Highlights
- Endovascular recanalization (ER) plus medical treatment was associated with a nearly threefold increase in the risk of stroke or death compared to medical treatment alone (aHR 2.80).
- The primary risk associated with ER occurs within the first 30 days post-procedure, where the risk of stroke or death was over 20 times higher than in the medical group.
- Between 30 days and one year, there was no statistically significant difference in ischemic stroke rates between the two treatment cohorts.
- The findings suggest that procedure-related risks currently outweigh the potential long-term benefits of restoring blood flow in nonacute intracranial artery occlusions.
Introduction: The Clinical Challenge of Symptomatic Nonacute Intracranial Artery Occlusion
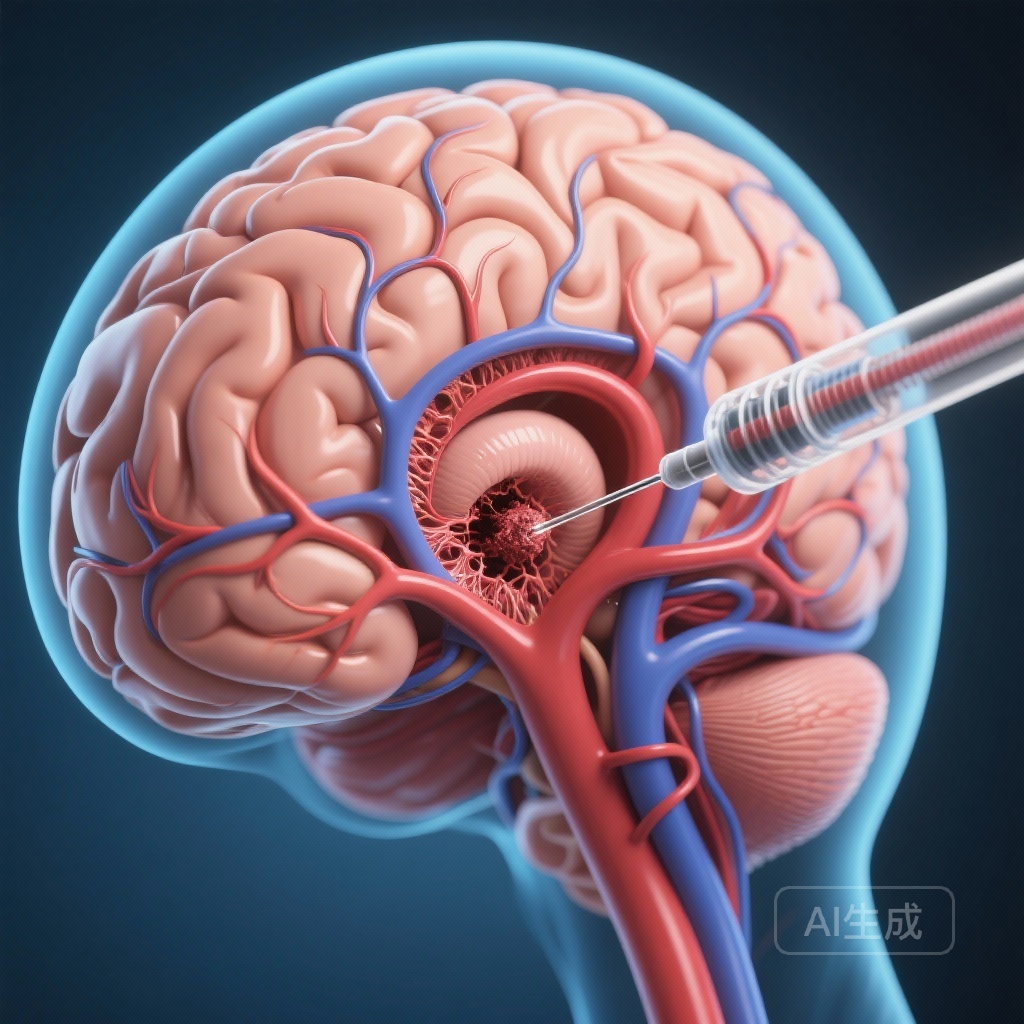
Management of symptomatic nonacute intracranial artery occlusion (sNAIAO) remains one of the most complex frontiers in neurovascular medicine. Unlike acute ischemic stroke, where endovascular therapy has become the gold standard for large vessel occlusion, the management of chronic or nonacute occlusions is fraught with uncertainty. Patients with sNAIAO often present with recurrent transient ischemic attacks (TIAs) or strokes despite standard medical therapy, indicating a failure of collateral circulation or hemodynamic instability. While the logic of restoring flow via endovascular recanalization (ER) is theoretically sound, the technical challenges and risks of navigating chronically occluded, often atherosclerotic vessels are substantial.
Previous landmark trials, such as SAMMPRIS and VISSIT, have demonstrated that aggressive medical management often outperforms stenting in the context of intracranial stenosis. However, the specific subset of patients with total nonacute occlusion—rather than just stenosis—has lacked high-quality, multicenter evidence to guide clinical decision-making. The ERNA-IAO study provides a critical evaluation of whether the addition of ER to medical therapy actually improves patient outcomes or simply introduces unnecessary procedural morbidity.
The ERNA-IAO Study: Methodological Rigor
The Endovascular Recanalization versus Medical Treatment Alone for Symptomatic Nonacute Intracranial Artery Occlusion (ERNA-IAO) study was a multicenter, prospective cohort study conducted at six comprehensive stroke centers in China. Between January 2020 and October 2023, the study enrolled 436 consecutive participants with sNAIAO. The cohort was divided into two groups: those receiving medical treatment alone (n=288) and those receiving ER plus medical treatment (n=148).
The primary outcome was a composite of any stroke or death within 30 days after enrollment, or ischemic stroke in the territory of the qualifying artery between 30 days and one year. This composite endpoint was designed to capture both the immediate procedural risks and the potential long-term protective benefits of successful recanalization. Researchers utilized Kaplan-Meier analysis and log-rank testing to assess differences, with hazard ratios adjusted for potential confounders.
Analyzing the Results: The High Price of Recanalization
The study results revealed a stark contrast between the two treatment strategies. The ER group experienced a significantly higher incidence of the primary outcome compared to the medical treatment group. Specifically, the adjusted hazard ratio (aHR) for the primary outcome was 2.80 (95% CI: 1.55, 5.08; P < .001). This indicates that patients undergoing the endovascular procedure were nearly three times as likely to suffer a major adverse event compared to those managed medically.
The 30-Day Critical Window
The most alarming finding was the disparity in early outcomes. Within the first 30 days of enrollment, the risk of stroke or death was exponentially higher in the ER group (aHR 21.74; 95% CI: 5.00, 95; P < .001). This suggests that the procedure itself carries an immense risk of periprocedural complications, such as vessel perforation, distal embolization, or hyperperfusion syndrome. In contrast, the medical treatment group remained remarkably stable during this initial period.
Long-Term Follow-Up: 30 Days to One Year
Proponents of ER often argue that while the initial risk is high, the long-term protection against recurrent stroke justifies the intervention. However, the ERNA-IAO data did not support this hypothesis. Between 30 days and one year post-enrollment, the incidence of ischemic stroke in the territory of the qualifying artery showed no significant difference between the groups (aHR 0.62; 95% CI: 0.24, 1.62; P = .33). While the hazard ratio numerically favored the ER group for late events, the difference failed to reach statistical significance and was insufficient to offset the high volume of early procedural complications.
Expert Commentary: Why Does Endovascular Recanalization Fail?
The failure of ER to show benefit in this study can be attributed to several pathophysiological and technical factors. Chronic intracranial occlusions are often characterized by hard, calcified plaques and long-segment occlusions. Attempting to cross these lesions with micro-wires and balloons carries a high risk of arterial dissection or rupture. Furthermore, the brain tissue distal to a chronic occlusion often adapts through collateral vessel formation; sudden restoration of high-pressure flow via recanalization can lead to hemorrhagic transformation or cerebral edema.
Clinicians must also consider the efficacy of modern medical therapy. With high-potency statins, dual antiplatelet therapy (DAPT), and rigorous blood pressure control, the natural history of sNAIAO may be more benign than previously thought. The ERNA-IAO study reinforces the notion that unless procedural safety can be drastically improved—perhaps through better patient selection using advanced perfusion imaging or more refined micro-catheter technologies—medical management should remain the frontline approach.
Conclusion and Future Directions
In patients with symptomatic nonacute intracranial artery occlusion, medical treatment alone is associated with superior clinical outcomes compared to endovascular recanalization plus medical treatment. The high rate of periprocedural stroke and death in the ER group serves as a cautionary tale for neuro-interventionists. While there may eventually be a niche for ER in patients who fail maximal medical therapy and demonstrate severe hemodynamic failure on perfusion imaging, such a subset has yet to be clearly defined by high-level evidence.
For now, the ERNA-IAO study provides a clear directive: the risks of endovascular recanalization for nonacute occlusions currently outweigh the benefits. Clinicians should prioritize optimizing medical regimens and only consider interventional options within the context of controlled clinical trials.
References
- Li L, Yan Z, Wu Q, et al. Endovascular Recanalization versus Medical Treatment Alone for Symptomatic Nonacute Intracranial Artery Occlusion: A Multicenter Cohort Study. Radiology. 2026;318(1):e251080.
- Chaudhary N, Wilseck J. Editorial: Rethinking Recanalization in Chronic Occlusions. Radiology. 2026;318(1).
- Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365(11):993-1003.
- Zaidat OO, Fitzsimmons BF, Woodward BK, et al. Effect of a balloon-expandable intracranial stent vs medical therapy on risk of stroke in patients with symptomatic intracranial stenosis: the VISSIT randomized clinical trial. JAMA. 2015;313(12):1240-1248.