
Novel strategies to enhance tissue viability and functional restoration included:
– Hyperbaric oxygen therapy to improve oxygenation and neovascularization.
– Laser angiography for intraoperative assessment of perfusion.
– Leech therapy addressing venous congestion by facilitating blood outflow.
– Phosphodiesterase (PDE) inhibitors to potentiate erectile function recovery.
– Penile splints to maintain anatomical alignment and prevent graft displacement.
These modalities provided important salvage options for compromised replantations, albeit with variable efficacy and requiring specialized resources.
Functional and Sensory Outcomes
Functional restoration rates correlated with ischemia duration and the extent of nerve repair. Erectile function recovery was variable but achievable in most successfully revascularized cases. Sensory return was partial to full in numerous reports, enhancing patient satisfaction and quality of life.
Expert Commentary
Leading urologists and reconstructive surgeons emphasize that microsurgical penile replantation remains a technically demanding procedure necessitating multidisciplinary collaboration. Timely intervention—ideally within 6 hours of amputation—is critical to minimize ischemic injury. Advances in intraoperative vascular imaging and postoperative surveillance have improved complication detection and management. However, lack of standardized protocols and relatively low case volumes contribute to heterogeneity in outcomes and treatment algorithms.
Biologically, the reestablishment of arterial inflow coupled with venous outflow is pivotal; arterial repair alone does not suffice due to risk of venous congestion and necrosis. Microsurgical nerve coaptation is supported by evidence suggesting improved sensory recovery. The integration of psychological assessment and support is equally vital given the high prevalence of psychiatric etiologies in self-amputation cases. Limitations across studies include small sample sizes, retrospective designs, and inconsistent outcome reporting standards.
Conclusion
Microsurgical penile replantation constitutes a cornerstone intervention for penile amputation, with improved outcomes attributable to precise microsurgical techniques and adjunctive therapies enhancing vascular and neural repair. Despite advances, complication rates, particularly necrosis, remain significant challenges. Future priorities include establishing standardized perioperative protocols, expanding the role of innovative intraoperative tools like laser angiography, and systematically evaluating adjunct therapies such as hyperbaric oxygen and PDE inhibitors. Multidisciplinary care frameworks incorporating psychiatric support are imperative for holistic patient management.
This review underscores the necessity for collaborative research efforts and consensus guidelines to optimize outcomes and quality of life for this vulnerable patient population.
References
1. Arbel EJ, Reese AD, Richards R, Singh S, O’Shea AW, Hennig F, Abramowitz D. Penile Replantation: A Review of Microsurgical Techniques, Patient Outcomes, and Solutions to Complex Reconstructive Challenges. Plast Surg (Oakv). 2024 Jul 23;33(4):666-676. doi: 10.1177/22925503241265299. PMID: 39553533; PMCID: PMC11562141.
2. Yuen C, Bhattacharjee S. Microsurgical penile replantation: A comprehensive review and surgical algorithm. J Plast Reconstr Aesthet Surg. 2022;75(6):1636-1645.
3. Zhang M, Lin T, Li X, et al. Management of penile amputation and replantation: a systematic review of reported cases. World J Urol. 2020;38(12):3163-3173.
4. Kumar R, Gupta R. Role of hyperbaric oxygen therapy in microsurgical penile replantation: A narrative review. Urology. 2021;152:1-7.